Idi.mak.ac.ug



"CALL ATIC ON TOLL FREE NUMBER : 0800200055 FOR FREE ADVICE ON PATIENT MANGEMENT. YOU CAN ALSO BEEP OR SMS ATIC ON 0717326500
VOLUME : 8
JUNE 2011
Quarterly Newsletter of the AIDS Treatment Information Centre, Infectious Diseases Institute, Makerere University, Kampala
Case Report: Skin Reaction to Tenofovir
By Dr. Gyaviira Makanga (Mmed Int.Med) & Dr. Stella Zawedde - Muyanja (MBChB)
A 30 year old female presented to a local HIV Care Centre in Kam-
nevirapine dose was then escalated to 200mg BD, which she toler-
pala, Uganda for Routine Counsel ing and Testing for HIV after her ated well for the next 2 months with a rise in CD4 to 487 cells/µl husband had tested HIV positive from another centre. She had no after 3 months on ART. The Nevirapine dosing was then escalated major complaints apart from a history of heavy menses, no prior ma-
to 400mg OD. (once daily dosing of nevirapine has been found to
jor opportunistic infections and physical exam was unremarkable.
have ARV efficacy similar to twice daily nevirapine and is recom-mended for treatment simplification)
She underwent routine pre and post-test counselling and was found HIV positive on two rapid HIV tests i.e. determine and statpak Three days after the new dose, she reported back to the clinic with a respectively. She was initiated on cotrimoxazole prophylaxis and generalised itchy maculo-papular rash involving the oral mucosa as ferrous sulphate 200mg three times a day. Her baseline labs were smal blisters. Al her medications were stopped including cotrimox-as below;
azole. She reported no herbal remedies used prior to the rash. No repeat laboratory tests were done. She improved within 2 weeks and
was re-started on TRUVADA®/efavirenz. One day after medication,
developed another generalised erythematous itchy maculo-papular
rash but no mucosal involvement. The ART was stopped, with clear-
ance of the rash within 4 days.
One week later, was re-initiated on TRUVADA® and ALUVIA®.
One day after this new medication, developed another generalised
itchy macula-papular rash with mucosal involvement, she stopped her medication and reported back to the clinic.
NB: The above are the basic initial laboratory tests done by the clinic, viral load, Hepatitis B and C tests are not routinely done Further consultation with colleagues at the AIDS Treatment Infor-due to cost.
mation Centre (ATIC) located at the Infectious Diseases Institute, Makerere University; Kampala suggested the offending drug could
Based on her CD4 cell count (<350), she underwent three pre-anti be tenofovir. A TRUVADA® switch was therefore suggested. retroviral therapy (ART) counselling sessions with the counselling team as per the Centre/Current ART guidelines and was initiated on One week later, she was counselled and re-initiated on AZT/3TC ART 2 months from time of first presentation.
(COMBIVIR®) plus ALUVIA® and cotrimoxazole was restarted. She did well on this new regimen with no further complication. She
She was started on tenofovir/emtricitabine (TRUVADA®) plus ne-
has continued to do well to-date with no further skin or mucosal
virapine 200mg OD for 14 days, with no major adverse effects. Her adverse reactions.
continues on Pg 2
INSIDE THIS ISSUE :
Skin Tuberculosis
Ethambutol Associated
Filarial Diseases


Dr. Natalie Prevatt Coordinator; African Short Course in
A typical day in the life of a healthcare worker will often find
Tropical Medicine, London School of Hygiene and Tropical Medicine & Hospital for Tropical Diseases, UK
them dealing with a rather wide range of health related issues, some similar and others unique to particular patients.
Dr. Philip Gothard Consultant Physician, Hospital forTropical Diseases, Mortimer Market Centre, Capper Street,
This edition of the ATIC Newsletter reflects the life of a health
London WC1E 6JB, UK .
worker that has to read up on different issues as they deal with different patients.
Dr. Tom Doherty London School of Hygiene and Tropical Medicine & Hospital for Tropical Diseases, UK
When most of us think of skin reactions to ARVs, Nevirapine and Efavirenz are the drugs that come to mind. In this article, we share with you a unusual case from Nsambya Home Care
Editorial Committee
HIV Clinic about a patient who got a skin reaction to Tenofovir.
We also share with you another interesting Case Report from the Infectious Diseases Institute on Skin Tuberculosis.
Ceppie Merry HIV Physician and Pharmacologist, TrinityCollege Dublin and Infectious Diseases Institute
Over the past months, a number of you have called ATIC with
Prof. Walter Schlech Dalhouise University, Canada
queries on how to manage patients with suspected Ethambutol
Prof. Allan Ronald University of Manitoba, Canada
toxicity and so we present you an article on Ethambutol asso-ciated Optic Neuritis in patients treated for Tuberculosis. We
Mairin Ryan HIV Pharmacist and Pharmacoeconomist, IMB
trust this will give you more information on the issue.
Kim Scarsi HIV Clinical Pharmacist, Northwestern MemorialHospital, Chicago
Our special collaboration with the London School of Hygiene
Charles Steinberg Consultant Training Department, Infectious
and Tropical Medicine continues in this edition with more arti-
Diseases Institute
cles on the Neglected Tropical Diseases. This time, we bring you an article on the Buruli Ulcer, and another on Filarial diseases.
