Untitled
European Heart Journal (2011) 32, 2499–2506
Novel therapeutic concepts
Hypertension management 2011: optimalcombination therapy
Peter S. Sever 1* and Franz H. Messerli 2
1International Centre for Circulatory Health, Imperial College London, 59 North Wharf Road, London W2 1LA, UK; and 2Division of Cardiology, St Luke's and Roosevelt Hospitals,Columbia University College of Physicians and Surgeons, New York, NY, USA
Received 11 August 2010; revised 16 March 2011; accepted 13 May 2011; online publish-ahead-of-print 22 June 2011
Raised levels of blood pressure result from the complex interplay of environmental and genetic factors. The complexity of blood pressurecontrol mechanisms has major implications for individual responsiveness to antihypertensive drugs. The underlying haemodynamic disorderin the majority of cases is a rise in peripheral vascular resistance. This observation led to the discovery and development of increasinglysophisticated and targeted vasodilators, although many of the earlier antihypertensive drugs, by virtue of their actions blocking the sympath-etic nervous system, had a vasodilator component to their mode of action. A recent meta-analysis of placebo controlled trials of monother-apy in unselected hypertensives, reports average (placebo-corrected) blood pressure responses to single agents of 9.1 mmHg systolic and5.5 mmHg diastolic pressure. These average values disguise the extremely wide ranging responses in individuals across a fall of 20 – 30 mmHg
systolic at one extreme, to no effect at all, or even a small rise in blood pressure at the other. The second factor determining individualresponses to monotherapy is the extent to which initial falls in pressure are opposed by reflex responses in counter regulatory mechanismsthat are activated following the blood pressure reduction. Thus, a satisfactory blood pressure response is rarely reached with monotherapyalone. What then is the next step if blood pressure is not a goal after the patient has been treated with monotherapy for a few weeks? Shouldyou uptitrate, substitute or combine?
Hypertension † Combination therapy
earlier antihypertensive drugs, by virtue of their actions blockingthe sympathetic nervous system, had a vasodilator component to
Raised levels of blood pressure result from the complex interplay
their mode of action. The first non-specific vasodilator, hydrala-
of environmental and genetic factors leading to the activation or
zine, was followed by vasodilatation which involved blockade
suppression of one or more of a host of physiological systems
of calcium channels on vascular smooth muscle cells [the
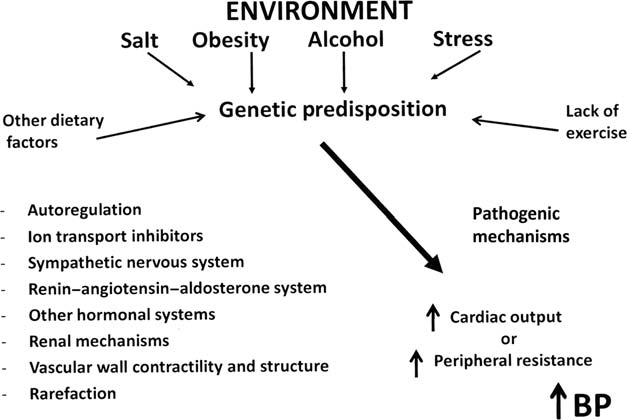
involved in blood pressure regulation (Figure The complexity
calcium channel blockers (CCBs)], blockade of post-synaptic
of blood pressure control mechanisms, first hypothesized by
alpha-adrenoceptors on peripheral sympathetic neurones (the
Irvine Page,has major implications for individual responsiveness
to antihypertensive drugs (Figure ), because of the inevitable
blockade of the renin – angiotensin – aldosterone system (RAAS)
variety of hypertensive phenotypes, the identification of which,
[angiotensin-converting enzyme (ACE) inhibitors, angiotensin
with some notable exceptions, remains elusive to the practicing
receptor blockers (ARBs), direct renin inhibitors (DRIs)] (Figure
physician involved in making treatment decisions for individual
The nature of these molecules, and in most cases their single site
of action, dictates that when administered to a heterogeneous
Hypertension is, by definition, a haemodynamic disorder. The
population, encompassing many hypertensive phenotypes, blood
major haemodynamic finding associated with higher levels of
pressure responses will be largely unpredictable and wide
blood pressure is a rise in peripheral vascular resistance. This
ranging (Figure ). If, in a particular case, blood pressure levels
observation led to the discovery and development of increasingly
are largely determined by activation of the RAAS, for example in
sophisticated and targeted vasodilators, although many of the
renal artery stenosis, marked falls in blood pressure with
* Corresponding author. Tel: +44 207 594 1100, Fax: +44 207 594 1145, Email: Published on behalf of the European Society of Cardiology. All rights reserved. & The Author 2011. For permissions please email:
[email protected]
P.S. Sever and F.H. Messerli
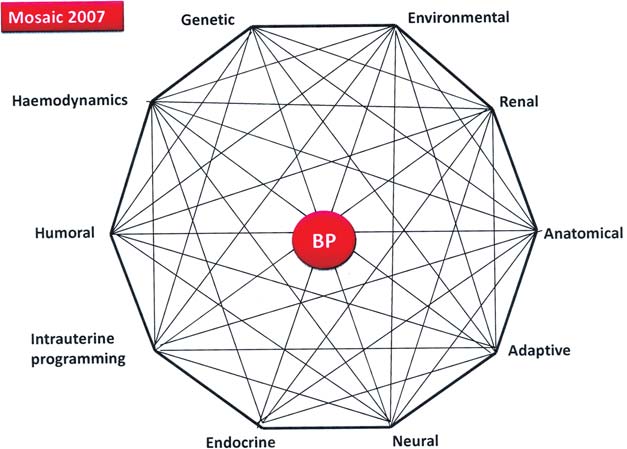
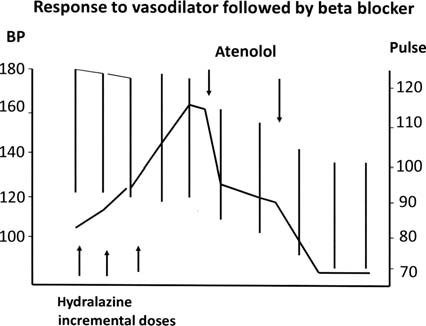
Figure 1 A schematic to demonstrate the interaction of environmental factors with underlying genetic predisposing factors to increase bloodpressure through the activation of a variety of pathogenetic mechanisms.
