Microsoft powerpoint - substance abuse and tbi bianh.pptx [read-only]

TBI and the Problem of Substance Abuse
Set Points of Drug Self Administration
– Impulse Control
– Reflection/Empathy
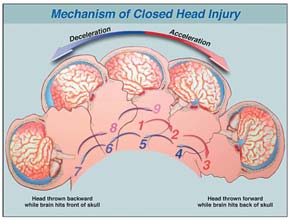
mTBI and complicated mTBI may also place
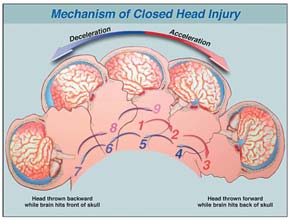
• Secondary Injury
– Delayed edema– Hydrocephalus– Drug interactions– Organ failure– Seizure activity
Focal deficits can occur
This occurs in the presence of a specific focal lesion usually due
to intraparenchymal bleeding in a specific area of the brain.
The interaction of the cognitive deficits and the physical
disability needs to be considered when planning rehabilitation
and long-term goals.
A patient with a focal lesion in the right parietal lobe will
display anosognosia (inability to appreciate his own illness).
An organic denial syndrome. Such patients have difficulty
understanding the purpose of various treatments and
Estimates indicate that 18.9 million adults in the
Cannabis is classified as a Schedule I substance
U.S. were diagnosed with substance abuse or
making it comparable to drugs such as heroin with
dependence in 2011, or approximately 8% of the
respect to legal penalties for use, possession and
Approximately 23.5 million Americans age 12 and
In 1969 84% of Americans were against legalization
older required intervention for substance use.
of marijuana and 12% in favor of it.
It is projected that disability caused by substance use
In 2011 46% of Americans are against legalization
disorders will surpass that caused by any other
and 50% in favor of legalization.
physical disease worldwide by 2020.
Diagnosed when it is determined that substance use
A major distinction between substance dependence
had led to significant recurrent negative
and substance abuse is the compulsive use of the
consequences in one or more of four domains over
substances with an inability to control their use,
the same 12-month period. These domains include:
despite realization that use causes negative
legal, interpersonal, work/school, hazardous
Substance dependence is diagnosed when substance
use persists despite leading to three or more recurrent negative cognitive, behavioral or physiological consequences over a 12-month period.
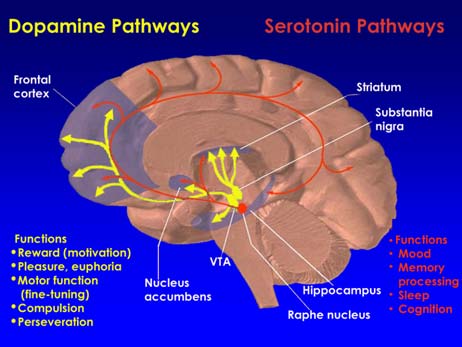
ASAM New Definition of Addiction
Addiction is a primary, chronic disease of brain reward, motivation, memory, and related circuitry. Dysfunction in these circuits leads to characteristic biological psychological social and spiritual manifestations. This is reflected in an individual pathologically pursuing reward and/or relief by substance use and other behaviors.

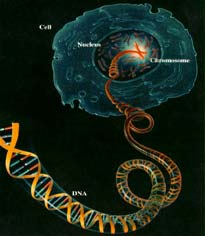
Factors Contributing to Vulnerability to Develop a Specific
Kreek (Rockefeller University) & Hassin
(Columbia P&S), 2004
Single Nucleotide Polymorphisms (SNPs) in Genes:
REWARD, COMFORT, AND PLEASURE from
ordinary activities; and a degree of calming to fight
SNP — a single
off unwanted stress. However, your genetics and
polymorphism, that is,
environment greatly affect this cascade; and
one nucleotide or base of
unfortunately, some of our genes come with
variations called polymorphisms. Polymorphisms
Allelic Frequency:
change the way the gene expresses itself. Most
people will call this a predisposition. These
1–5% intermediate
polymorphism's can alter their intended genetic
>5% high, frequent
Kreek (Rockefeller University) & Hassin
(Columbia P&S), 2004
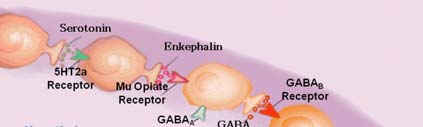
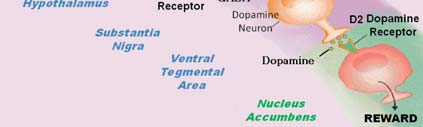
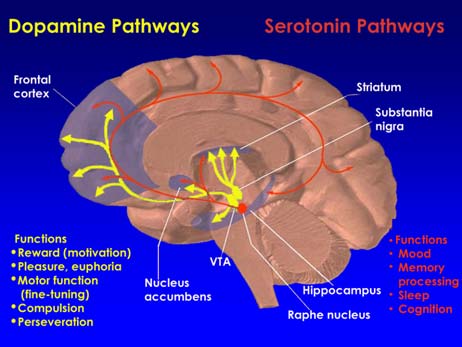
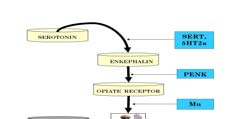
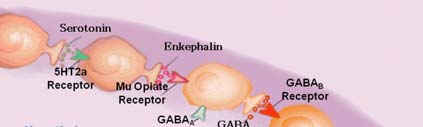
The Brain Reward Cascade
All Roads Lead to Dopamine
DA is used to signal novel and motivationally
relevant environmental events.
DA is also important for the motivation and
reinforcement of actions. Drugs that interfere with
DA transmission interfere with reinforcement
learning, while manipulations that enhance DA transmission, such as brain stimulation and addictive drugs, often act as reinforcers.