Leah Thayer Head of Training Department,Infectious Diseases Institute
Please read on and learn from the different experiences and
Sheila Karamagi ATIC Research and Communications
information we have specially packaged for you.
Monica Amuha Grace ATIC – Pharmacist
Sheila Karamagi – ATIC Research and Communications
Stella Zawedde-Muyanja ATIC – Medical Officer & Team leader
Skin and subcutaneous reactions i.e. urticaria, vesiculobul ous
rash, pustular rash, maculopapular rash, pruritus and skin discol-
oration are seen in one to ten out of 100 people taking Truvada. It
is therefore plausible that the patient improved after discontinu-
ation of Tenofovir.
Although the culprit drug was later found to be Tenofovir, we
should stress that NVP should be used with caution in women with
CD4 cell counts above 250 due to increased risk of hepatotoxic-
ty and that when a maculopapular rash occurs on NVP, patients
Discussion :
should also be assessed for hepatotoxicity as the two adverse drug
Although hypersensitivity skin reactions in HIV infected people are reactions tend to occur together.
more commonly at ributed to cotrimoxazole and Non-Nucleoside
Reverse Transcriptase Inhibitors ( NNRTIs), they can also be caused *Case is from a patient attending Nsambya Home Care HIV clinic*
by Nucleoside/Nucleotide Reverse Transcriptase Inhibitors (NRTIs/
NtRTI), although with much less frequency. 15-27% of patients * The programme this patient was enrolled in uses the WHO 2010
receiving EFV and 17% of patients receiving NVP develop a rash cut off point of 350 to initiate patients on ART*
compared to 9% of patients receiving CBV+3TC.
References
• Once daily dosing of NVP versus twice daily dosing of NVP. Journal of
The possibility of an NRTI or NtRTI causing a maculopapaular rash
Antimicrobial Chemotherapy 2008 61( 1) 13-16
should be suspected if a rash does not resolve with discontinuation • www.medicines.ie : Truvada : Summary of Product Characteristics of cotrimoxazole and the NNRTI component of an ART regimen.
• Medical Management of HIV Infection: Drug information: Nevirapine
and Efavirenz


Skin Tuberculosis: A Case Report
John Mark Bwanika1 ; Esther Nasuuna1*; Robert Lukande2 ; Yukari C. Manabe1,3
1. Research Department, Infectious Diseases Institute,
Key words: Cutaneous Tuberculosis.
Makerere College of Health Sciences, Kampala
Corresponding author: Esther Nasuuna
P.O Box 22418,
2. Department of Pathology; Makerere University of
Mulago Hospital Complex,
College of Health Sciences.
Kampala Uganda
3. Division of Infectious Diseases, Department of
Medicine, Johns Hopkins School of Medicine,
Tel; +256-414-307200 / +256-701-620063
Baltimore, Maryland, USA.
Abstract.
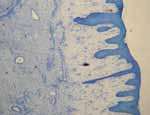
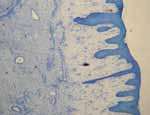
We report a case of primary cutaneous tuberculosis (lupus vulgaris) Fig 1
from the Infectious Diseases Institute, Mulago Hospital Complex, Kampala, Uganda.
A 28 year old, HIV positive woman presented with a four month history of large leg ulcers, fever and night sweats.
A wedge biopsy of the ulcer revealed stratified epithelium with foci of acathosis, ulceration of the epithelium and stroma with The physical exam was otherwise normal including the respira-
numerous Langerhans giant cells, necrosis and epitheloid cells tory system. Laboratory testing revealed a normal complete blood
with ill-defined granulomas.
count, normal renal & liver function tests, normal chest radiograph
The patient was started on anti-tuberculous drugs and has had ex-
and sputum was negative for acid fast bacilli.
cellent clinical response.
Purulent material gathered from the ulceration was cultured and
Case History
identified as pseudomonas aeuruginosa that was sensitive to gen-
A 28 year old woman who first presented to the Infectious Diseases tamicin and piperacillin tazobactam and resistant to ciprofloxacin
Institute (IDI) clinic in August 2010 with a four month history of and cefepime.
spontaneous, progressively enlarging ulcers on the anterior aspect
of the left leg. At that visit, she was tested and found to be HIV A skin biopsy was performed which showed stratified epithelium with
positive with a CD4+ cell count of 295 cells/μl.
foci of acanthosis, ulceration of the epithelium and stroma with numer-
ous Langerhan giant cel s, necrosis and epitheloid cel s with il defined
She also had an intermittently productive cough, persistent evening granulomas consistent with lupus vulgaris ( see figures below) .
fevers, drenching night sweats and poor appetite. She also reported
a 2-week history of voice hoarseness during that period.
She reported no history of weight loss, no history of trauma preced-
ing the ulcers. She had no prior history of TB disease or treatment
and had no known contact with a TB patient.
She had used various oral antibiotics but with no improvement in
the leg ulcers.