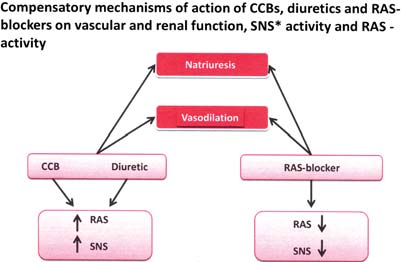
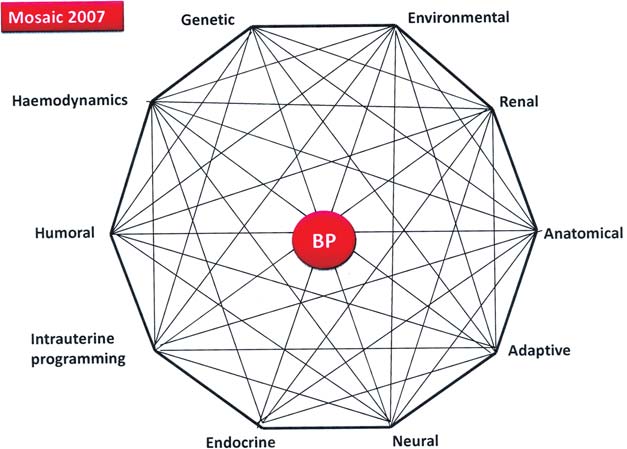
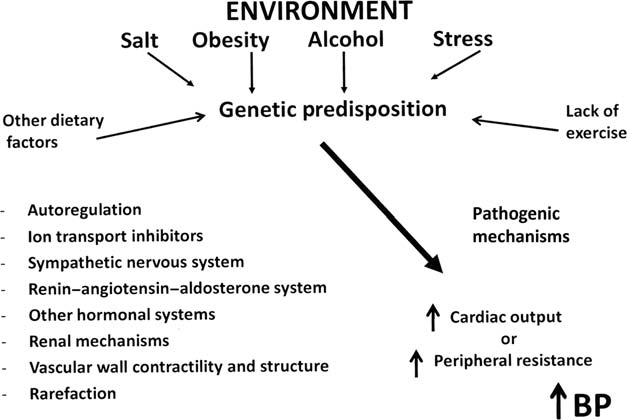
Figure 2 A modified and updated mosaic theory of blood pressure regulation derived from the original Paige mosaic.
impairment of renal function may follow the administration of an
systolic and 5.5 mmHg diastolic pressure. These average values dis-
ACE-Inhibitor.On the other hand, in the elderly and in those
guise the extremely wide ranging responses in individuals across a
of African origins, where the activity of the RAAS is generally sup-
fall of 20 – 30 mmHg systolic at one extreme, to no effect at all, or
pressed, blood pressure reductionswith an ACE-Inhibitor may
even a small rise in blood pressure at the (Figure
be small. In general, however, the phenotype is not known.
The second factor determining individual responses to mono-
A recent meta-analysis of placebo-controlled trials of monother-
therapy is the extent to which initial falls in pressure are
apy, in unselected hypertensives,reports average (placebo cor-
opposed by reflex responses in counter regulatory mechanisms
rected) blood pressure responses to single agents of 9.1 mmHg
that are activated following the blood pressure reduction. In
To uptitrate, to substitute, or to combine drugs
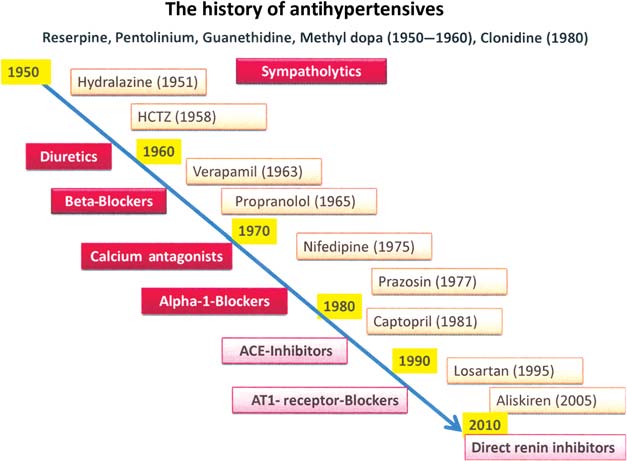
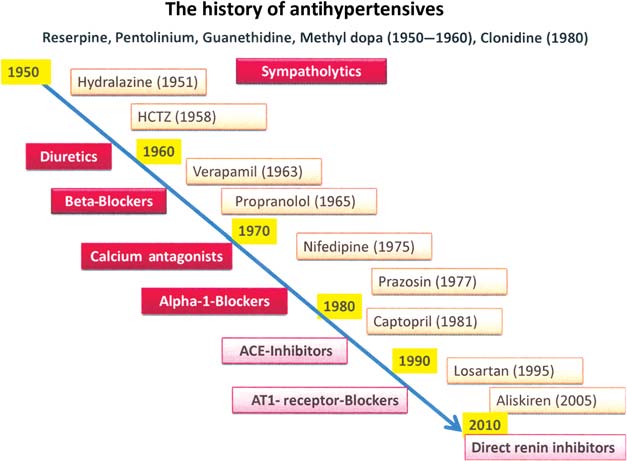
Figure 3 The history of development of antihypertensive drugs reproduced with kind permission of Thomas Unger.
