Microsoft word - coma04final.doc

CLINICAL VIGNETTE
An 18-year-old woman with medically intractable seizures
An 18-year-old woman presented for evaluation of seizures that were not controlled by medical
therapy. At the age of 6 months she was hospitalized with a fever and seizures, and was reported
to have encephalitis. She lost motor and language developmental milestones, but these were
gradually regained and she was treated for a year with phenobarbital and was without recurrent
seizures. The phenobarbital was tapered at age 2 but at the age of 6 years she again experienced
seizures, which occurred at low frequency until puberty, when the seizure frequency increased to
two to three per day. The seizures were characterized by an initial aura of tightness in the head
and chest and sweaty palms, followed by impaired consciousness, lip smacking, hand rubbing,
and unresponsiveness. During a seizure she was unable to talk but could hear, and could not
fully process information. She was treated with a variety of anticonvulsants, including
phenobarbital, carbamazepine, phenytoin, valproate, and lamotrigine without significant success
in seizure control. Her medical history was otherwise unremarkable. There was no family
history of seizures.
Physical Examination: Vital signs: normal. Bedside mental status examination: no significant
abnormalities. Neuropsychological testing: full-scale IQ of 97, performance IQ of 97 and a
verbal IQ of 96; mild difficulty acquiring certain types of information and some difficulty with
uncued recall. Speech: normal. Cranial nerves: normal with only minimal, unsustained
nystagmus on lateral gaze. Motor and sensory examinations: normal. Muscle stretch reflexes:
normal. Coordination and gait: normal.
Stop and Consider: What is the classification of her seizures according to the International
Classification of Seizures? How should she be treated at this point?
Laboratory Findings: CBC, serum
chemistries with liver and renal functions,
PT, PTT, ESR: normal. MRI: see figure,
shows left hippocampal atrophy and
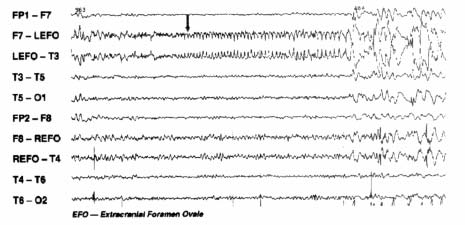
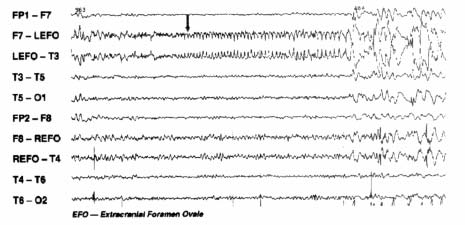
increased T2 signal. Interictal EEG: left
temporal sharp and slow wave activity
suggestive of left temporal onset of seizures.
Continuous video-EEG monitoring: several
seizures captured. EEG, see figure, next
page, shows left mesial temporal (EFO)
onset. Interictal positron emission
tomography (PET) scan: hypometabolism of
the left temporal lobe.
Diagnosis: Medically intractable partial
complex seizures associated with
hippocampal atrophy.
In this patient, MRI, prolonged video-EEG monitoring study, and PET scan were
consistent with a left mesial onset of seizures and invasive EEG recording was not necessary. Preoperative Wada's test (intracarotid amytal injection) demonstrated left hemisphere language dominance and adequate right hemisphere memory function. She underwent left anterior temporal lobectomy and did very well postoperatively in terms of memory function with no change from her baseline findings, and became seizure-free. An attempt to taper by antiepileptic drugs was followed by breakthrough of seizures but reinstitution of antiepileptic medications again resulted in complete seizure control.
EPILEPSY
Epilepsy: anatomic and physiologic correlates
Epilepsy is the condition of chronic recurrent seizures that occur because of an
inherent problem with brain hyperexcitability. Seizures are the phenomenon of abnormal
synchronization of cortical neurons that results in a change in perception or behavior.
There are many causes of seizures that include intoxications by drugs that alter neuronal circuit
excitability (e.g. cocaine or drugs that block synaptic inhibition), withdrawal from certain drugs
(e.g. alcohol), or a wide variety of metabolic derangements (low glucose, low calcium, hepatic or
renal failure). Up to 8% of the population will have a seizure at some time in their life.
Epilepsy, however, is a condition in which seizures occur without definite
provocative factors. About 0.5% of the population has epilepsy. There are many causes of
epilepsy and the term does not refer to a specific disease but a condition.