As a result of this biopsy and the culture, the patient was diagnosed
On physical exam, she was in good general condition, no wasting, with primary skin TB with pseudomonal super infection and treated
temperature was 37.4C. She had oral candidiasis, no lymphadenop-
athy, no figure clubbing.
with a 4–drug oral anti–TB therapy (ethambutol, rifampicin, pyra-zinamide and isoniazid) and also intravenous gentamicin 160mg
Examination of the lower extremities revealed two large irregular daily for 5 days. Two weeks later, she was started on zidovudine,
ulcers on the inferior aspect of her left leg measuring 5cm x 4cm lamuvudine and efavirenz (CBV/EFV) combination anti-retroviral
with undermined edges. The ulcer base had a light greenish dis-
therapy. Over the next 16 weeks, there was marked improvement of
charge (see figures 1& 2 ).
the symptoms and ulcer regression (see figures 6 and 7 ).
continues on Pg 4
Lupus vulgaris is a persistent, chronic skin ulceration. Lesions ap-
pear in normal skin as a result of direct extension of underlying tu-
berculous foci, of lymphatic or hematogenous spread, after primary
inoculation , BCG vaccination or in scars of old scrofuloderma3.
Definitive diagnosis is made histologically. The pathologic hall-
mark is an epitheliod granuloma with central caseation necrosis4.
In this case the patient had chronic ulcers that were treated with
many courses of antibiotics without improvement. This scenario of
Tuberculosis (TB) is an airborne, communicable disease that oc-
chronic, non–healing ulcers in an HIV (+) patient led the attending
curs after inhalation of infectious droplets expelled from patients physician to suspect and investigate for cutaneous TB. The sugges-
with laryngeal or pulmonary TB during coughing, sneezing or tive biopsy results and the excellent clinical response to anti–tuber-
culous medications further secured the diagnosis.
speaking. The most common site of the primary lesion is within
alveolar macrophages in sub-pleural regions of the lung. Although Non–healing ulcers in a setting of endemic, high burden TB should
mycobacteria are spread by blood throughout the body during ini-
warrant further biopsy-driven investigation for skin tuberculosis
tial infection, primary extra-pulmonary disease is rare except in especially in the immunocompromised.
severely immunocompromised hosts.
Cutaneous tuberculosis is invasion of the skin by mycobacterium The authors would like to grateful y acknowledge the patient and the
tuberculosis and it is an uncommon form of extra-pulmonary TB. staff of the IDI clinic. Funding for John Mark Bwanika and Yuka C.
It is more common in crowded parts of India and china. In Uganda Manabe has been provided from the National Institute of Health, DMID
and in particular at the Infectious Disease Clinic where 400 HIV under the Tuberculosis Clinical Diagnostics Research Consortium.
patients are seen daily with 30 of these in TB Clinic, no such case
has been reported before.
1 .Dwari BC, Ghosh A, Paudel R, Kishore P. A clinicoepidemiological study
This may be due to limitations in diagnostic capacity but also as a of 50 cases of cutaneous Tuberculosis in a tertiary care teaching hospital in
pokhara,Nepal. Indian J Dermatol, 2010 Jul-Sep; 55(3)233-7 (PUBMED)
result of the very low index of suspicion among clinicians. Even 2. Monte S Meltzer, Carol A Nacy, Cutaneous Tuberculosis (eMedicine
in areas with high TB prevalence, it occurs in less than 0.1% of Dermatology)
TB patients1,2. It has four common presentations that is; verrucosa 3. Bravo FG, Gotuzzo E.cutaneous tuberculosis. Clin Dermatol.
cutis, lupus vulgaris, scrofuloderma and tuberculoid.
4. Fariña MC, Gegundez MI, Piqué E, et al. cutaneous tuberculosis: a
clinical, histopathologic, and bacteriologic study. J Am Acad Dermatol.
Verrucosa cutis occurs after direct inoculation of TB in the skin of 1995;33(3):433–440.
a previously infected person. It presents a purplish or brownish red observations of cutaneous tuberculosis in Larkana, Pakistan. Int J Dermatol.
warty growth on the knees, feet and buttocks.
Buruli ulcer By Dr. Natalie Prevatt
Buruli ulcer is a necrotizing disease of skin and soft tissue. It is caused by an
environmental mycobacterium named Mycobacterium ulcerans.
M ulcerans produces a toxin called mycolactone that has cytotoxic properties,
which cause tissue necrosis (death of body tissue). Mycolactone is also im-
munosuppressive, and patients do not therefore present with fever or lymph-
Over weeks/months a nodule or papule breaks down into a necrotic ulcer
Nodule (Buruli commonly begins as
Plaque (occasional y it starts as a skin plaque)
a 1-2cm nodule)
What are the differentials?
Buruli ulcer was first described in Buruli, Uganda (now Nakason-
Early infection may look like an insect bite or pimple, psoriasis,
gola district) but has been reported in numerous African countries, or leprosy.
in Asia and Australia. Children under 15 years are most at risk in
Africa. Infection rates are equal for males and females.
The nodule can be mistaken for a cyst, lipoma, or onchocercoma.