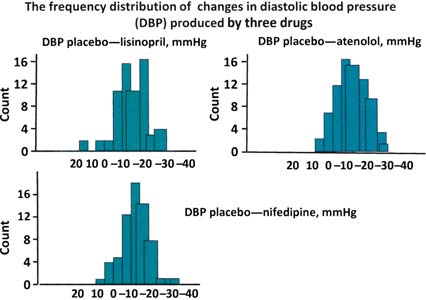
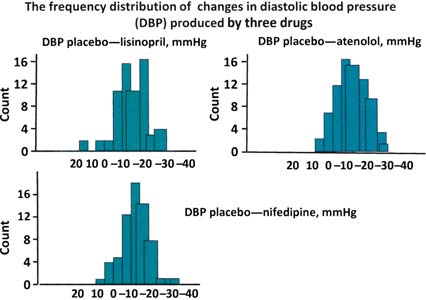
Figure 4 The frequency distribution of changes in diastolicblood pressure produced by three different antihypertensive
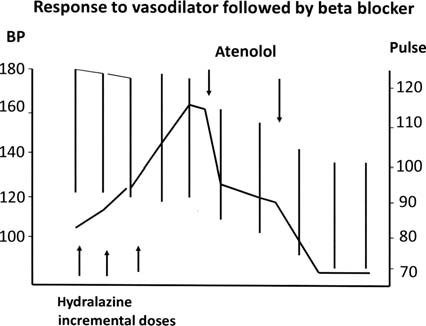
Figure 5 Response to the vasodilator hydralazine followed by
drugs. Negative values represent placebo-corrected reductions
the co-administration of the beta-blocker, atenolol.
in diastolic pressure. Modified from reference.
antihypertensive drugs have a rather shallow dose – response
extreme cases, these reflex responses can nullify any fall in
curve. In particular, with RAAS inhibitors doubling the dose has
pressure (Figure
minimal incremental effect on blood pressure. In contrast, with
Thus, a satisfactory blood pressure response is rarely reached
CCBs, additional antihypertensive efficacy can be gained when, for
with monotherapy alone. What then is the next step if blood
example, the starting dose of amlodipine is doubled from 5 to
pressure is not at goal after the patient has been treated with
10 mg. However, the incidence of pedal oedema also is dose depen-
monotherapy for a few weeks? Should you uptitrate, substitute,
dent and increases with a higher dose of amlodipine. Importantly, the
additional blood pressure fall from combining drugs from two differ-ent classes is �5 times greater than the one from doubling the dose
of a single drug.Thus, the odds of getting blood pressure to goal are
Uptitration of the initial drug is reasonable only if definitive,
several times greater with combining drugs than with up titration of
enhanced antihypertensive efficacy of the higher dose has been
monotherapy. From a sheer efficacy point of view, combination
documented and the cost is not prohibitive. Regrettably, most
therefore takes precedence over uptitration.
P.S. Sever and F.H. Messerli
Although there are some differences between guidelines, several
now recommend the initiation of combination therapy as first line
Substituting an antihypertensive drug from a different class should be
in particular circumstances, in view of the associated risks of more
considered only if there is no antihypertensive effect with a reason-
severe hypertension, the recognition that dual (or triple therapy) is
able dose, as is occasionally observed with beta-blockers or RAAS
invariably needed to achieve target blood pressures of ,140/
blockers in black patients, or if there are any intolerable adverse
90 mmHg, and that there is a degree of urgency in reducing
effects such as angioedema. Fortunately, most modern antihyperten-
blood pressure to more acceptable levels to combat this risk.
sive drugs are generally well tolerated and serious adverse effects are
JNC-7 recommends initiating therapy with two drugs when
few. However, before resorting to drug substitution one may con-
blood pressure is .20 mmHg above systolic goal or 10 mmHg
sider that the addition of another drug may unmask the antihyperten-
above diastolic The European including their
sive efficacy of the initial agent. For instance, the addition of a thiazide
most recent updaconfirm such a recommendation and also
diuretic in a patient previously unresponsive to RAAS blockade is
proposes the initiation of combination therapy in those with
prone to stimulate the renin – angiotensin system to the extent
milder degrees of blood pressure elevation in the presence of mul-
that now both drugs, the RAAS inhibitor as well as the diuretic,
tiple risk factors, subclinical organ damage, diabetes, renal, or
have an additive antihypertensive
associated cardiovascular disease. Although combination therapyis not specifically advocated as initial therapy in the 2004 British
Rationale for combination therapy
Hypertension Society (largely based on the fact thatthere is a lack of randomized controlled trial evidence to
The rationale for combination therapy in hypertension is therefore
support such practice), it is probable that the results of ongoing
straightforward. First, it is to combine drugs acting on different
trials will provide new evidence in favour of their early introduc-
physiological systems in a situation where the phenotype is not
tion into treatment strategies.
known and where a pharmacological ‘attack' on two (or more)
Inevitably, there are concerns that initiating therapy with more
systems will have a greater impact on blood pressure reduction
than one drug could induce significant hypotension and increase
than blind monotherapy. Second, it is an attempt to block counter-
coronary risk. An analysis of intervention trials in hypertension
regulatory responses that are activated by the perturbation of the
provides some evidence for a ‘J-curve' relationship between the
blood pressure regulatory mechanisms when a physiological
magnitude of blood pressure lowering and coronary heart
system is blocked with single-drug therapy (Figure ).
disease outcome, but this seems to be confined to high-risk indi-
Third, the hypertensive population includes many with levels of
viduals including those with established coronary artery disease,
blood pressure categorized as moderate or severe (stage 2 hyperten-
in whom excessive blood pressure lowering compromises coron-
sion).There is general consensus that those with systolic blood
ary perfusion. In uncomplicated hypertension, lower pressures are
pressures .160 mmHg and/or diastolic pressures .100 mmHg fall
well tolerated, for example, as seen in the Systolic Hypertension in
into this category. They constitute 10– 15% of hypertensive popu-
the Elderly Study, in which diastolic pressures as low as 60 mmHg
lations and are at substantially greater risk of a future cardiovascular
were achieved in the active treatment group.Ongoing trials com-
event. For every 20 mmHg increase in systolic blood pressure,
paring initiation of dual therapy vs. sequential monotherapy in
there is an approximate doubling of cardiovascular risk
hypertension will aim to clarify the safety of the former.
Obviously the proportion of the population with hypertension
Fourth, blood pressure variability has been shown to decrease
increases with age and this also applies to those with stage 2 hyperten-
with combination therwhen compared with monotherapy.
sion. As age advances systolic hypertension predominates and is
In an extensive analysis of several randomized trials, visit-to-visit
largely accounted for by loss of elasticity and increasing rigidity of
variability of systolic blood pressure was documented to be a
large arteries.
strong predictor of both stroke and myocardial infarction andthis was independent of mean in-trial blood pressure.Interest-ingly enough, CCBs and diuretics were most efficacious in reducingvisit-to-visit blood pressure variability and also were associatedwith the most efficacious stroke prevIn contrast, beta-blockers were shown to increase variability of systolic pressurein a dose-dependent way and also were the least efficacious instroke prevention. The addition of a CCB or to a lesser extentof a diuretic to a RAAS inhibitor diminishes variability of systolicpressure, which makes another strong argument for combinationtherapy.