DA transmission is crucial for creating a state of
motivation to seek rewards.
>1/3 OF THE Total US Population Carries the DRD2 A1
(Over 100,000,000 people)
50% of African Americans carry the DRD2 A1 gene
58% of Hispanics carry the DRD2 A1 gene
72% of Asians carry the DRD2 A1 gene
85% of Native Americans carry the DRD2 A1 gene
Carriers of the DRD2 A1allele
at birth have a 74% chance of
becoming addicted to many Reward Deficiency Behaviors
Carriers of the DRD3 are
particularly sensitive to Cocaine
Carriers of the G allele of the mu –opiate receptor
have a very high risk for heroin seeking behavior.
With low function of the opiate receptor this will
There is evidence that these carriers
result in too much activity of the neurotransmitter
are at greater risk for all RDS
GABA which will prevent dopamine release from the neurons in the reward site of the brain (accumbens) .
behaviors including opioids and nicotine.
The result is increased cravings for drugs and food.
Carriers of the 3R allele of the MAO –A gene
Carriers of the 181 allele of GABAB3 gene
have increased metabolism of dopamine in the
have an altered function of GABA
cell at the energy producing mitochondria.
transmission leading to an augmented anxiety trait.
Having this allele causes an increased breakdown
of dopamine in the cell resulting in reduced
Carriers of this Allele may be prone to
dopamine in the storage sites and as such lower
alcoholism to reduce the anxiety level.
amounts of dopamine are released to combat stress as only one example.
Carriers have an inability to cope with
All RDS behaviors are at risk with this allele.
"Go" and "Stop" Switches
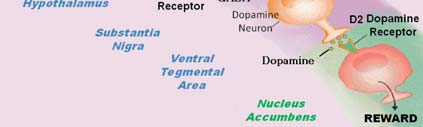
The area of the brain that encourages a human (or
Carriers of the COMT-G allele are at
any mammal) to perform or repeat an action that
high risk for all RDS behaviors because
promotes survival is called the survival/reinforcement circuit. Its normal function
this allele causes an enhanced
is to reinforce an action that promotes survival (e.g.
catabolism of dopamine in the synapse
eating, drinking, having sex). It is also the part of
after being released from the neuron at
the brain most affected by psychoactive drugs.
the reward site of the brain.
Technically, this circuit is referred to as the
mesolimbic dopaminergic reward pathway which is located in the old brain.
Role of the Pre-Frontal Cortical Regions in Drug Addiction
This survival/reinforcement circuit, located in the old
Pre-frontal cortical areas work in tandem with striatal
brain, acts as a "go" or "more" switch. At the heart of the
regions via corticostriatal networks that are modulated by
circuit is the Nucleus Accumbens Septi (NAc).
The Ventral Tegmental Area, lateral hypothalamus and
These include the dorsolateral PFC, which is involved in
amygdala also play important roles.
higher cognitive operations and decision-making; the OFC,
The control circuit, located mostly in the new brain, acts as
which is involved in salience attribution and goal-directed
a "stop" switch and is driven by the left orbital prefrontal
behaviors; and the anterior cingulate cortex, involved in
cortex. The stop switch works in conjunction with the
inhibitory control and awareness in addicted subjects could
fasciculus retroflexus and the lateral habenula, which
underlie the enhanced incentive motivational value of drugs
connect and communicate from the "Stop" switch to the
and the user's loss of control over drug intake.
"go" switch.
Memory, Psychoactive Drugs and Euphoric Recall
Old Brain – New Brain Distinction
When people use psychoactive drugs, memories of the
The old brain consists of: brainstem, cerebellum and
experience are imprinted on the brain: where they got the
mesocortex (mid brain), which contain the limbic
drug, the reason they used it, and what feelings (emotional
system (the emotional center).
and physical) resulted.
Regulating physiological functions of the body.
The stronger the drug, the more rapid the growth and
proliferation of memory "footprints" (dendritic spines) and
Experiencing basic emotions and cravings (e.g.
therefore the more deeply imprinted the memory.
anger, fear, hunger, thirst, lust, pain and pleasure).
The earlier in life a person begins using drugs or practices
Imprinting survival memories (e.g. that green plant
addictive behaviors, the longer and stronger the memories
tastes good, this bad odor signifies danger)
remain in the brain and the more likely the brain is to use the information from those memories to deal with events later in life.
Old Brain – New Brain
Old Brain – New Brain
The old brain responds to internal changes and
The old brain is the senior partner and the new brain
memories as well as to sensory inputs from external
is the young upstart.
Whenever the two brains are challenged by a crisis
When a person uses a psychoactive drug, most often
such as fear or anger, there is an automatic tendency
it is the old brain that remembers the experience and
to revert to the more established old-brain function.
how it felt.
And because the craving to use a psychoactive drug
almost always resides in the old brain, the desire for the pleasure, pain relief and excitement that drugs promise can be very powerful.
Old Brain – New Brain
Old Brain – New Brain
The new brain (neocortex) processes informaiton
Craving can override the new brain's rational arguments of
from the old brain, from different areas of the new
"too expensive" or "bad consequences" or "there's a
brain, and from the senses via the peripheral nervous
midterm tomorrow so don't party tonight."
The old brain acts four or five times more rapidly than the
new brain, so an action is usually well under way before
The new brain allows us to speak, reason, create,
common sense kicks in.
remember, make decisions and then act. The old
During intentional abstinence from a drug cravings are
brain simply reacts.
evoked by memory and emotions and a virtual tug of war between the old brain and the new brain occurs. There is a conscious desire to remain drug-free but the old brain seeks to resume drug use, mistaking the craving as a survival need.