Later it may appear similar to cutaneous leishmaniasis and TB, or
M. ulcerans live in slow moving or stagnant water, the exact trans-
the ulcer may appear like a venous ulcer or tropical ulcer, or as a
mission method is unconfirmed but is assumed to be through con-
deep fungal infection.
tamination of pre-existing minor wounds.
Buruli ulcer patients are not sick or febrile but the ulcer may be-
Human to human transmission is very rare. The true prevalence of come secondarily infected leading to sepsis or tetanus.
Buruli ulcer is not known because there is underreporting and the
variable presentation means that health workers often mistake it
for other things.
Is Buruli Ulcer more common in HIV?
Although Buruli is a mycobacterial infection there is little evidence
Is Buruli ulcer dangerous?
to suggest higher rates in HIV positive patients.
There is a low mortality rate, but because infection extends deep
into fascia, muscle and bone it often leads to permanently restricted How do you confirm the diagnosis?
function and considerable morbidity. The scars left behind also A direct smear of exudate from the necrotic base of the ulcer (or
have a social and emotional impact on the patients' life.
under the edge) should be sent for ZN stain. This may show acid-
fast bacilli. ZN stain only has 40% sensitivity and so if negative it
How does buruli ulcer present?
should also be sent for culture.
Lesions are normally on the limbs, especially the legs.
Culture is performed between 30-33 C (lower than for M.tb) and
Buruli begins as a small firm nodule which is mobile in the subcu-
takes 6-8 weeks on Lowenstein-Jensen medium. Culture has around
taneous fascia, or sometimes as a painless papule (in the dermis), 40% sensitivity.
or an elevated dry plaque. This is occasionally pruritic. In a period
ranging from days to weeks it begins to ulcerate.
PCR of biopsy specimens has very high sensitivity >90% and pro-
vides results in 48 hours. PCR diagnosis is being rolled out in some
African reference laboratories but is not available in the field.
Biopsies taken at operation can also confirm the diagnosis where
culture does not rule out other causes.
Do you need to confirm the diagnosis?
Diagnostic confirmation is a long process with low sensitivity.
Many patients present after ulceration has occurred. The ulcer is Treatment must be started early and so diagnosis is most often made
large, but remains painless. It usually has scalloped borders and based on epidemiological and clinical acumen.
necrotic slough in the base. A Buruli ulcer has an undermined edge
and thus the lesion appears smaller than it really is. It may destroy Management
vessels, nerves and bone. From here M. ulcerans can spread via Medical (all stage treatment)
lymph or blood to another site and satellite ulcers may develop
In 2004 WHO reported the effectiveness of specific antibiotics - the
recommended treatment is now directly observed rifampicin and
Lesions eventually heal with disfiguring scars and contractures.
streptomycin with or without surgery.
*less frequently an oedematous form may be seen which starts as a painful non–pitting oedmatous area.
Side effects
Adults: 10mg/kg/day up to 600mg/day PO
Gastro intestinal symptoms, flu like symp-
Children: 10-20mg/kg/day up to 600mg/day PO
toms, headache, altered liver functionbodily
secretions e.g. urine turn orange/red colour
Adults: 15mg/kg up to 1g OD
Children: 15mg/kg up to 1g OD
Nephrotoxicity, neurotoxicity, diarrhoea
Ciprofloxacin or clarithromycin can be used as
alternative to IM streptomycin– studies show no
significant difference in regimes
Adapted from WHO guidance 1
continues on Pg 6
There is no vertical Buruli ulcer programme in Uganda. Thus treatment should be given in local health centres, district and referral
hospitals, without delay. WHO suggests that in endemic countries such as Uganda treatment should follow a protocol, which is seen
here divided into 3 categories:
Form of disease
Primary aim
Small early lesion (nodules/papules/
Start antibiotics at least 24 hours before
plaques/ulcers <5cm diameter)
surgery and continue for 4 weeks
Schedule immediate excision and suture
If cannot excise then treat with same anti-
biotics for 8 weeks
Large ulcerative lesions (>5cm),
Give 4 weeks antibiotics before surgery
Reduce extent of surgery
(then surgery if still required)
oedematous/plaque forms (ulcerative/
followed by another 4 weeks antibiotics
lesions on the face/head/neck
Mixed/ disseminated disease including
Start antibiotics at least 1 week before
Reduce extent of infection
surgery and continue for 8 weeks
before surgical excision
Amended from WHO table 1
Although this recommendation was based on observational stud-ies, a recent RCT in Ghana 2 showed this treatment to be very ef-fective for patients with small early lesions: 96% of patients treated with eight weeks of rifampicin and streptomycin had healed le-sions at one year.
Surgical (late stage treatment)
Nodules/ papules and small ulcers are excised and closed.
Large ulcers are excised and closed with skin grafts. The addition of rifampicin and streptomycin to surgery has reduced recurrence rates ten fold 2.
(1) Provisional guidance on the role of antibiotics in the management of myco-
After treatment
bacterium ulcerans disease (buruli ulcer). WHO (World Wide Web document)
Ultrasound can be used to assess extension of ulcers under the skin Retrieved 1/2/11 from ht p:/ www.who.int/buruli/information/antibiotics/en/and thus response to treatment.