Trial evidence for and against
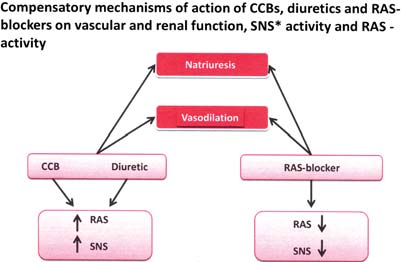
Figure 6 Renin– angiotensin – aldosterone system and sym-
specific combinations
pathetic nervous system activation and suppression by different
An extensive review of first-line drug choices has been published
classes of antihypertensive drugs.
To uptitrate, to substitute, or to combine drugs
Collaborationand is based upon prospective meta-analyses of
cardiovascular outcome, and differentially affected by different
trials comparing different drug regimens. Similar analyses have been
treatment strategies. For example, in the CAFE´ substudy of
undertaken by the National Institute for Clinical Excellence (NICE)
ASCOT, the amlodipine/perindopril regimen lowered central
in the The difficulty in extending these analyses to evaluate
aortic blood pressure to a greater extent than the atenolol/thia-
the comparative effects of different combinations of drugs is that in
zide regimen (by 4 mmHg systolic), and the level of central
many trials it is not possible to establish which add-on drugs were
pressure was related to cardiovascular and renal outcomesIn
used and in what doses. The evidence base for making claims about
another substudy, various measures of blood pressure variability
the comparable or superior efficacy of one regimen vs. another
during the trial were strongly associated with both stroke and
comes from trials where the treatment algorithm was clearly
coronary outcomes, in that the amlodipine-based treatment
defined and one could conclude with reasonable assuredness
regimen reduced blood pressure variability compared with the
that a particular regimen was similar to, better than or worse
atenolol-based regimen. These differences largely accounted for
than another. The best evidence, from which claims can be
the observed differences in cardiovascular outcomes between
made of outcomes in favour of a particular regimen, comes from
the two-drug regimen
four trials, the Losartan Intervention For Event Reduction Trial
In the third trial, ACCOMPLISH,11 506 hypertensive patients
(the LIFE the Anglo-Scandinavian Cardiac Outcomes Trial
were randomized to a combination of the ACE-Inhibitor, benaze-
(ASCOThe Avoiding Cardiovascular Events through Combi-
pril, with either hydrochlorothiazide, or the CCB, amlodipine.
nation Therapy in Patients Living with Systolic Hypertension Trial
Patients were followed for 3 years. Blood pressure levels were
(ACCOMPLISH)and the Valsartan Antihypertensive Long-term
reduced similarly in the two arms of the trial. Cardiovascular
Use Evaluation Trial (VALUE).
events were significantly reduced by 20% in benazepril/amlodipine
In the LIFE 9193 hypertensive patients were random-
arm compared with the benazepril/hydrochlorothiazide arm.
ized to initial treatment with either an ARB (losartan) or a beta-
Myocardial infarction was reduced significantly (22%) and stroke
blocker (atenolol). Hydrochlorothiazide was added in the
non-significantly (16%) by benazepril/amlodipine compared with
majority of patients to achieve blood pressure control, along
benazepril/hydrochlorothiazide. The benefits of the benazepril/
with the further addition of common third-line agents in a min-
amlodipine combination over benazepril/hydrochlorthiazide were
ority of patients. After an average follow-up of 5 years during
seen in both diabetic and non-diabetic pat
which there was no discernable difference in blood pressure
In the fourth study, VALUE,15 245 hypertensive patients
between the two regimens, the composite primary cardiovascu-
were randomized to either the ARB, valsartan, or the CCB,
lar endpoint was reduced by 13% in the losartan-based group
amlodipine. Hydrochlorothiazide was added to each limb in
compared with the atenolol-based group. The major benefit
attempting to achieve goal blood pressures. Other add-on
was seen in the secondary stroke endpoint (a component of
drugs were similar in the two treatment arms. Mean follow-up
the primary) which was reduced by 25% in the losartan-based
was 4.2 years. Blood pressures were more effectively and more
rapidly reduced in the amlodipine-based treatment arm. Although
In the second trial, ASCOTover 19 000 hypertensive patients
the primary composite endpoint of cardiac morbidity and mor-
with no prior history of coronary heart disease were randomized
tality was similar in the two arms of the trial, myocardial infarc-
to either a CCB, amlodipine, or a beta-blocker, atenolol. The
tion occurred significantly less frequently (risk reduction 19%)
ACE-Inhibitor perindopril or the diuretic bendroflumethiazide
and strokes non-significantly less often (risk reduction 15%) in
was added to each arm, respectively, in an attempt to achieve
blood pressure targets. Again, common third-line drugs could be
valsartan-based arm. The authors of the trial attributed early
added to each arm in a minority of patients. After an average
differences in blood pressure as an explanation for the differential
follow-up of 5.5 years, the trial was stopped prematurely on the
effects of the two treatments on myocardial infarction and
advice of the Data Safety Monitoring Committee, because of
highly significant outcome benefits in favour of the amlodipine-
The cumulative evidence from these trials strongly supports the
based regimen. All cardiovascular events were reduced by 26%,
view that, in hypertensive patients, combination therapy with CCB/
stroke by 23%, and all-cause mortality by 11% by the amlodipine-
ACE-I or CCB/ARB is likely to be associated with better cardiovas-
based regimen compared with the atenolol-based regimen. The
cular outcomes, including myocardial infarction and stroke, than
primary endpoint of non-fatal myocardial infarction and fatal cor-
regimens containing beta-blockers and thiazide diuretics and that
onary disease was reduced non-significantly by 10% in favour of
CCB/ACE-I combinations are preferable to diuretic/ACE-I combi-
the amlodipine-based regimen, best explained by the early termin-
nations on major cardiovascular endpoints. Added to this should
ation of the trial before the required number of primary endpoints
be the cost-effectiveness analysis from the NICE Guidelines
had been reached. In the event, a more comprehensive coronary
which clearly demonstrates that CCBs and ACE-Is or ARBs are
more cost-effective treatment choices than beta-blockers or
reduced significantly by 13%.
thiazide diuretics.