Old Brain – New Brain
The old brain and the new brain carry out their
As humans develop they continue to learn to integrate the
functions by creating, storing and utilizing
drives of the old brain and the common sense of the new
memories. Even emotions and cravings depend on
brain. Some people, however, lose some of this ability due
memories. Some memories are stored on a
to genetic learning abnormalities, a chaotic or abusive childhood, brain injury, the use of psychoactive drugs and
conscious level (explicit memory) and some are
the practice of compulsive behaviors.
stored on an unconscious level (implicit memory).
Psychoactive drugs subvert the survival mechanism from
Storage, activation, and use of memories are at the
common sense integration of the new and old brains,
heart of the obsession to use drugs, which is one-half
resulting in the irrational behavior of addiction, which
of the addictive process.
relies on the "wants" of the old brain rather than the rational "needs" of the new brain.
The OFC has been shown to participate in outcomes
Impairments of the OFC and ACC are associated
related to primary reinforcers in both nonhuman and
with compulsive behaviors and impulsivity, and it
human studies. These neurons encode details
has also been postulated that impaired modulation
concerning the sensory properties of rewards, such
of these regions by DA might underlie the
as visual, olfactory and gustatory aspects, and the
compulsive and impulsive aspects of drug-taking and
size or timing of past or future rewards, as well as the
magnitude of more abstract rewards and penalties.
Impaired self-control plays a fundamental role in
drug-taking behaviors in addiction. Successful self-regulation functions require top-down control from the PFC to the striatal and limbic regions involved with rewards and emotions.
Impaired self-control in addicted people is believed to
Thus, dysregulated activity of the OFC could underlie
reflect disrupted prefrontal regulation of striatal regions.
both the impulsive choices for immediate rewards
The level of impairment is influenced by the emotional
and compulsive drug taking when the drug-induced
state (negative mood increases impairment) and the
DA increases may be profoundly attenuated in
context (exposure to unexpected cues can also impair it).
addicted people. This loss of control might continue
Damage to the OFC also interferes with the inhibition of
even when drug-taking has become less rewarding or
responding to formerly rewarding cues that are no longer reinforcing, thus favoring the emergence of perseverative
when adverse consequences far outweigh the
behaviors even when these are no longer reinforcing
psychological or physiological benefits of drug-taking.
Substance Abuse and TBI
Substance Abuse and TBI
History of TBI is frequent among individuals receiving
There is strong evidence that intoxication at the time of
treatment for alcohol and substance use disorders
injury is related to acute complications, longer hospital
The relationship between alcohol abuse and TBI is complex
stays, and poorer discharge status.
and probably circular
Alcohol abuse prior to TBI has consistently been found to
Adolescents who drink regularly were twice as likely to
mediate outcome from TBI.
sustain a TBI compared with adolescents who had never
Corrigan (1995) documented that a history of substance
used alcohol.
abuse is related to a wide range of outcomes, including
Initial alcohol-related TBI sustained after age 12 were
higher mortality rates, poorer neuropsychological
associated with a four-fold increased risk of repeat TBI by
functioning, increased chance of repeated injury, late
deterioration and worse functional outcome.
Substance Abuse and TBI
Substance Abuse and TBI
Intoxication and a history of premorbid alcohol use
Pre-injury history of alcohol abuse also appears to
are related to worsening injury severity indicators
exacerbate the effects of TBI on brain structure and
and early medical outcomes.
Patient's with +BALs on hospital admission have
TBI patients with a history of alcohol abuse
lower levels of consciousness when admitted, longer
demonstrated greater volumes of intracranial
duration of coma, and longer lengths of
TBI patients with a history of alcohol abuse also have
Post-traumatic amnesia and loss of consciousness
more pronounced local brain atrophy over time
were significantly longer in groups of patients with
compared to non-drinkers.
pre-injury alcohol abuse.
Substance Abuse and TBI
Mechanisms of Behavior Change
TBI sustained in people with a history of alcohol
Current evidence-based treatments for alcohol and
intoxication at the time of the injury demonstrated worse
drug-use disorders vary in theoretical foundations,
cognitive outcomes than those with negative toxicology
approaches and presumed mechanisms of action.
screens, with particular difficulty on tests of verbal intelligence, verbal memory and attention and
Yet, it remains a conundrum that these treatments
are often equally effective across clients who differ
Harmful or hazardous alcohol use in the 12 months prior to
substantially in neurocognitive impairment and
TBI was associated with poorer verbal learning and
other distinguishing features such as age, disorder
memory and slowed processing speed.
severity, and co-occurring psychopathology
Previous alcohol abuse increases the risk for development
of mood disorders following TBI
Mechanisms of Behavior Change
Mechanisms of Behavior Change
Several putative mechanisms of behavior change in
Key Question: Do the direct effects of
addiction treatments that have received relatively
alcohol/drugs on the brain, or neurocognitive
consistent support for enhancing treatment success
problems due to co-occurring TBI, and metabolic
include the clients motivation for behavioral change,
and nutritional disturbances have down-stream
the alliance between the treatment provider and the
effects on addiction treatment processes and thereby
client, the client's perceived self-efficacy to resist
alter substance-use-related treatment outcomes,
urges to use alcohol/drugs, and social support
and/or psychosocial adaptation more generally?
networks that support and encourage abstinence goals.
Mechanisms of Behavior Change
Mechanisms of Behavior Change
Some of the most potentially disruptive effects of
Deficits in prospective memory functioning may
psychoactive substances on the brain are that they
contribute to problems encountered in everyday
compromise the structure and function of the
living both during and after addiction treatment
prefrontal cortex, which results in substantial
Thus, neuropsychological impairment may
impairment to central executive control and
contribute to the failure to regulate drinking and
drug-taking behaviors in the moment, thereby
Memory impairment is also prevalent in addiction
escalating the risk for relapse, and over the long term
populations. This includes prospective memory
may contribute to the maintenance of substance-use
functioning, which refers to the memory needed to
behaviors, even in the face of severe, negative
plan and carry out future actions and involves
consequences of such use.
integrated memory and executive functions.