(2) Nienhuis, W.A. and Stienstra, Y. et al. 2010. Antimicrobial treatment for
early limited Mycobacterium ulcerans infection: a Randomized Control ed Trial.
Lancet. 20;375(9715):664-72
There is some evidence that BCG vaccination is protective but only for a short time. The Global Buruli Ulcer Initiative3 aims to im-
(3) Global Buruli Ulcer Initiative. In: Surveillance and control of Mycobacte-
rium ulcerans disease (Buruli ulcer). In: Fifty-seventh World Health Assembly,
prove the situation by increasing awareness among health profes-
Geneva, 17–22 May 2004. Resolutions and decisions. Geneva, World Health
sionals and encouraging early clinic attendance for patients with Organization, 2004 (WHA57/2004/REC/1):1–2.
suggestive early lesions.
Gill, G.E & Beeching, N.J. (2008) Lecture Notes on Tropical Medicine. 5th
Major advances are only likely to be made when a rapid diagnostic Ed. Oxford. Blackwell Science.
test becomes available for early disease.
Buruli Ulcer. WHO web page: http://www.who.int/buruli/en/
Dr Jenny Goldblatt
Three diseases caused by filariae can affect people in Uganda; phatic Filariasis (LF), 13 million of who live in Uganda. It is
these are lymphatic filariasis, onchocerciasis, and loa loa (figure estimated that the disease disfigures a third of people infected.
1). They are all spread by insect vectors. Whilst not fatal they do
cause chronic conditions which impact on patients' quality of life Vector: Mosquito species (Aedes, Anopheline, Culex, Mansio-
and their economic and social functioning. It is important to dis-
nia or Ochlerotatus)
cuss the filarial diseases at the same time because the treatments
used to kill one type of filariae can cause serious and sometimes Major features: Lymphoedema of the limbs, genitals or breasts,
fatal reactions in patients infected with another.
progressing to elephantiasis. Complications include bacterial
super-infection and "filarial fevers" (acute exacerbations) char-
Life of filariae inside humans
acterised by headache, malaise, pain and fever.
Filarial larvae gain entry to humans through the bites of infected
insects. They migrate into the body to mature into adults over Disease course: Infection is usually acquired in childhood.
a number of weeks. Adults produce millions of microfilariae Lymphoedema can develop several decades later and is caused
which can be found in many types of bodily fluid including blood by damage to the lymphatics from recurrent attacks of lymphan-
and CSF. The vector ingests the microfilariae when biting, thus gitis due to dying adult worms. Superimposed bacterial infec-
continuing the life cycle.
tions contribute to the severity of lymphedema from inflamma-
tion and fibrosis and subsequent progression to elephantiasis.
The complications of filarial infections often result from ineffec-
tive immune defense leading on to chronic carriage and inflam-
Oedema: Thrombophlebitis, venous thrombosis, cellulitis, bac-
terial lymphangitis, proximal lymphatic occlusion, heart failure,
cirrhosis, nephrotic syndrome.
Lymphatic Filariasis (Wuchereria bancrofti)
Scrotal Swelling: epidydimo-orchitis, abscess formation, hernia,
varicocoele, congential hydrocoele, epididymal cyst, testicular
An estimated 120 million people worldwide are at risk of Lym-
continues on Pg 8
Diagnostic tests:
If filarial fever occurs patients should take antipyretics and antibi-
Filariasis is diagnosed by identifying microfilaria on giemsa otic treatment if bacterial skin infection is present. Patients should stained blood film smears. Blood should be drawn at night (when be advised against cutting the skin. The WHO produces educa-the vector is expected to bite), diagnosis can also be made with a tional material for healthcare workers and patients on this topic. card-based antigen detection kit.
If you have any more concerns about filariasis, you can contact
ATIC on 0800200055
Management:
The mainstay of management is preventing complications: Advice There are limited trials that examine optimal drug treatment as part of
the patient to keep the affected area clean by washing with clean filariasis management. Current recommendations are based on lim-
ited trials and expert opinion. Adult worms are kil ed with the use of
water and soap, drying carefully and avoiding injury to the skin. Diethylcarbamazine DEC for 21 days, though this does not reverse
Affected limbs should be elevated where possible and patients existing changes (see table 1). DEC must be used with caution if co-
should exercise to aid lymphatic drainage.
infection with onchocerca volvulus is possible (see Onchocerciasis).
Table 1: Doses of medications commonly used in filarial disease
Lymphatic filariasis Treatment
Diethylcarbamazine (DEC) 1mg/kg first day, building up over 3 days to
6mg/kg/day (in 3 doses) for 21 days
Control (appropriate to
400mg taken once
150 mcg / kg taken onceWeight
Number of tablets
Treatment and control
As for LF. Repeated every 6-18 months for
several years.