In several subsequent analyses, the small blood pressure differ-
The above recommendations apply, in general, to those subjects
ences observed early in the trial did not explain the outcome
with uncomplicated hypertension. In hypertensives with associated
benefits in favour of amlodipine-based treatment.In recent
cardiovascular disease such as heart failure or coronary heart
reports, however, it has been shown that additional haemo-
disease, the guidelines are consistent in recommending specific
drugs with compelling indications, based on randomized controlled
P.S. Sever and F.H. Messerli
trial evidence, that should be incorporated into treatment
therefore be the preferred agent to be combined with a RAAS
blocker. Unfortunately most RAAS inhibitors are available only ina fixed-dose combination (FDC) with hydrochlorthiazide.
Specific drug combinations
In a recently reported study in a very elderly (.80 years) hyper-
tensive population, the Hypertension in the Very Elderly Study
Given that there are seven major classes of antihypertensive drugs
a thiazide-like diuretic, indapamide, to which an
and numerous members of each class, the number of possible
ACE-Inhibitor, perindopril, was added, was found to reduce
combinations is extensive. In the following, we subdivide combi-
stroke incidence (30%) and the incidence of heart failure (64%),
nations as preferred, acceptable or unacceptable/ineffective combi-
compared with placebo.
nations, based on outcome, antihypertensive efficacy, safety, and/ortolerability.
Acceptable combinationsBeta-blockers and diuretics
Preferred combinations
The addition of diuretics has been shown to improve the antihy-
Renin – angiotensin – aldosterone system inhibitors
pertensive efficacy of beta-blockers in African-American patients
and calcium channel blockers
and other populations with low-renin hypertension. However,
Additive blood pressure reduction has been documented with the
both of these drug classes have been shown to have similar
combination of an ACE-Inhibitor, ARB, or DRI with a CCB. The
adverse effects in that they increase the risk of glucose intolerance,
common dose-dependent adverse effect of CCB monotherapy is
the development of new-onset fatigue, and sexual dys-
peripheral oedema. The addition of a RAAS blocker has been
function. Outcome studies have shown a morbidity and mortality
shown to mitigate this adverse effect. A recent meta-analysis has
reduction with diuretics and beta-blockers in combinat
shown that ACE-Inhibitors are somewhat more efficacious thanARBs in decreasing peripheral oedema associated with CCB
Calcium channel blockers and diuretics
therapy.As stated above, the ACCOMPLISH trial showed that
Most physicians are somewhat reluctant to combine a CCB with a
fixed combination of an ACE-Inhibitor (benazapril) with a CCB
diuretic. However, in the VALUE hydrochlorthiazide was
(amlodipine) was more beneficial with regard to morbidity and
added as a second step in patients randomized to amlodipine
mortality reduction than the fixed combination of the same
and the diuretic/CCB combination was well tolerated, although
ACE-Inhibitor with hydrochlorthiazide.Generally, similar end-
there was a higher risk of new onset diabetes and hyperkalaemia
point reductions have been demonstrated with ACE-Inhibitors
when compared with the valsartan arm. Nevertheless, morbidity
and ARBs, although there is a suggestion that ACE-Inhibitors
and mortality reductions were at least as good in the amlodipine
may be slightly more cardioprotective and that ARBs may confer
as in the valsartan arm of the VALUE study.
some advantages in stroke prevention.
The International Verapamil-Trandolapril Study was
Calcium channel blockers and beta-blockers
a comparison of ‘new' vs. ‘old' drugs in that a regimen of the non-
The combination of a beta-blocker with a dihydropyridine CCB
dihydropyridine, verapamil, to which trandolapril was added if
has additive blood pressure reduction and, in general, is well toler-
necessary, was compared with atenolol to which hydrochlorthia-
ated. In contrast, beta-blockers should not be combined with non-
zide was added if necessary to achieve blood pressure goals. A
dihydropyridine calcium blockers such as verapamil or diltiazem.
total of 22 576 hypertensives with established coronary artery
The negative chronotropic effect of both of these drugs may
disease were enrolled and followed up for a mean of 2.7 years.
result in heart block or bradycardia.
The combined cardiovascular outcome was similar in the twogroups. Perhaps the most logical explanation for these findings is
Dual calcium channel blockade
that the disadvantage of the beta-blocker regimen observed in
The combination of a dihydropyridine CCB with either verapamil
hypertension trials in uncomplicated patients was offset by the
or diltiazem has been shown in a recent meta-analysis to have
known advantages of beta blockade in the context of established
an additive effect on blood pressure lowering without significantly
coronary artery disease.
increasing adverse events. Dual CCB blockade may be useful inpatients with documented angioedema on RAAS inhibitors or in
Renin – angiotensin – aldosterone system inhibitors
patients with advanced renal failure at risk for hyperkalaemia.
However, no outcome data are available with dual CCB therapy
Numerous factorial design studies have shown that the combi-
and long-term safety remains undocumented.
nation of a thiazide diuretic with an ACE-Inhibitor, an ARB, or aDRI result in fully additive blood pressure reduction. Diuretics,
by depleting intravascular volume, activate the RAAS which
Dual renin – angiotensin – aldosterone system blockade
causes salt and water retention as well as vasoconstriction. The
For the treatment of hypertension per se, dual RAAS blockade, in
addition of a RAAS blocker attenuates this counter regulatory
general, is not recomIn the ONTARGET study,there
response. Moreover, diuretic induced hypokalaemia as well as
were more adverse events with a combination of telmisartan and
glucose intolerance is mitigated by the addition of a RAAS
ramipril than with individual agents and cardiovascular endpoints,
blocker. Chlorthalidone has been shown to be more effective
despite a small additional blood pressure reduction, were not
than hydrochlorthiazide in reducing blood pressure and should
improved compared with monotherapy. Thus, there is little if any
To uptitrate, to substitute, or to combine drugs
reason to combine an ARB with an ACE-Inhibitor for the treatment
of hypertension. However, as blockade of the renin – angiotensincascade by either an ACE-Inhibitor or an ARB increases plasma
The adverse reactions associated with combination treatments are
renin activity, the argument has been put forward that the addition
largely predicted from the known side effects of the individual
of a DRI could have additional benefits. Indeed, the combination of
components. However, in older combinations of vasodilators
aliskiren with an ARB has been shown to have a small, significant
(hydralazine) with beta-blockers and diuretics, the side effects of
additional effect on blood pressure in a double-blind study of 1797
vasodilatation (tachycardia and fluid retention) were mitigated by
patients.However, this fall in blood pressure with dual RAAS
the additional drugs. There is some evidence that the oedema
blockade was less than one would have expected by the addition
commonly associated with dihydropyridine CCBs is partially
of either a thiazide diuretic or a CCB. Of note, in an open label pro-
relieved by co-administration of RAAS blockerand RAAS
spective crossover study in patients with resistant hypertension, the
blockers may reduce the incidence of hypokalaemia induced by
aldosterone antagonist spironolactone was shown to lower blood
On the other hand, it seems likely that the increase
pressure more effectively than conventional dual RAAS blockade.