Mechanisms of Behavior Change
Mechanism of Behavior Change
Clinically, neuropsychological impairments have
In addition, in both alcohol- and drug-use-disordered
been associated with reduced treatment retention
clients, neuropsychological impairment interacted with
and compliance, self-efficacy to resist urges to use
self-efficacy to resist urges to use, such that a relatively
alcohol/drugs, coping-skill development and other
higher level of self-efficacy was a less robust indicator of successful substance use outcomes in impaired clients
prognostic indicators of addiction treatment
compared to those without neuropsychological impairment.
This finding suggests that mechanisms of behavior change,
In a large study of alcohol-use-disordered clients,
such as perceptions of self-efficacy to resist urges to use
impairment led to less treatment compliance and
alcohol and drugs, operate differently, or are perceived or
lower self-efficacy to resist urges to use alcohol,
reported less accurately in impaired clients.
which in turn predicted less successful outcomes following treatment.
Recap: Scope of the problem of
Mechanisms of Behavior Change
TBI and Substance Abuse
Greater involvement in A.A. has been observed in impaired
compared to unimpaired clients, suggesting that social
20% to 30% of persons with TBI show alcohol intox-
support for abstinence might be particularly useful to
ication at hospitalization, minimal data on other drugs.
bolster treatment effectiveness in cognitively impaired
50% to 60% of adolescents and adults in acute
rehabilitation have prior histories of substance abuse.
More severe executive and verbal impairment at treatment
entry predicted better substance-use outcomes in
Indices of brain structure and function suggest an
outpatients who had frequent contact with a social network
additive effect of substance abuse and TBI.
that supported abstinence, while impairment predicted
Substance abuse is associated with unemployment,
poorer substance-use outcomes in clients with more severe
living alone, criminal activity, lower subjective well-
alcohol-use histories who had frequent contact with a social
network that encourage drinking.
Need for assistance controlling use going unmet.
Vulnerable brain structures
Neocortex (especially the frontal lobes)
Limbic system (especially the hippocampus and
Decreased neuron density in the frontal cortex
Comorbid conditions:
15-23% of cortical neurons are selectively lost from the frontal
Malnutrition, diseases of the liver and the cardiovascular
association cortex following chronic alcohol consumption
After four weeks of abstinence there is a partial reversal of brain
shrinkage and some recovery of metabolic functions in the frontal
Head injury, encephalopathy
lobes and cerebellum
Psychiatric conditions and the use of medicines and other
Frontal lobe blood flow continues to increase with abstinence
returning to normal levels within four years
Cognitive deficits
Relapse leads to resumption of shrinkage, continued declines in
metabolism and cognitive function and evidence of neuronal cell
Impaired reasoning
Impaired Learning (poor semantic encoding)
Impaired Visuoperceptual processing
Wenicke's Encephalopathy
Interact with a specific binding site in the CNS—Gamma-
aminobutyric acid (GABA) receptor complex
GABA is the dominant inhibitory neurotransmitter of the
CNS and is the most wide spread neurotransmitter released at 30% of all synapses and helps to shape, integrate and refine the information conveyed by excitatory neurotransmission
GABA tends to act like a "brake" on the brain, with too
much transmission causing the individual to become drowsy and sedated, and too little making the individual become anxious and over excited.
Tolerance to the various actions of
Neuropsychological impact
benzodiazepines does not develop at the same rate.
Across 12 areas of cognitive assessment all long-term Benzo
For example, tolerance to the hypnotic effects can
users were impaired while using (Barker et al., 2004)
develop rapidly while tolerance to the anxiolytic
All 12 areas improved with withdrawal
effects tends to develop more slowly
11 areas of cognitive assessment were impaired as compared to
normal controls 6 months after withdrawal
Discontinuance should occur gradually
Discontinuance syndrome: rebound, recurrence
Areas of long-term impairment
Heavy use of cocaine is associated with alterations
Verbal Memory
of neurotransmitter systems in humans.
Psychomotor speed
Speed of processing
These alterations can manifest as abnormalities in
Motor control/performance
regional cerebral blood flow and cerebral glucose
Working memory
metabolism in the prefrontal cortex and in other
limbic areas, which in turn provide the substrates
General Intelligence
for neurobehavioral effects (depression,
compulsive behavior, cognitive deficits)
Nonverbal memory
Problem-solving
Verbal reasoning
Brain and Cocaine
Neuropsychological Sequelae
Greater errors of commission on sustained attention tasks
Attentional response speed is impaired
Vigilance impairments
Verbal learning/memory—shallow learning curves
Poor immediate and delayed recall
Poor working memory
Poor response inhibition
Cognitive switching impairments
Cocaine and Brain Hemorrhage
Cocaine-induced neurological abnormalities such as
Prefrontal brain regions, including the OFC, ACC,
atrophy and/or cell death as a results of ischemic
DLPFC and amygdala are activated during
events, can also manifest as neuropsychological
intoxication, craving and binging and deactivated
during withdrawal.
Vulnerable brain areas include: Orbitofrontal cortex,
These same brain areas are also involved in critical
anterior cingulate cortex, the dorsolateral prefrontal
behaviors such as decision-making, control and
cortex, amygdala, putamen and cerebellum.
inhibition of inappropriate responses, conflict monitoring and evaluation of the saliency of a stimuli or reward.