Treatment of adult worms
200mg OD for 6 weeks (doxycycline not in
(with Ivermectin)
children <12 or pregnant women)
1mg/kg first day, building up over 3 days to
6 mg/kg/day (in 3 doses) for 21 days
Prevention - Mass Drug Administration (MDA)
ern borders of the country This includes areas like Arua, Yumbe,
In the past, there has been annual mass treatment to prevent LF Moyo , Adjumani, Hoima, Kasese and Kisoro across Uganda, using Ivermectin and Albendazole. This programme is no longer active. It is recommended that population based treat-
ment programmes are repeated annually for 5-6 years.
Onchocerciasis is spread by blackflies (Simulium sp), which live near fast flowing water. Bites are very painful.
Onchocerciasis (river blindness)
Epidemiology:
Features:
Nearly 3 million people live in regions of Uganda in which oncho-
Patients complain of intensely pruritic skin. This itch is due to
cerciasis is endemic. These are largely those areas along the West-
death of microfilariae as they migrate through tissue. As patients
continuously scratch, the skin of the thighs and buttocks becomes Surgical removal of skin nodules can be performed. lichenified and depigmented and loses its elasticity. This dermatitis progresses to atrophy where the typical hanging groin can be seen.
Prevention
Community directed MDA programmes
There are several manifestations in the eye including sclerosing Some community directed programmes using Ivermectin have been
keratitis, cataract formation and optic atrophy, all of which can established in parts of Uganda where there is a higher risk of On-
cause blindness. Eye disease usually starts as an itchy red eye due chocerciasis.
to inflammation triggered by parasite migration.
The Onchocera volvulus adults may lie in subcutaneous nodules. Loa Loa
These are often seen near bony prominences which the worms have Importance:
been unable to pass by.
People infected with Loa Loa can have serious adverse reactions such as encephalopathy and retinal haemorrhage if treated with
Ivermectin. Loa Loa is know to be prevalent in Central and West
Skin manifestations: atopic dermatitis, contact dermatitis, chronic Africa, including regions bordering Uganda, and has previously
eczema, malnutrition, loa loa, superficial mycoses, streptocerciasis, been reported in Uganda, so it is important to be vigilant for evi-
vitiligo, lipoma.
dence of this disease in areas in which Ivermectin may be given.
Ocular manifestations: glaucoma, trachoma, cataract
Vector: Mango Fly (Chrysops sp).
Features:
Diagnostic tests:
Infected individuals are often asymptomatic. Localised, sudden onset
Skin snips are taken from near a nodule or a high yield area such and short-lived inflammation may occur as a result of migration of as the thigh. The skin is lifted with point of a needle and a 1mm adult worms through the subcutaneous tissues. This Calabar swel -scalpel snip is collected and sent to laboratory in saline to look for ing, often at the wrist, is reported by the patient as a swel ing which microfilarae and typical histological changes. Serology does not appeared and disappeared leaving no trace. Worms may visibly mi-distinguish between past and current infections.
grate under the sclera of the eye, which is distressing for the patient.
Management:
Differential Diagnosis of Calabar swelling:
The mainstay of treatment is Ivermectin (see table 1). This can im-
Reactive arthritis, onchocerciasis, idiopathic angioedema
prove both ocular and dermatological manifestations. Ivermectin
prevents production of microfilaria (but has no action against adult Diagnostic tests:
worms, which can live in humans for around 12 years, and so treat-
Visualisation of microfilariae in blood taken at noon when the vec-
ment must be repeated every 6-18 months for a number of years.
tor is most likely to bite. Serology has been used for population screening.
Doxycycline has some activity against adult worms and can be giv-
en at a dose of 200mg daily for 6 weeks in addition to Ivermectin Treatment:
but not in children under 12 years.
DEC can be used against adult worms (see table 1). Encephalitis has been reported in patients with high microfilarial loads due to
Treatment carries a risk of al ergic / inflammatory reactions which death of migrating worms. can lead to facial oedema, anterior uveitis, keratitis, tachycardia and postural hypotension as wel as myalgia, lymphadenopathy, syno-
Adults migrating across the eye can be removed surgically if it is
vitis and headache. Although this is markedly more common with not possible to do this with the corner of a piece of paper.
DEC, particularly in the malnourished, 1-5% of those treated with Ivermectin alone may also be affected.
Interaction with HIV
There is no clear evidence of significant interaction between HIV
The use of low dose dexamethasone (3mg/kg) may reduce the severity and filarial infections, though there is experimental evidence to of this reaction without reducing anti-microfilarial activity. Ivermectin suggest that lymphocytes from those infected with filariae may be is not safe for pregnant women, lactating mothers, children younger more susceptible to HIV infection.
than five years and people with heart, liver and kidney diseases.
Adults larvae produce millions of microfilariae which
can be found in many types of bodily fluid including
blood and CSF.