in incidence of new-onset diabetes commonly associated with
At the present time, no outcome data are available to support
beta-blockers is exacerbated when these drugs are given in con-
benefits of the combination of a DRI with either an ACE-Inhibitor
junction with thiazide diuretics. A meta-analysis of the increased
or an ARB. Nevertheless, a randomized double-blind trial (ALTI-
incidence of new-onset diabetes with beta-blocker and thiazide
TUDE) has been designed to look into this question and is currently
treatment, compared with ‘newer' drugs, is provided by the
in progress.
NICE Guidelines.
These conclusions assume that there are no differences
between individual drugs within a particular drug class in relation
Renin – angiotensin – aldosterone system blockers
to their effects on long-term morbidity and mortality. Among
and beta-blockers
the CCBs, the best evidence is for amlodipine. Among the
In patients having suffered a myocardial infarction or in those in
ACE-Is and ARBs, several different drugs have been used both
heart failure, these two drug classes are commonly combined
within and without combination trials in hypertensive patients
because both have been shown to reduce reinfarction rates and
and in other cardiovascular patient groups, and no clear benefits
to improve survival. However, their combination produces little
of one drug over another are evident. For thiazide and thiazide-like
additional blood pressure reduction compared with either mono-
diuretics, there persists an opinion that the evidence base for long-
therapy. Thus, for the treatment of blood pressure per se, there is
term benefits is best for moderate doses of chlorthalidone,
no reason to combine these two drug classes.
compared with other thiazides in lower doses. Regrettably, thereare unlikely to be future trials comparing drugs within this class.
Beta-blockers and antiadrenergic drugs
For the beta-blockers, atenolol has been the drug most often
Little if any antihypertensive efficacy can be gained when beta-
used and claims have been made that had other drugs in this
blockers are combined with antiadrenergic drugs such as clonidine.
class been used in the trials then perhaps different results would
In fact, an exaggerated rebound in BP has been observed with this
have occurreThis is unlikely since the adverse effects of ateno-
lol, observed in ASCOT, on blood pressure variability,and anincrease in central aortic pressures compared with amlodipine
Other drug classes in combination therapy: alpha-blockers
(both of which were associated with an increase in cardiovascular
and spironolactone
risk), would be likely to occur with most other beta-blockers.
Alpha-adrenoceptor antagonists have been widely used as add-on
Outcome trials in hypertension with beta-blockers possessing
drugs in combination regimens to achieve target blood pressures.
additional pharmacological properties have not been conducted.
The availability of extended release formulations has improvedtheir tolerability profile. Data from an observational analysis ofthe ASCOT trial showed that doxazosin gastrointestinal thera-peutic system (GITS) used as third-line therapy lowered blood
Fixed-dose combinations and
pressure and caused a modest reduction in serum In con-
trast to earlier findings in ALLHAT,doxazosin use in ASCOT wasnot associated with an increased incidence of heart failure.
In a recent review of the potential advantages of FDC formulations
For subjects with resistant hypertension, defined as failure
over their corresponding free drug components given separately, it
to achieve target blood pressure (,140/90 mmHg) despite
was shown that the FDCs were associated with significantly better
maximum doses or maximum tolerated doses of three antihyper-
compliance and a non-significant improvement in persistence with
tensive drugs including a RAAS blocker, a CCB, and a thiazide
treaSimilarly, in a meta-analysis of nine studies comparing
diuretic, quadruple therapy is frequently required. Recent reports
the administration of FDCs with their separate components, the
demonstrate that spironolactone added to triple therapy is associ-
adherence rate was improved by 26% in patients receiving FDCs.
ated with substantial further reductions in blood pressure of,
In trials in which blood pressure data were reported, use of
on average, 22/9.5 Spironolactone is therefore rec-
FDCs was associated with a non-significant lowering of systolic
ommended as a component of combination therapy in patients
and diastolic pressure (4.1 and 3.1 mmHg, respectively) compared
with resistant hypertension.
with the corresponding drugs administered separately.Such
P.S. Sever and F.H. Messerli
differences in blood pressure if sustained long term wouldundoubtedly confer advantages on cardiovascular outcomes.
Drug combinations in hypertension:
Blood pressure control in practice
Worldwide surveys of blood pressure control to targets rec-
ommended by national and international guidelines have consist-
ently revealed that in clinical practice the conventional goal of a
blood pressure ,140/90 mmHg is reached by only a minority of
patients.Data from several countries are shown in Figure .
While there are several explanations for physicians failing to
achieve target blood pressures, including poor compliance or con-
cordance with drug taking by patients, white coat hypertension,
undiagnosed secondary causes of hypertension, and true resistant
Renin inhibitor/diuretic
hypertension, in the majority of cases therapeutic inertia on the
Renin inhibitor/CCB
part of the physician plays a major role. There is good evidence
Dihydopyridine CCB/non-dihydropyridine CCB
that when physicians are faced with patients on treatment for
hypertension, but who have not reached goal blood pressures,
they are reluctant to increase drug doses or initiate second- and
Renin inhibitor/ARB
third-line combination therapy.