Based upon this brain-behavior relationship, Goldstein &
Based on this logic, the heavy use of cocaine,
Volkow (2002) have proposed that cocaine addiction is a
because of repeated ischemic events due to its
syndrome of impaired response inhibition and salience
vasoconstrictive properties, might have caused a
attribution. This model conceptualizes addiction as a dysregulation of cognitive and emotional processes that
state comparable to what is observed with lacunar
results in overvaluing of drug reinforcers, the undervaluing
infarcts in the white matter of the brain. This
of alternative reinforcers and difficulty with the inhibitory
might in turn, cause neurological states akin to
cognitive control that culminates as an inability to abstain
deconnection syndromes between regions within
from drug taking.
Cocaine and Alcohol
Neurocognitive deficits associated with cocaine use
Many heavy cocaine users also use other substances,
appear to be dose-related and persistent for at least 6
including alcohol.
months of abstinence. Heavy cocaine use = 4
Most studies have found that the interaction of cocaine
and alcohol is associated with greater neuropsychological impairment.
Deficits in executive function, spatial processing,
memory, concentration and motor function.
The cognitive domains most affected were short- and
long-term memory and visuomotor functions
Neuroimaging studies demonstrate additional reductions
in rCBF are observed when alcohol and cocaine were used
The mechanism is the formation of the highly toxic
Methamphetamine (cell loss)
Methamphetamine use produces long-lasting and negative
changes in brain structure and function.
Meth use is associated with an increased risk for
experiencing intracrainal hemorrhage
Meth use is associated with an increased risk for CVA for
the following reasons: increased bp, vasculitis, toxic effects on the cerebral vasculature and cardiac abnormalities.
In a recent study 19/21 meth using subjects had
Frequency of Impairment by Neuropsychological
Neuropsychological deficits are demonstrated for
at least 1 year after cessation.
Frontal activation is reduced (fMRI)
Impaired learning and memory
Impaired fluency
Impaired psychomotor speed
Impaired processing speed during decision making
Reduced dopamine and serotonin activity in
Hypoperfusion in several brain areas including the
frontal and parietal lobes.
A decrease in neurofilament (NF-L) proteins
Hypoperfusion in abstinent (4 months) abusers
in the frontal cortex. These proteins are thought to be involved in axonal transport and
Psychiatric comorbidity moderated these findings
neuronal morphology, suggesting that
such that hypoperfusion in the right frontal and
decreases in NF-L may be associated with
left temporal lobes occurred with depression and
functional impairment, particularly executive
in the right frontal lobe only in those with
functions and other functions associated with
antisocial personality disorder
the frontal cortex.
Methadone Maintenance Patients performed worse
Mintzer & Stitzer (2002) found MMP to be impaired
than normal controls on tests of psychomotor
on psychomotor speed, working memory, decision-
performance, information processing, attention,
making and meta-memory.
short-term memory, long-term memory and
A separate study in which the MMP group was
problem-solving. Difficult to generalize from this
divided into smokers and nonsmokers found that the
study since 67% reported a history of head injury
MMP smokers were more impaired than controls
(Darke et al. 2000)
and MMPI nonsmokers.
MDMA is a compound with properties common
A pronounced MDMA-induced denervation
to both the central stimulants and the
has been visualized throughout the neocortex,
striatum and thalamus, while lesser damage in
Difficulty to predict the behavioral effects of
the hippocampus, hypothalamus and basal
Usually taken intermittently
MDMA depletes 5-HT.
Not as reinforcing as cocaine or meth
Neuropsychological deficits in
Does not produce frank hallucinations
attention/concentration, learning/memory, motor/psychomotor speed and executive functioning.
During 2003 in the U.S. alone, 97 million people
over the age of 12 reported using cannabis.
Cannabis use in the US is most prevalent among
adolescents and young adults between the ages of 15 and 29.
Cannabis use produces a wide range of acute effects,
Cannabis research increased dramatically following
including changes in mood, mental status, and
the discovery of the cannabinoid receptor CB1.
perception as well as promotes physiological
The CB receptors are in the family of G-protein-
alterations (e.g. analgesia, neuroprotection and
coupled receptors. Such proteins are involved in
decreased intraocular pressure, body temperature,
second messenger signaling, and modulate chemical
inflammation, and neuronal excitability).
reactions inside cells.
Acute subjective sensations commonly include
The highest concentration of CB receptors are in the
sedation/relaxation, euphoria, depersonalization,
basal ganglia, cerebellum, hippocampus and
happiness/laughter and increased sensory
perception or subtle perceptual distortions.
Naturally occurring ligands in the brain:
Acute intoxication is associated with hypotension,
paranoid thinking, anxiety, panic attacks,
Arachidonic acid (an essential fatty acid found in cell
unpleasant feelings of depersonalization, and
membranes and the brain)
Less frequent adverse reactions include: anxiety,
Neurocognitive Effects of cannabis:
depression, paranoia, panic symptoms, panic
Acute Effects
reactions or psychotic symptoms.
Working memory difficulty
These less frequent adverse reactions are most often
Learning and recent memory (immediate recall)
experienced by naïve users.
Sustained Attention
Reduced motivation
Residual Effects
Mostly apply to heavy and recent users. After 4 weeks no
Neuropsychological Sequelae
0-6 hours after use
Deficits in psychomotor coordination
There are a number of OTC drugs that when used
Deficits in selective and sustained attention
improperly can create euphoria at a similar level as
Deficits in speed of information processing
illicit drugs of abuse.
Deficits in learning and memory
Deficits in inhibition and executive functions
Ether (Diethyl Ether)
Diethyl Ether, more commonly just called Ether, is
mainly used medically, as an anesthetic. However, it also has a long history of recreational use. In the late nineteenth century, it was used regularly in Ireland, Russia, France, Norway, the United States and elsewhere. The effect of ether was similar to alcohol, but it was cheaper, and allowed someone to sober up quicker, making it popular among those who didn't have much money.