Ethambutol Associated Optic Neuritis :
One Of The Side Effects To Look Out For In Patients Treated For TuberculosisMonica Amuha Grace B.Pharm, MPS
Ethambutol is a synthetic antituberculosis agent used in com- Patients who develop optic neuritis may complain of bilateral
bination with other antituberculosis agents in the treatment of progressive painless blurring of vision or decreased color per-
clinical Tuberculosis (TB). Tuberculosis caused by Mycobac- ception. Some individuals may be asymptomatic with abnor-
teruim tuberculosis, is a major cause of morbidity and mortal- malities detected only by vision tests.
ity in Uganda. Uganda was ranked 18th out of the 22 tuber-
culosis high-burden countries in the world during 2009. The Examination by an ophthalmologist may reveal pupils that are
incidence of TB is 330/100,000 population for all TB cases and bilaterally sluggish to light, decrease in visual acuity with mini-
136/100,000 population for sputum smear-positive pulmonary mal or no light perception, constriction of visual fields, areas of
TB. The Annual Risk of TB Infection (ARI) for Uganda is esti- diminished vision within the visual field( scotomas), and loss of
mated at 3 percent.
red-green color discrimination which may be the earliest sign
The interaction between TB and HIV is increasing the burden
of both diseases. HIV is one of the major risk factors for the
development of active TB among individuals infected with My- Characteristics of ocular toxicity of ethambutol
cobacterium tuberculosis. At present, an estimated 60% of TB The extent of ocular toxicity appears to be dose and duration re-
patients in Uganda are also infected with HIV. TB accounts for lated. However, such toxicity has also been reported rarely only
30 percent of all deaths among HIV positive patients.
after a few days of therapy with the drug.
The recommended first line anti-tuberculosis agents used in Dose-related
management of TB include; rifampicin(R), Isoniazid (H), The reported incidence of ethambutol-related optic neuritis var-
Pyrazinamide(P) and Ethambutol(E).
ies between 18% in patients receiving more than 35 mg/kg per
day, 5% to 6% with 25 mg/kg per day, and less than 1% with
The current WHO 2010 TB guidelines no longer recommend an 15 mg/kg per day ( the recommended dose) of ethambutol for
8 month regimen of 2RHZE and 6EH as the first line treatment more than 2 months. 50% of ethambutol is excreted in urine,
for tuberculosis in adults. They instead recommend a 6 months therefore patients with poor renal function are at higher risk of
regimen containing 2RHZE and 4RH . This is because the use of ocular toxicities.
rifampicin for only 2 months in the intensive phase was associ-
ated with a high rate of relapses and deaths.
The manifestation of ocular toxicity is usually delayed, and gen-
However, in Uganda we are yet to adopt this recommendation erally does not develop until at least 6 weeks after treatment.
and are still using an 8 months regimen of 2RHZE/6EH. With The mean interval between onset of therapy and toxic effects
this regimen, there is a longer duration of exposure to ethambu- has been reported to be 3 to 5 months. However, manifestations
tol thus increasing the risk of ethambutol associated side effects. of toxicity as late as 12 months after therapy initiation have also
Ethambutol has several side effects that include optic neuritis,
headache, malaise, dizziness, mental confusion, fever, abdomi- Other factors that predispose subjects to toxicity include
nal pain, anorexia, nausea and vomiting and more rarely periph- diabetes and optic neuritis related to tobacco and alcohol
eral neuritis, rash, pruritus, urticaria, hepatitis and thrombocyto- consumption.
penia. The most important of these is optic neuritis.
Management
Patients in whom ethambutol is relatively contraindicated should Where possible patients commencing treatment with ethambutol
be identified before initiation of TB treatment. These include pa- should have a baseline eye examination including best corrected
tients who are unlikely to notice or describe visual symptoms, visual acuity, color vision and visual field. These parameters
such as patients with dementia, mental retardation and children. should then be monitored periodically (every 1 to 3 months) .
In some of these patients e.g. children below 12 years, etham-
butol should be avoided, (recommended first line regimen for Outcome
children below 12 yrs is 2 months of RHZ and 4 months of RH) When ocular toxicity is detected early and ethambutol is discon-
and in others pharmacovigilance should be encouraged.
tinued promptly, the visual effects are generally reversible over
a period of weeks or months. Rarely, depending on the degree of
The dose of ethambutol must always be carefully calculated on impairment, recovery may be delayed for up to 1 year or more,
a weight basis and the dose or the dosing interval should be ad- or the effect may be irreversible. Care should be taken to be
justed based on creatinine clearance in patients with impaired
renal function. If creatinine clearance is between 10-50ml/ certain that variations in vision are not caused by underlying
minute: administer 15mg/kg of ethamutol every 24-36 hours, pathologic conditions such as cataracts, diabetic retinopathy or
if creatinine clearance is <10ml/minute administer 15mg/kg of CMV retinitis in HIV positive individuals.
ethamutol every 2 days.
Patients treated with ethambutol should be educated on the pre- 1. AHFS Drug Information 2009, American Society of Health System Phar-
senting sign and symptoms of ocular toxicity i.e. blurred vision
macists. Page 576-578
2. Drug Information Handbook, A comprehensive Resource for all Clinicians
and/or decreased colour perception. They should promptly seek
and Healthcare Professionals 18th Edition, 2009-2010. page 573-574
medical advice if their sight or perception of color deteriorates. 3. Ministry of Health Manual of The National Tuberculosis and Leprosy Pro-
In this case, ethambutol should be stopped and replaced with
gramme: 2nd edition 2010
streptomycin during the intensive phase and rifampicin and iso- 4. Treatment of Tuberculosis Guidelines Fourth edition WHO 2010
niazid should be given for the continuation phase for 4 months.