We classify seizures in terms of the anatomic correlate of the abnormal
synchronous electrical activity. In the broadest sense seizures are either focal, starting in one
region of the cortex, or generalized at onset, beginning diffusely throughout the cortex and
driven by thalamocortical pathways. Focal seizures may spread to become secondarily
generalized seizures and the anatomic substrate includes corticothalamic, thalamocortical,
association fibers, and callosal connections.
Focal seizures are termed partial
seizures and the symptomatology is dictated
by what area of the cortex is activated.
When these seizures do not affect
consciousness, they are referred to as
simple partial seizures. If the motor cortex
is involved, then the seizure consists of
rhythmic motor activity contralateral to the
focus. Correlating the behavior of seizures
and the associated lesion or electrical
abnormality has greatly enhanced our
understanding of cortical anatomy. In fact
the homunculus that you are all familiar with
was a product of a neurosurgeon (Wilder
Penfield) stimulating the brain of awake
patients undergoing surgery to try and
remove the area of abnormality responsible
for their seizures.
Partial seizures, particularly those that begin in the limbic system may begin with various
emotional feelings like fear and may also cause deja vu sensations. Limbic seizures often spread
to involve important substrates for consciousness without producing frank unconsciousness.
When a focal/partial seizure involves impairment of consciousness the seizure is referred to
as a complex partial seizure. The patient does not remember what they do during the seizure,
usually there is significant dysfunction of the hippocampi during the seizure that blocks memory
formation. During this period, usually lasting 1-2 min, a variety of automatic behaviors may
occur and are termed automatisms (an automatic and apparently undirected, nonpurposeful
behavior that is not consciously controlled.)
Classification of Seizures
A. Simple: consciousness unaffected, symptoms refer to cortex involved
B. Complex: consciousness impaired, amnesia
C. Secondarily generalized, thalamocortical and other pathways involved
II. Generalized A.
Any seizure that begins in one area of the cortex (partial or focal) may spread and the
seizure may evolve into a generalized tonic-clonic or grand mal seizure. The seizure spreads
via the anatomic connections that you have learned about and include connections to adjacent
gyri, to the opposite hemisphere via the corpus callosum, and to the thalamus.
Partial seizures are associated with underlying regions of abnormal cortical
excitability that results from any of a great many insults. The EEG correlate of partial
seizures is the interictal (between seizure or ictus) spike or sharp wave that is localized to a
region of the scalp. When a seizure occurs, a more sustained abnormal rhythm that consists of
rhythmic slow and spike or sharp activity occurs in the EEG. As the seizure spreads, other brain
regions reflect abnormalities in the EEG.

Generalized seizures are either associated with a genetic predisposition for abnormal
excitability inherent to an instability in the thalamocortical connections or result from a
severe dysfunction of neuronal activity from multiple lesions or inherited neurologic
storage diseases.
Generalized seizures begin all over the brain at once and are a product of an
instability of the thalamocortical circuitry. The most intense generalized seizure is a tonic-
clonic seizure that consists of a tonic phase lasting up to 20-30 seconds followed by rhythmic
clonic muscle activity lasting another 30-60 seconds. After a tonic-clonic seizure the patient has
post-ictal unresponsiveness that evolves to a period of consciousness and confusion. Other
generalized seizures are less dramatic but may be equally problematic. Absence seizures (petit
mal) are associated with high voltage 3 Hz spike (versus a normal 8-12Hz "awake" EEG) and
wave activity associated with rather minor behavioral changes. During an absence seizure, the
person may stare, blink their eyes at 3/sec, and will not respond to verbal stimuli. The seizure
only last 15-20 seconds and the person is amnestic for what ever happens during the seizure.
Afterwards the EEG and the person return to normal without postictal changes.
Myoclonic seizures are repetitive jerks of axial and limb musculature that are usually
brief and also associated with a generalized spike-wave pattern. Seizures may also be generalized and associated with loss of motor tone (atonic seizures) or marked increase in tone (tonic seizures). These latter two seizures are also brief, lasting seconds, and associated with a desynchronization or decremental response in the EEG.
The thalamocortical pathways that mediate these seizures are the same pathways
that modulate sleep-wake cycles. In fact the generators of sleep spindle activity are the same
that lead to absence seizures. When not treated, people with absence seizures have very few
spindles but instead have spike-wave activity. With treatment, the spike-wave abnormalities are
replaced by normal spindle activity.