Recreationally, DXM can have very powerful
effects, ranging from euphoria, elevated mood, dissociation, dream-like states, and increased awareness. Some other effects which may or may not be considered good, depending on the person, include disorientation, confusion, altered perception of time, decreased sexual functioning, and hallucinations. Higher doses can greatly impair memory, language and judgment. Using this drug is often referred to as "robo-tripping".
Unisom (Doyxlamine)
Teenagers will abuse Doxylamine for its
hallucinogenic properties, but it also makes them agitated and confused. It actually doesn't sound exactly like a very fun high, but people try all kinds of stupid things. In large doses, it can be quite dangerous, resulting in prolonged agitation, seizures, and the occasional coma.
Tramadol (opiate receptor agonist)
Tramadol enjoys a very unique legal status. While it
is considered a prescription drug, it is not federally scheduled, and has only been scheduled in a few US states. What this means is that, while one is supposed to have a prescription to purchase Tramadol, it is perfectly legal to posses the drug without a prescription in most of the United States.
Kava is an herb that comes from the Pacific Islands,
where the islanders have been using it medicinally
for a very long time. Kava has recently developed
some popularity in the Western world, where it is
still very legal to buy and use. While low-to-
moderate doses of Kava give one a sense of euphoria,
relaxation, or general well-being, higher doses can
cause hallucinations. It is also believed by scientists
that chronic use can cause yellow skin discoloration,
drowsiness, ataxia, liver damage, and malnutrition,
none of which sound very fun at all.
Kratom (Mitragyna Speciosa)
Kratom, referred to in scientific literature as Mitragyna
Speciosa, is a plant native to Southeast Asia. This plant is
from the same family as coffee, and is often used
medicinally to relieve pain. However, it has gained recent
popularity in the United States for its psychoactive
properties. It is currently unregulated, and can easily be
bought at online or at certain "herbal supplement" stores.
The powder or leaves are usually ingested in a tea-like
preparation, or smoked; sometimes it is also ingested
orally. A few grams of this substance can give someone a
high for two to three hours. While it was originally used
medicinally, it has been banned in its native Thailand,
due to the abuse of the plant. Watch out, this plant is
considered highly addictive.
Diphenhydramine usually goes by the trade name
Benadryl; it is marketed to deal mainly
with allergies, but is also often used as a sedative
when people are having trouble sleeping. It has
some popularity among recreational drug users, due
to its affect as a deliriant. When recreational users
take a high dose, they can expect such symptoms as
drowsiness, fatigue, disturbed coordination,
dizziness, blurred vision, confusion, and
hallucinations, which are somehow considered
positive things by recreational users.
Dimenhydrinate is a drug that most of you probably
know as Dramamine, and is mainly used to combat
motion sickness. It is also a deliriant, and is popular
among recreational drug users for the audio and
visual hallucinations that it provides in high doses.
Setting it apart from its cousin Diphenhydramine, it
is reported to also have a euphoric effect, along with
the hallucinations. It is not only abused by
recreational users, but also by psychiatric patients,
though in their case it is for self-treating anxiety and
the like, not for recreation.
Propylhexedrine is the active drug in a nasal spray
called Benzedrex, and it originally replaced amphetamine sulfate as the active ingredient years back due to abuse. Unfortunately, Propylhexedrine is also capable of abuse. Recreational users have been known to use some sort of extraction process to gain crystals from it, and it has hence earned the nickname "stove top speed," due to the effect that it has on people.
Afrin (Oxymetazoline)
Oxymetazoline is a drug used in a widely-used
commercial nasal spray called Afrin. It does not have a particularly strong high, and is instead more likely to cause psychosis in those who use it, some of whom have reported recurring hallucinations. What makes this drug noteworthy is just how addicting it is. Doctors have found that those hooked on it simply cannot function without the drug.
4 Quadrant Model of Service Provision
Quadrant III
Quadrant IV
Collaboration in the
Integrated Treatment
Integrated Treatment
of Traumatic Brain Injury and
Quadrant I
Quadrant II
Acute Medical Settings
Collaboration in
Rehabilitation Programs
Acquired Brain Injury
4 Quadrant Model of Service Provision
Integrated Treatment of TBI and SA
Case Management to change the
Quadrant III
Quadrant IV
Collaboration in the
Integrated Treatment
organize the team
Substance abuse treatment
to establish new attitudes,
Integrated
Collaborative Care
beliefs and skills
Quadrant I
Quadrant II
Acute Medical Settings
Collaboration in
Rehabilitation Programs
Screening & Referral
Collaborative Care
Rehabilitation toimprove functionalabilities
Acquired Brain Injury
Integrated Treatment of TBI and SA
Integrated Treatment of TBI and SA
Unique challenge for persons with TBI:
Establishing a therapeutic alliance is more difficult
with clients who are ego-centric, or otherwise lack
insight into others' thoughts and feelings.
Professionals will need greater commitment to and
experience with this population, as well as flexibility engaging them in treatment.
Programmatic options: specialized caseloads, smaller
caseloads, greater counselor freedom to customize procedures, consistency in personnel from engagement through treatment completion.
Integrated Treatment of TBI and SA
Integrated Treatment of TBI and SA
Unique challenge for persons with TBI:
Having multiple therapeutic alliances can lead to
inconsistencies, if not confusion.
Professionals need to communicate with each
other, optimally with the client included.
Programmatic options: joint treatment planning
and progress review and agency flexibility in allowing staff participation with "ad hoc" teams.