5. www.bnf.org BNF 61 March 2011
ATIC Dr. Stella Zawedde-Muyanja. MBChB
As a Quality Improvement advisor at health centers in Eastern Uganda, I have observed some
challenges in provision of antiretroviral therapy (ART) at the facilities I supervise.
Due to challenges in logistics management, some health centers experience occasional stock outs of
antiretrovial drugs (ARVs) ranging from single drug formulations to fixed dose combinations.
This often leads to rationing of the available ARVs for clients as providers wait to receive more stocks.
Sometimes, this rationing leads to treatment interruptions for varying durations among HIV/AIDS
clients on antiretroviral therapy.
Are there risks of resistance associated with such unplanned interruptions in antiretroviral therapy ?
If so, after what duration of interruption do you anticipate emergence of resistance and recom-
mend change in treatment regimen ?
Yes there are.
Treatment Interruptions whether planned or unplanned are not recommended during Antiretroviral Therapy.
Evidence that treatment interruptions are not a good treatment option comes from previous clinical trials that
explored different treatment interruption schedules
One of these clinical trials was a randomized trial nested within a bigger trial (the DART Trial) . This trial
compared fixed length Structured Treatment Interruption and Continuous Treatment in adults on first line
Antiretroviral Therapy (ART).
Patients who had been on ART for more than 48 weeks and were clinically stable with CD4 cell counts
above 300cells/ul were randomized to continue taking ART continuously or to undergo Structured
Treatment Interruptions with repeated 12 week periods on or off therapy
This trial was stopped early because patients in the structured treatment interruption arm had a greater risk
of disease progression and more HIV related complications than patients in the continuous treatment arm.
Trials of treatment interruption done in other countries produced similar results with more deaths, drug
related complications and HIV related events in patients who underwent the treatment interruption.
The speed at which resistant mutations emerge after treatment interruption depends on the type of
ART regimen and the mode of discontinuation.
Patients whose treatment gets interrupted while on Non-Nuleoside Reverse Transcriptase Inhibitor
(NNRTI) based regimens develop resistance (to the NNRTI component) very quickly. This is because
the NNRTIs (efavirenz and nevirapine), have very long half lives and stay in the bloodstream longer than
the Nuleoside Reverse Transcriptase Inhibitors (NRTIs). Patients are in effect exposed to monotherapy
with NNRTIs which leads to resistance. The situation is worse if the ART regimen is stopped without
a twoweek lead out dose of the NRTIs. This is unfortunately what happens in most cases of unplanned
A study done in Kampala , which followed up HIV-positive, antiretroviral-naive individuals initiating
ART on stavudine, lamivudine and nevirapine for 24 weeks, found that treatment interruptions were
significantly associated with drug resistance. At the end of this study, none of 33 participants who did
not interrupt treatment for over 48 h had drug resistance, whereas eight of 62 (13%) participants who
did interrupt therapy experienced drug resistance.
It is therefore important for all personnel involved in ART care to realize that they should do their best to
ensure continuous supply of ART so that their patients can continue their treatment without interruption.
A few measures that healthcare workers can put in place to achieve this are ;
• Submitting drug order forms to the district focal person and to National Medical Stores (NMS) in a
timely manner to facilitate drug processing and delivery.
• Accurate quantifying their drug needs so that all patients on their programme are catered for
References:
•
Medical Management of HIV infection 2009-2010 Edition: Pages 109-111
Fixed Duration Interruptions are inferior to continuous treatment in African Adults starting therapy with CD4cell counts < 200 cells/ul.
The DART Trial Team AIDS 2008, 22: 237-247
Treatment interruptions predict resistance in HIV-positive individuals purchasing fixed-dose combination antiretroviral therapy in Kampala, Uganda
Jessica H. Oyugi, Jayne Byakika-Tusiime, Kathleen Ragland, Oliver Laeyendecker, Roy Mugerwa, Cissy Kityo, Peter Mugyenyi, Thomas C. Quinn and David R. Bangsberg, AIDS 2007, 21:965–971
Source: http://idi.mak.ac.ug/docs/ATIC%20Newsletter%20June%202011.pdf
BMJ 2012;344:e615 doi: 10.1136/bmj.e615 (Published 2 March 2012) Cost effectiveness of strategies to combat vision and hearing loss in sub-Saharan Africa and South East Asia: mathematical modelling study Rob Baltussen senior researcher 1, Andrew Smith honorary professor 2 1Department of Primary and Community Care, Radboud University Nijmegen Medical Center, PO Box 9101 6500HB Nijmegen, The Netherlands;2Centre for Disability and Development, London School of Hygiene and Tropical Medicine, London, UK
Anti-libidinal medication and people with disabilities – long-term follow-up of outcomes following third party consent to medication for problematic sexual behaviour CRC 38/00-01 REPORT TO THE CRIMINOLOGY RESEARCH COUNCIL AUGUST 2002 Associate Professor Susan Hayes, AO, PhD Fiona Barbouttis, BA, GDS (Psych)