We also try to classify the syndrome associated with a patient's epilepsy. Seizures that
begin focally are considered to be localization related epilepsy and the characteristics of the seizure relate to the area of where the seizures begin, e.g. from the frontal, temporal, occipital, or parietal lobes. Many of the generalized seizures that have a definite inherited predisposition may remit with maturation, and the clinical picture is of a developmental syndrome.
Our treatment of seizures depends on the type of seizures. In general, seizures appear
to begin because of an imbalance between synaptic inhibition and excitation. For
generalized seizures this imbalance exists in thalamocortical circuitry. An effective drug for
absence seizures is ethosuximide, which reduces low threshold calcium currents. In partial
seizures the imbalance in inhibition and excitation is localized to a specific cortical area.
The drugs we use to treat these seizures tend to decrease the ability of neurons to fire action
potentials at a high rate (eg. phenytoin or carbamazepine). Another treatment strategy is to
increase inhibition by using drugs that enhance GABA's function (eg. phenobarbital or diazepam
derivatives). Recent drugs have also been targeted to blocking GABA uptake or enzymatic
degradation. In the future, drugs may be targeted to specific glutamate receptors that may be
particularly important for seizure generation.
READ ON ONLY IF YOU ARE INTERESTED.
I WILL NOT ASK YOU ANY QUESTIONS ABOUT WHAT FOLLOWS.
Thalamocortical circuitry in sleep-wake physiology
The interaction between the intralaminar nuclei of the thalamus and the cortex defines our state, i.e. are we awake or sleep, and what state of sleep are we in. The thalamic relay neurons, those neurons that project to the cortex, have membrane properties that define how they fire at different membrane potentials. When the neurons have a membrane potential of around -80mV, they fire in a bursting mode. The burst firing mode results from a low threshold voltage dependent calcium current. At a membrane potential of about -65 mV, they fire in a more regular mode of single action potentials. At this membrane potential the low threshold calcium current is inactivated (similar to the inactivation of sodium current that occurs with depolarization).
The transfer mode of neuron firing is the basis for an awake, alert state. A number of neurotransmitters or modulators can produce depolarization so that the membrane potential is around -65 mV. The membrane potential can be depolarized by closing potassium channels. Neurotransmitters like acetylcholine, norepinephrine, or histamine will favor the transfer mode of firing).
The burst firing mode is characteristic of stage II and III sleep and the bursting of the
relay neurons drive the generation of sleep spindles. The relay neurons are hyperpolarized by GABAergic input from the reticular neurons. GABA acts at both GABAA and GABAB receptors and the GABAB receptor activation changes the relay mode to a burst firing mode. Because none of these neurons function in isolation, the synaptic circuitry involving the relay neurons, the reticular neurons, and cortical neurons allow for oscillations to occur. Deep sleep characterized by slow waves is associated with even more hyperpolarization of the relay neurons and a slower 1-2 Hz oscillation. REM sleep is associated with a return to a relay mode of firing.
Problem Solving
1. Seizures that begin in one area of the cortex are called:
A. generalized seizures
B. absence seizures
C. primary seizures
D. partial seizures
E. none of the above
2. Generalized seizures: A. are not localized at their onset B. predisposition is often inherited C. occur because of thalamocortical circuitry instability D. all of the above E. none of the above
3. Partial seizures that impair consciousness: A. are called a complex partial seizure B. patient remembers what they do during seizure C. never evolve to tonic-clonic D. do not involve the limbic system E. none of the above
4. Any of these mechanisms may have anti-epileptic actions except: A. increased synaptic inhibition B. decreased synaptic excitation C. decrease of a low threshold calcium current D. decrease in ability of neuron to generate action potentials E. enhancement of glutamate receptor numbers on cortical neurons
5. Which of the following statements is FALSE regarding complex partial seizures?
A. begin with a deja vu sensation
B. originate in the temporal lobe
C. never lead to generalized tonic-clonic seizures
D. involve limbic structures
E. may result from head trauma
6. Consciousness is normal during which type of seizure?
A. generalized tonic-clonic
B. absence
C. complex partial
D. simple partial
E. none of the above
Problem solving ANSWERS
Consciousness: Neuroanatomy, physiology, and pathophysiology
We all know what consciousness is and recognize that we are conscious beings. But
what makes us conscious? In this lecture we will explore the anatomy, physiology and pathophysiology of consciousness. The goals are to define how abnormalities of consciousness and its regulation are symptoms of disease processes. The student should be able to identify key anatomic substrates of consciousness, how their activity defines changes in consciousness, and how injury to these anatomic substrates produce conditions of abnormal consciousness.