Integrated Treatment of TBI and SA
Integrated Treatment of TBI and SA
Unique challenge for persons with TBI:
Substance abuse treatment
to establish new attitudes,
Substance abuse services are not cognitively and
beliefs and skills
Substance abuse providers need to be able to identify
and treat clients with unique learning or communication
styles; be able to appreciate both neurobehavioral and
motivational sources of behavior; and understand the
unique presentation of traumatic brain injury.
Rehabilitation to improve functional abilities
Programmatic options: in-service and pre-service
training, staff sharing, reduce barriers to consultation,
allow more flexibility in program structure.
Integrated Treatment of TBI and SA
Integrated Treatment of TBI and SA
Case Management to change the environment and
Unique challenge for persons with TBI:
organize the team
Substance abuse treatment
Rehabilitation professionals have biased views
to establish new attitudes,
and, thus, expectations about persons with substance
beliefs and skills
Rehabilitation professionals need current and
accurate information about the nature and extent of
addictions, as well as their treatment. They need to
increase their knowledge and comfort level so that they
can address these issues and clients more objectively.
Rehabilitation toimprove functionalabilities
Programmatic options: in-service and pre-service
training, staff sharing, reduce barriers to consultation.
Integrated Treatment of TBI and SA
Integrated Treatment of TBI and SA
Case Management to change the
Unique challenge for persons with TBI:
Case management requires the time to develop a
organize the team
Substance abuse treatment
strong therapeutic relationship and address multiple
to establish new attitudes,
access and resource needs, while taking responsibility for
beliefs and skills
the coordination of all the providers involved.
Case managers need smaller caseloads, the capability to
engage via outreach, and longer allowable lengths of stay.
Changing the environment requires knowledge of health,
behavioral health, social service and vocational systems, as well as cooperation from these provider communities.
Rehabilitation toimprove functional
Programmatic options: skilled staff, specialized
caseloads, smaller caseloads, flexibility structuring treatment.
Making Services More Responsive
• Initiate cross-training, facilitate consultation and
explore staff-sharing options.
• Promote staff participation in "ad hoc" teams.
Actively Using and Uninterested in Treatment
Impulsively Using and Interested in Changing
• Take advantage of specialized caseloads.
Regularly Using and Interested in Changing
• Allow smaller caseloads and maximize consistency of
Not using and fearful of relapse
personnel throughout treatment.
• Provide case management services that can engage and
be effective with this population.
• Attract the most skilled staff to the most demanding
roles, and empower them.
Substance Abuse Assessment
Assessing substance abuse
Mostly males between the ages of 18 & 50.
History taking
Most were substance users prior to TBI
Medical Issues
Most have ongoing emotional disability
Specifics regarding substance use
Most have executive function impairment and/or memory
Understanding the implications of specific drugs (e.g. MDMA).
Understanding the circumstances of use
Most have slowed information processing
Assessing Neuropsychological Status
Taking Neuropsychological status into account when
Slowed Processing Speed
planning treatment
Decreased Attention Span/Immediate recall
Cognitive demands of treatment
Word Finding Difficulty
Cognitive demands of living sober/drug free
Retrieval Difficulty
Executive Function Difficulty
Slowed processing = increased stress and
demand in voc. Rehab
Assessing Readiness for Change
Word finding difficulty = decreased elaboration
Process of Change Model
Poor retrieval = loss of didactic information
Formal Assessment
Executive difficulty = poor self-cueing,
Change Ladders
difficulty with reflection, empathy and planning
Executive difficulty = poor impulse control,
failure to learn from negative experience, poor guidance.
Psychological Assessment
Assessing Emotional Status
Diagnostic Interview
Shaped by the Assessment results
Counseling Principles
Formal testing
Personality Assessment Inventory
Detailed Assessment of Posttraumatic Stress
Avoid Arguments
Point out discrepancies
Reduce barriers
Provide choice
Initiating Treatment
Making Modifications
Formal Treatment approaches must be understood well
Over 100 models of counseling
enough that modifications can be made.
Even Self-Help approaches may need modifications
Modifications are necessary
Psychotherapy and Cognitive Impairment
Initiating Treatment
The combination of diffuse deficits (e.g. slow
The first step is to identify the sensory-perceptual,
processing) and focal cognitive deficits (e.g.
attentional, linguistic, memory and reasoning or
impaired verbal attention) requires flexibility
planning deficits that could prevent the delivery of
throughout the psychotherapy process.
effective psychological treatment.
The scope and nature of psychological services for
These deficits represent the most basic level of
the TBI/SA patient should stem from continual
potential obstacles for the therapist.
appraisal, understanding and responsiveness on
The integration of cognitive rehabilitation may be
the part of the therapist
For successful psychological intervention, a patient
Early in treatment, the therapist should establish a
must be able to attend to and understand verbal
contract or predefined set of rules for refocusing the
material or therapeutic dialogue as it unfolds within
discussion if a session becomes derailed due to the
patient's inattention or decreased self-monitoring
The therapist and the patient should agree on a
Strategies to assist a patient in staying focused may
prompt or cue phrase, such as "Let's get back on
track," to regain focus
At the outset of each session, the therapist should
The patient's risk of becoming lost also can be
present a limited number of topics or themes to be
reduced if the therapist pauses frequently while
covered in the session; providing a patient with a
presenting therapeutic material or during
written list of these topics strengthens this strategy.
dialogue to allow the patient to mentally review
The patient will find it easier to retain the topical
the previous 5 min of the session.
thread of a discussion if the therapist avoids long,
complex sentences and dialogue
It is difficult to achieve a cumulative effect if memory
Working Memory: the limited, temporary store
deficits prohibit a patient from retaining the
where new information is held while it is
conclusions, insights or context of even a single
manipulated in a meaningful way to solve a current
Three aspects of memory dysfunction are germane to
the success of psychotherapeutic intervention:
Long-term memory: Memories formed over a longer
working memory, long-term memory and meta-
period of time from minutes to days or longer
Working Memory
Frequently rehearsing verbal information
Grouping similar psychotherapeutic topics or goals
Meta-memory: self-monitoring of one's own
Regulate the rate at which verbal information is presented
memory (e.g. remembering to remember)
Long-term Memory
Instruct the patient in ways to use symbolism
Help the patient to recognize and monitor his/her own
Teach the client ways to generate visual images
limitations. Such an awareness motivates the patient to
Use of mnemonic strategies
learn and use compensatory strategies and devices, the most critical of which is the memory notebook.