What is consciousness? I know that if you are reading this sentence you are conscious.
In simplest terms, consciousness is the awareness/perception of self and environment. It is a
state in which we can respond appropriately to our environment. If you are starting to drift off to
sleep as you read these notes, your level of consciousness is decreasing. A strong afferent
stimulus like a door slamming or a fire alarm will help you regain your consciousness. In more
philosophical terms, consciousness represents a condition of self-awareness that includes abstract
thought processing. Modern neuroscience believes that consciousness is produced by our brain's
activity.
Coma: Pathologic Unconsciousness
The condition of unconsciousness from which a patient cannot be aroused is termed
coma. If the patient arouses but quickly falls back into unconsciousness we call them stuporous.
Stupor and coma have many causes and patients need to be thoroughly evaluated as to cause.
The anatomy of coma must include dysfunction of one of the following: both cerebral
hemispheres, the thalamus, or the ascending reticular activating system (ARAS).
The most common causes of coma are metabolic derangements. We term this condition
encephalopathy. Some of these comatose patients are comatose because of a drug overdose.
The most common drugs include barbiturates and alcohol that enhance the GABAA receptor
function. GABA is the main inhibitory neurotransmitter in the brain. Interestingly most
anesthetics also act at the GABAA receptor. Other drugs that cause coma are opiates and
compounds that have an anticholinergic effect. Remember that our awake and alert state is in
part due to cholinergic drive on thalamic and cortical neurons.
Other patients who are comatose because of metabolic problems have endogenous metabolic
abnormalities. Neurons are affected by a variety of metabolic abnormalities and cause them to function abnormally. These include encephalopathy following hypoxia, because of organ failure (liver, kidney, or endocrine), and because of electrolyte or glucose disturbances.
Consciousness 1042
Patients with metabolic coma do not have focal
neurologic findings unless they are due to pre-existing conditions. They may have hypo- or hyperreflexia but the findings are symmetric. Babinski signs may be present, but are usually bilateral. These patients have coma because of a diffuse disturbance of cortical, thalamic and ARAS. The EEG shows slowing and a variety of periodic patterns.
Comatose patients also have lesions in the brain
stem. The most common cause of these lesions is thrombosis of the basilar artery. Their coma results from injury to the ARAS.
One condition you should be familiar with is called the "locked-in" syndrome. In this
condition there is a lesion, usually produced by a stroke, in the ventral pons that cuts off the corticospinal and corticobulbar tracts bilaterally (see figure below). The ARAS is spared (travels in the tegmentum) so that the patient is conscious; however, the patient cannot move or speak. Communication can be maintained by having the patient open or close their eyes in a coded fashion. The EEG is normal since the ARAS is not damaged. It is important to recognize the existence of the "locked-in" state and communicate with the patient appropriately.
Brain stem damage resulting in coma also
occurs following supratentorial (structures lying above the tentorium cerebelli) lesions. In the following (A, B, C, D) you can see the effects of a cortical lesion/mass that eventually causes compression/damage/death of most of the diencephalon and brain stem.

SCENARIO A
Let's suppose a subarachnoid hematoma has affected the right cerebral hemisphere and
diffusely affected the thalamus and hypothalamus, perhaps more on the right. (We understand
that this diagram is very schematic!!). This causes a left hemiplegia. The effect of the lesion on
the thalamus induces coma. The left upper arm is flexed and the left lower limb is extended.
This should sound familiar. This posturing of the limbs in which coma is also present is called
DECORTICATE RIGIDITY. Both pupils are small (meiosis; sound familiar?) as the
hypothalamus is damaged on both sides and thus the descending sympathetics to T1-L2 are
interrupted. The pupils are, however, reactive to light because the pathways for the pupillary
light reflex are intact. Caloric stimulation (remember COWS!) is normal at this time as CN VIII
is caudal and the connections of the VOR are intact. Interestingly, when you excite the circuitry
of the VOR you don't get the snap-back second movement of nystagmus. This is because the
fast movement is dependent upon a normal frontal eye field, i.e., cortex. These descending
projections to the PPRF are damaged bilaterally in the internal capsule. Since the fast movement
is gone, warm water into right ear (for example) will result in movement of the eyes left.
Moreover, if you move the patient's head to the right (be sure that the cervical spine is OK) the
eyes will turn to the left. This is called DOLL'S EYES.


Consciousness 1044
SCENARIO B
A little later in the scenario, there is
compression/damage/death to deeper structures.
The cortex, thalamus and hypothalamus are more
affected and begin to comprise a central mass or
central herniation that pushes on the midbrain.
The decorticate rigidity now involves all four
extremities. The pupils will usually be mid-sized
and unreactive to light (fixed). This is due to the
bilateral interruption of the descending
autonomics and stretching of CN IIIs. Since CN
III is damaged, the action of the VOR is affected.
Thus stimulation of the right ear with warm water
will result in movement of the left eye, (right
vestibular apparatus, right vestibular nuclei, left
PPRF and left LR6 are fine). However, the right
medial rectus cannot contract as CN III is shot.
NO DOLL'S EYES.
SCENARIO C
Now the lesion has moved down to include the midbrain, at the level of the junction of the superior
colliculus and inferior colliculus. The coma now includes what is called DECEREBRATE
RIGIDITY. All four extremities are extended. The pupils are in mid-position and unreactive to
light (fixed). This is due to the lesion damaging both descending autonomic pathways and the CN IIIs
(fibers and nuclei). Since CN III is damaged, the action of the VOR is affected. Thus stimulation of
the right ear with warm water will result in movement of the left eye, (right vestibular apparatus, right
vestibular nuclei, left PPRF and left LR6 are fine). However, the right medial rectus cannot contract
as CN III is shot. No DOLL'S EYES

SCENARIO D
Here the lesion extends into the medulla. There are no extreme positions of the extremities. The
pupils are still in midposition (descending autonomics and CN III are shot!) and fixed
(remember, the lesion now runs the length of the brainstem). Since the vestibular nerves/nuclei
are now damaged, the VOR does not work.
herniation also results from supratentorial pressure. This occurs when the uncus
and medial temporal lobe structures herniate through the tentorial notch. The local anatomy of
this region includes CN III. Because fibers that produce pupillary constriction are on the
outside/periphery of CN III, pupillary dilatation and a sluggish response to light are the first
signs of CN III nerve compression. (It is interesting that in a diabetic mononeuropathy of CN
III, the most central fibers (associated with the somatomotor/eye muscle innervation are affected
first, sparing the peripherally located parasympathetic fibers). The left herniation causes the left
cerebral (smart) peduncle to be damaged; this results in a contralateral/right hemiplegia in
addition to the ipsilateral/left dilated pupil. In some cases the pressure distribution results in the
opposite (right) cerebral peduncle being compressed against the tentorium. This results in
hemiplegia ipsilateral to the CN III dysfunction. When the opposite (to the herniation) cerebral
peduncle is compressed against the taunt free edge of the tentorium cerebelli, a "notch" in the
peduncle occurs. This is called Kernohan's notch. Most herniations cause
twisting/compression/stretching of the brainstem that results in damage to penetration branches
of the basilar artery. These are called Duret hemorrhages.
Consciousness 1046
Brain Death
Modern medicine allows us to maintain vital functions without a conscious brain. In some
cases the brain is damaged so that functional recovery is not possible. The most severe condition is
brain death and is associated with the lack of any cortical or brain stem function. There is no
response to pain or verbal stimulation, all brain stem reflexes are absent (pupillary response,
vestibulo-ocular response from caloric stimulation, corneal and gag reflexes), and there are no
spontaneous respirations. To test for respiratory drive, the ventilator is disconnected and 100%
oxygen is delivered to the distal trachea. This maintains oxygenation but allows CO2 accumulation,
which should trigger respiration if there is any central respiratory drive from around the solitary
nucleus to an intact lower motor neuron system for respiration. Besides
absence of these functions, brain death can only be declared if the patient is
not hypothermic or on any medications which could depress brain stem
reflexes (curare, high dose barbiturates or other anesthetic compounds).