The memory notebook fosters organization and provides
a method for rehearsal of treatment information. Can be coupled with an alarm device found on a digital wristwatch.
In view of the highly verbal nature of psychotherapy
Language deficits derived from right hemisphere
for substance abuse language deficits can seriously
damage can be overlooked but are critical since
diminish its effectiveness.
nonverbal aspects of language contribute
Direct consultation with a speech/language specialist can be
significantly to overall comprehension.
very helpful.
Journaling can be helpful for patients with motor based
language difficulty
Patients manifesting deficits in motivation, initiation
The significance of current behavioral problems
of behavior, abstract reasoning, insight, planning,
should be emphasized to help the patient see the
problem solving or impulse control can present the
importance of productive therapeutic work.
most challenging situations.
Discussing the impact of negative behaviors on family
Structure, goal, and action-based therapeutic strategies are
members or a significant other can increase the patient's
motivation for treatment.
When motivation for treatment is compromised by
Modeling of desired behavior is important
decreased awareness or insight that a problem
Combining modeling and videotape technology
exists, the use of video technology makes abstract
shows objective and salient examples of behaviors
issues of therapy more salient for the patient.
to be targeted for treatment
Videotaping group setting reveals issues related to social
Additional structuring and rule setting within the
interaction that a TBI survivor might not have recognized
context of therapy may be required for patients
just from the subtle reactions of people in natural social situations
who have sustained orbital frontal damage and therefore, experience increased impulsivity and reduced self-regulatory capacities.
Awareness and Denial
Information Level
Diminished insight and awareness of self are common
Problems perceiving information about their disorders and can
sequelae of TBI and other neurological illnesses
even be completely unaware of any impairment (anosagnosia)
Three levels of awareness are: Information, Implication and
Difficulty understanding medical information and material
related to the diagnosed condition also is classified as reduced awareness at the information level
Implication Level
To effectively treat an individual with a
When patient's perceive information but are incapable of
neurological condition that affects self-awareness
appreciating the implications or long-term consequences
of their conditions, deficits, or life situations.
it is critical to clarify the etiology of the awareness
Integration Level
Patient accurately perceives their condition and are
Interventions will vary
aware of the implications but are unable to absorb
emotionally the gravity or meaning of their situation.
Defense mechanisms such as denial may appear when
deficits of awareness occur at the integration level.
Concent.
Pain, Addiction and TBI
Impairment Impairment Impairment
Complex population
The issues related to substance abuse and TBI treatment are similar for
Verbal Cues tion, notes,
behavioral pain management
Addiction related to pain management may be better perceived as
"pseudo-addiction" in most cases
Is chronic pain a type of brain injury?
Peri-aquaductal gray
Prefrontal cortex
Nonverbal & written
Parietal Lobes
Pain and Brain
Pain and Addiction
30-50% of chronic pain patients experience cognitive
fMRI studies indicate 30% reduction of cell volume
in the parietal lobes of chronic pain patients
Specialized programs for people with both chronic
pain and addiction are currently being developed
Interesting new treatments for chronic pain are
being developed that is responding to neuromatrixtheory of chronic pain (e.g. Scrambler Therapy)
Allen & Woods, Eds (2014). Neuropsychological aspects of substance
use disorders. Oxford University Press
Corrigan, J., Smith-Knapp, K. & Granger, C. (1998). Outcomes in the
first five years after traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 79, 298-305.
Sparadeo, F. & Gill, D. (1989). Effects of prior alcohol use on head
injury recovery. Journal of Head Trauma Rehabilitation.
Sparadeo, F. and Barth, J. & Stout, C. (1992). Addiction and traumatic
brain injury. In C.E Stout, J.L. Levitt & D.H. Ruben (Eds.), Handbook for assessing and treating addictive disorders (pp. 237-251). New York: Greenwood Press.
Sparadeo, F. and D'Amato, S. (2014). Scrambler Therapy: Effective
use of artificial neurons in the treatment of chronic neuropathic pain.
Journal of Nurse Life Care Planning, 14, (4). 14-27. New York.
Source: http://www.bianh.org/pdf/SubstanceAbuseTBI.pdf
NIH Public AccessAuthor ManuscriptProg Polym Sci. Author manuscript; available in PMC 2009 June 19. NIH-PA Author Manuscript Published in final edited form as: Prog Polym Sci. 2007 ; 32(8-9): 991–1007. doi:10.1016/j.progpolymsci.2007.05.013. Silk as a Biomaterial Charu Vepari and David L. KaplanDepartments of Chemical & Biological Engineering and Biomedical Engineering, Tufts University,4 Colby St, Room 153, Medford, MA 02155, Tel: 617-627-3251, Fax: 617-627-3231, Email:[email protected]
Volume 2 Spring 2007 REAP THE BENEFITS OF LOWERING LDL CHOLESTEROL BELOW 70 Over 50 percent of the U.S. population have cholesterol levels that are considered New patient enrollment to be too high. High blood cholesterol, also called hypercholesterolemia, is known tosignificantly lead to heart disease and stroke. Sometimes, no matter how much a person controls their diet, weight, exercise and medical conditions, it just isn'tenough.