Brain death is a clinical diagnosis and sometimes it is helpful to
confirm it with laboratory tests. One confirmational test is electrocerebral silence as defined by EEG. A problem with this test is the interpretation of a record with artifacts that may mimic brain activity. Another test is to demonstrate the absence of cerebral blood flow as measured by radionucleotide blood flow scanning or the lack of cerebral metabolism as measured by PET (positron emission tomography) or SPECT (single photon emission computerized tomography) scanning. Brain death allows for the procurement of organs for transplantation so strict criteria are required.
A. Pupillary reflexes are tested by shining a bright light alternatively in each eye,
while looking for a DIRECT and CONSESUAL response of the pupil. In
Brain Death neither pupil will react to light and the pupils will be in
midposition. Tests integrity of CN II and optic tract and CN III = oculomotor
nerve and nucleus.
B. The corneal reflex is tested by touching each cornea with a cotton swab while
looking for bilateral contraction of the orbicularis oculi. In Brain Death this
reflex is absent bilaterally. Tests the integrity of CN V (chief sensory V) and
CN VII (motor VII and nerve supplying the orbicularis oculi muscles).
C. The vestibulo-ocular (or oculovestibular) reflex is tested by irrigating the ear
canal with ice water with the head at a 30o angle up from the horizontal, while
looking for eye movements. In Brain Death there will be NO movements of
the eyes upon caloric stimulation. Tests the integrity of CNs III, VI and VIII
and the VOR circuitry.
D. The pharyngeal reflexes are tested by stimulating the pharynx and esophagus
by passage of a suction catheter into the back of the throat and down the nasogastric tube. Tests the integrity of CNs IX and X.
Consciousness 1048
Persistent Vegetative State
Persistent vegetative state is the complete unawareness of self and environment with the
persistence of some vegetative functions that involve the hypothalamus and brain stem. Patients may have signs of wakefulness and sleep; however, they cannot make meaningful behavioral responses other than to nociceptive stimuli. To be considered as a persistent state, the patient must meet criteria for at least one month. Although these patients are not comatose, they lack awareness of self and from this standpoint can be considered to be unconscious.
The causes of persistent vegetative state include acute traumatic and non-traumatic
injury, degenerative and metabolic disorders, and severe developmental malformations. A common cause of non-traumatic acute injury is the hypoxia. The most famous case of hypoxic encephalopathy and persistent vegetative state is Karen Ann Quinlan. Her parents obtained legal permission to discontinue ventilatory support, but after discontinuation she survived in a persistent vegetative state for the next nine years. The most common damage in persistent vegetative state involves the corex qith relative preservation of the hypothalamus and brain stem.
The persistent vegetative state is an unfortunate condition that can drain resources for the care
of an individual who is unlikely to make a meaningful recovery. We now realize that this condition does not dictate heroic efforts to maintain survival. Society is providing alternatives in allowing us to determine our fate if we should develop irreversible brain damage in the form of a living will.
Brain Death
Persistent
Locked-in
Vegetative State
Syndrome
Variable, may be
Problem Solving
1. The most common cause of coma is:
A. metabolic dysfunction (drugs or endogenous)
B. supratentorial lesions
C. pontine hemmorhages
D. medullary hemmorhage
E. spinal cord tumors
2. Which of the following occurs in locked in syndrome?
A. patient appears alert but has no meaningful cognitive responses
B. patient exhibits normal EEG
C. patient is unconscious
D. patient exhibits no brain stem reflexes
E. patient does not respond to pain
3. Which of the following occurs in coma?
A. patient appears alert but has no meaningful cognitive responses
B. patient exhibits normal EEG
C. patient is unconscious
D. patient exhibits no brain stem reflexes
E. patient has a flat EEG
4. Which of the following occurs in brain death?
A. patient appears alert but has no meaningful cognitive responses
B. patient exhibits normal EEG
C. patient has normal respiration
D. patient exhibits no brain stem reflexes
E. patient responds to pain
5. Which of the following occurs in persistant vegetative state?
A. patient appears alert but has no meaningful cognitive responses
B. patient exhibits normal EEG
C. patient is has abnormal respiration
D. patient exhibits no brain stem reflexes
E. patient has abnormal sleep-wake cycles
6. Which of the following statements is FALSE?
A. without input from the thalamus, consciousness is not maintained
B. the final seat of consciousness lies in the cortex
C cells in the locus coeruleus produce norepinephrine and project diffusely and widely to cortex
D. cells in the raphe nuclei produce serotonin and project diffusely and widely to cortex
E. the ARAS does not play a role in the sleep-wake cycle
7. Which of the following statements is FALSE?
A. coma follows central herniation involving the diencephalon
B. there can be pupillary and eye movement problems following central herniation
C. a lesion of the spinal cord does not result in coma
D. "locked in" syndrome results from bilateral damage to descending corticospinal and
corticobulbar pathways within the basilar (ventral) pons
E. the ARAS is involved in the "locked in" syndrome
8. Which of the following statements is FALSE regarding the clinical deficits that can result
from a cortical mass in the LEFT uncal herniation?
A. right hemiplegia
B. dilated pupil in the left eye
C. left hemiplegia
D. it would be possible to have quadriplegia
E. damage to the midbrain would never lead to coma
9. Which of the following statements is FALSE about brain death?
A. absence of gag reflex
B. wide range of abnormalities in EEG
C. absence of respiration
D. no sleep wake cycle
E. absence of vestibulo-ocular reflex upon caloric stimulation
10. Which of the following statements is TRUE about the lesion shown here?
A. the patient is in a coma
B. the patient can speak
C. the patient can move
D. the patient is in a persistent vegetative state
E. the patient has normal sleep and wake patterns because there is no damage to the ARAS.
11. Which of the following statements is FALSE about the persistent vegetative state?
A. patient can sometimes appear wakeful
B. respiration is normal
C. patient exhibits sleep/wake cycles
D. flat EEG
E. none of the above are FALSE
12. Which of the following statements is FALSE regarding locked-in syndrome?
A. normal respiration
B. normal sleep/wake cycles
C. normal EEG
D. spasticity
E. tongue deviates to the right upon protrusion
13. Fill in the blanks in the table below.
Coma
Persistent
Locked-in
Vegetative State
Syndrome
Variable, may be
14. Which of the following statements is TRUE?
A. the arms are flexed in decerebrate rigidity
B. the legs are flexed in both decerebrate and decorticate rigidity
C the lesion lies rostral to the red nucleus in decerebrate rigidity
D. the lesion lies between the superior and inferior colliculi in decorticate rigidity
E. none of the above is TRUE
15. In brain death:
A. the gag reflex is normal
B. the corneal reflex is normal
C. the pupillary light reflex is normal
D. the VOR is normal
E. none of the above is TRUE
16. Which of the following is TRUE regarding Kernohan's notch?
A. Babinski would occur contralateral to it
B. lies ipsilateral to the dilated pupil
C. seen is uncal herniations
D. is a notch in the internal capsule
E. two of the above are TRUE

17. Which of the following associations is/are correct regarding the four different stages of
damage shown here?
A. in A there are normal calorics
B. in B there is decerebrate rigidity
C. in C the pupils are meiotic
D. in D pupils are dilated
E. in A the pupils are constricted
18. Which of the following associations is/are correct regarding the four different stages of
damage shown above?
A. in A, B, C, and D there is coma
B. in B there is decorticate rigidity
C. in C caloric stimulation of the right horizontal SS canal with warm water results in movement
of the right eye to the left
D. in D pupils are reactive to light
E. two of the above are TRUE
Problem solving ANSWERS
PROBLEM SOLVING ANSWERS
1. A
13. see chart 18. E (A and B)
Source: http://www.neuroanatomy.wisc.edu/coursebook/neuro11(2).pdf
ZÉRO ATTENTEZÉRO PAPERASSEUN SERVICE EXPRESS EN CAS D'URGENCE avec votre inscription Une allocation d'études en cas SÉCURITÉ SOCIALE ÉTUDIANTE d'échec à vos examens Si vous êtes obligé(e) de redoubler votre année Mutuelle étudiante de proximité membre du Réseau national emeVia car vous ne pouvez pas vous présenter à vos
Journal of Chinese Medicine • Number 91 • October 2009 The treatment of Elevated FSH Levels with Chinese Medicine The treatment of Elevated FSH Levels with Chinese Medicine Follicle stimulating hormone (FSH) levels are routinely tested during biomedical investigations into female fertility. An appropriately low FSH level is frequently required by fertility clinics as an entry requirement for women wishing to receive assisted reproductive technology (ART) treatment such as in vitro fertilisation (IVF). This article