The issues surrounding these observations are complex. Clearly
lack of education and failure to appreciate the importance of
lowering blood pressure to targets to prevent cardiovascular
Centrally acting agent/beta-blocker
outcomes associated with uncontrolled blood pressure are impor-tant issues. The historical focus on diastolic pressure as the basisfor initiation of therapy and as a treatment target is another. Inpractice, diastolic targets of ,90 mmHg are far more commonly
often the norm rather than the exception. In hypertension, the
attained than systolic targets of ,160 mmHg.
underlying rationale for combination therapy is somewhat differ-
Lastly, and importantly, true therapeutic inertia—the reluctance
ent. Since we do not know the cause of the blood pressure
to change medications when faced with a patient whose blood
elevation, therapy is essentially blind and a shotgun approach
pressures remain above goals. Excuses such as the following
may be more efficacious than targeted therapy. This is particularly
example—‘It's a little bit higher today (cold weather, rush to
true because monotherapy invariably triggers a variety of counter
clinic, stress at work, domestic problems etc) but we will see
regulatory mechanisms which are mitigated by combination
what it's like in a few weeks/months time' are all too frequent.
therapy. Thus, a strong case can be made for the early introduction
This major problem can be overcome (as we observe in trials)
of combination therapy and conceivably, the time will come when
when physicians or nurses are obliged to follow goal directed
combination therapy in low doses will be the preferred option for
treatment algorithms dictated by a trial protocol, and when
first-line treatment in patients with hypertension.
‘excuses' cannot be made to avoid changes in medications whenblood pressures are not at target.
Take home message and
An alternative scheme, practised in the UK since 2004, has been
to remunerate doctors based on the extent to which they achieve
(1) Many, if not most patients, need two or more drugs from
a number of clinical targets, one of which is dictated by the pro-
different classes to achieve blood pressure control.
portion of their hypertensive patients whose blood pressures are
(2) Combination therapy should be initiated if the patient's blood
lowered to an audit standard of ,150/90 mmHg. This has contrib-
pressure is .20/10 mmHg above target level unless cardiovas-
uted to improvements in the levels of blood pressure control in
cular status is brittle.
the population and has been accompanied by the increasing use
(3) Preferred or acceptable two drug combinations should be
of combination therapies.
(4) Whenever convenience and cost outweigh other consider-
ations fixed-dose combinations rather than individual drugs
The use of combinations of drugs in therapeutic practice is
should be used.
common place in contemporary medicine in a wide variety ofdisease categories, for example, in infectious disease, to cover mul-tiple organisms and to overcome drug resistance; in respiratory
Conflict of interest: P.S.S. has received grant income and honor-
illness such as chronic bronchitis or asthma to target multiple
aria from Pfizer and Servier. F.H.M. is an ad hoc consultant for the
pathophysiological mechanisms of disease and in neurological con-
following organizations: Novartis, Daiichi Sankyo, Pfizer, Takeda,
ditions to interfere with different abnormalities of neurotransmit-
F.H.M. received grant support from Forest, Daiichi
ter function. In fact throughout medicine, combination therapy is
Sankyo and Boehringer Ingelheim.
To uptitrate, to substitute, or to combine drugs
20. Blood Pressure Lowering Treatment Trialists' Collaboration. Effects of ACE
inhibitors, calcium antagonists, and other blood-pressure-lowering drugs; results
1. Page IH. The MOSAIC theory. In Page IH, ed. Hypertension Mechanisms.
of prospectively designed overviews of randomised trials. Lancet 2000;356:
New York: Grune and Stratton, 1987 p910 – 923.
1955 – 1964.
2. Sever PS. The heterogeneity of hypertension: why doesn't every patient respond
21. Blood Pressure Lowering Treatment Trialists' Collaboration. Effects of different
to every antihypertensive drug? J Hum Hypertens 1995;9:S33 – S36.
blood-pressure-lowering regimens on major cardiovascular events: results of
3. Mimran A, Ribstein J, Du Cailar G. Converting enzyme inhibitors and renal func-
prospectively-designed overviews of randomised trials. Lancet 2003;362:
tion in essential and renovascular hypertension. Am J Hypertens 1991;4(Suppl. 1):
1527 – 1535.
22. Nice guidelines. Management of hypertension in adults in primary care. 2004.
4. Dickerson JE, Hingorani AD, Ashby MJ, Palmer CR, Brown MJ. Optimisation of
antihypertensive treatment by cross-over rotation of four major classes. Lancet
23. Dahlof B, Devereux RB, Kjeldsen SE, Julius S, Beevers G, Faire U, Fyhrquist F,
1999;353:2008 – 2013.
Ibsen H, Kristiansson K, Lederballe-Pedersen O, Lindholm LH, Nieminen MS,
5. Matterson BJ, Reda DJ, Cushman WC. Department of Veterans Affairs.
Omvik P, Oparil S, Wedel H; LIFE Study Group. Cardiovascular morbidity and
Single-therapy of hypertension study. Revised figures and new data. Department
mortality in the Losartan Intervention For Endpoint reduction in hypertension
of Veterans' Affairs Cooperative Study Group on Antihypertensive Agents. Am J
study (LIFE): a randomised trial against atenolol. Lancet 2002;359:995 – 1003.
Hypertens 1995;8:189 – 192.
24. Dahlo¨f B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, Collins R,
6. Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treat-
Kjeldsen SE, Kristinsson A, McInnes GT, Mehlsen J, Nieminen M, O'Brien E,
ment with blood pressure lowering drugs: analysis of 354 randomised trials.
BMJ 2003;326:1427 – 1435.
Ostergren J; for the ASCOT Investigators. Prevention of cardiovascular events
7. Attwood S, Bird R, Burch K, Casadei B, Coats A, Conway J, Dawes M, Ebbs D,
with an antihypertensive regimen of amlodipine adding perindopril as required
Farmer A, Robinson J, Sherlock C. Within-patient correlation between the anti-
hypertensive effects of atenolol, lisinopril and nifedepin. J Hypertens 1994;12:
Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm
1053 – 1060.
(ASCOT-BPLA): a multicentre randomised controlled trial. Lancet 2005;366:
8. Wald DS, Law M, Morris JK, Bestwick JP, Wald NJ. Combination therapy versus
895 – 906.
monotherapy in reducing blood pressure: meta-analysis on 11,000 participants
25. Jamerson K, Weber MA, Bakris GL, Dahlo¨f B, Pitt B, Shi V, Hester A, Gupte J,
from 42 trials. Am J Med 2009;122:290 – 300.
Gatlin M, Velazquez EJ; ACCOMPLISH Trial Investigators. Benazepril plus amlo-
9. Jamerson KA. Rationale for angiotensin II receptor blockers in patients with low-
dipine or hydrochlorothiazide for hypertension in high-risk patients. NEJM
renin hypertension. Am J Kidney Dis 2000;36(Suppl. 1):S24 – S30.
2008;359:2417 – 2428.
10. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr,
26. Julius S, Kjeldsen SE, Brunner H, Hansson L, Platt F, Ekman S, Laragh JH,
Jones DW, Materson BJ, Oparil S, Wright JT Jr,, Roccella EJ; Joint National Com-
McInnes G, Schork AM, Smith B, Weber M, Zanchetti A; VALUE Trial. VALUE
mittee on Prevention, Detection, Evaluation, and Treatment of High Blood
trial: Long-term blood pressure trends in 13,449 patients with hypertension
Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure
and high cardiovascular risk. Am J Hypertens 2003;7:544 – 548.
Education Program Coordinating Committee. Seventh Report of the Joint
27. Poulter NR, Wedel H, Dahlo¨f B, Sever PS, Beevers DG, Caulfield M, Kjeldsen SE,
National Committee on Prevention, Detection, Evaluation, and Treatment of
Kristinsson A, McInnes GT, Mehlsen J, Nieminen M, O'Brien E, Ostergren J,
High Blood Pressure. Hypertension 2003;42:1206 – 1252.
Pocock S; for the ASCOT Investigators. Role of blood pressure and other
11. MacMahon S. Blood pressure and the risks of cardiovascular disease. In Swales JD,
ed. Textbook of Hypertension. Blackwell Scientific Publication, 1994, p46 – 57.
Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm
12. Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G,
(ASCOT-BPLA). Lancet 2005;366:907 – 913.
Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L,
28. Williams B, Lacy PS, Thom SM, Cruickshank K, Stanton A, Collier D, Hughes AD,
Rynkiewicz A, Schmieder RE, Struijker Boudier HA, Zanchetti A; European
Thurston H, O'Rourke M; CAFE Investigators; Anglo-Scandinavian Cardiac Out-
Society of Hypertension; European Society of Cardiology. 2007 ESH-ESC Guide-
comes Trial Investigators; CAFE Steering Committee and Writing Committee.
lines for the management of arterial hypertension: the task force for the manage-
Differential impact of blood pressure-lowering drugs on central aortic pressure
ment of arterial hypertension of the European Society of Hypertension (ESH) and
and clinical outcomes: principal results of the Conduit Artery Function Evaluation
of the European Society of Cardiology (ESC). Blood Press 2007;16:135 – 232.
(CAFE) study. Circulation 2006;113:1213 – 1225.
13. Mancia G, Laurent S, Agabiti-Rosei E, Ambrosioni E, Burnier M, Caulfied MJ,
29. Rothwell PM, Howard SC, Dolan E, O'Brien E, Dobson JE, Poulter NR, Sever PS;
Cifkova R, Clement D, Coca A, Dominiczak A, Erdine S, Fagard R, Farsang C,
on behalf of the ASCOT-BPLA and MRC Trial Investigators. Effects of b-blockers
Grassi G, Haller H, Heagerty A, Kjeldsen SE, Kiowski W, Mallion JM,
and calcium-channel blockers on within-individual variability in blood pressure
Manolis A, Narkiewicz K, Nilsson P, Olsen MH, Rahn KH, Redon J, Rodicio J,
and risk of stroke. Lancet Neurol 2010;9:469 – 480.
Ruilope L, Schmieder RE, Struijker-Boudier HA, Van Zwieten PA, Viigimaa M,
30. Weber MA, Bakris GL, Jamerson K, Weir M, Kjeldsen SE, Devereux RB,
Zanchetti A. Reappraisal of European guidelines on hypertension managements:
Velazquez EJ, Dahlof B, Kelly RY, Hua TA, Hester A, Pitt B; for the ACCOMPLISH
a European Society of Hypertension Task Force document. J Hum Hypertens
Investigators. Cardiovascular events during differing hypertension therapies in
2009;27:2121 – 2158.
patients with diabetes. JACC 2010;56:77 – 85.
14. Williams B, Poulter NR, Brown MJ, Davis M, McInnes GT, Potter JF, Sever PS,
31. Makani H, Bangalore S, Romero J, Wever-Pinzon O, Messerli FH. Effect of
Thom SM; BHS guidelines working party for the British Hypertension Society.
renin-angiotensin-system blockade on calcium channel blockers associated
Guidelines for the management of hypertension: report of the fourth working
peripheral edema. Am J Med 2011;124:128 – 135.
party of the British Hypertension Society, 2004—BHS IV. J Hum Hypertens
32. Sever PS, Poulter NR. Management of hypertension: is it the pressure or the drug?
2004;18:139 – 185.
Blood pressure reduction is not the only determinant of outcome. Circulation
15. Messerli FH, Mancia G, Conti CR, Hewkin AC, Kupfer S, Champion A, Kolloch R,
2006;113:2754 – 2774.
Benetos A, Pepine CJ. Dogma disputed: can aggressively lowering blood pressure
33. Pepine CJ, Handberg EM, Cooper-DeHoff RM, Marks RG, Kowey P, Messerli F,
in hypertensive patients with coronary artery disease be dangerous? Ann Intern
Mancia G, Cangiano JL, Garcia-Barreto D, Keltai M, Erdine S, Bristol HA,
Med 2006;144:884 – 893.
Kolb HR, Bakris GL, Cohen JD, Parmley WW; INVEST Investigators. A calcium
16. Bangalore S, Messerli FH, Wun C, Zuckerman AL, DeMicco D, Kostis JB, La
antagonist vs. a non-calcium antagonist hypertension treatment strategy for
Rosa JC. Treating to New Targets Steering Committee and Investigators.
patients with coronary artery disease. The International Verapamil-Trandolapril
J-Curve revisited: an analysis of the Treating to New Targets (TNT) Trial. Am J
Study (INVEST): a randomised controlled trial. JAMA 2003;290:2805 – 2819.
Coll Cardiol 2009;53:A219.
34. Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D,
17. SHEP Cooperative Research Group. Prevention of stroke by antihypertensive
Stoyanovsky V, Antikainen RL, Nikitin Y, Anderson C, Belhani A, Forette F,
drug treatment in older persons with isolated systolic hypertension. Final
Rajkumar C, Thijs L, Banya W, Bulpitt CJ, for the HYVET Study Group. Treatment
results of the Systolic Hypertension in the Elderly Programme (SHEP). JAMA
of hypertension in patients 80 years of age and older. NEJM 2008;358:
1991;265:3255 – 3264.
1887 – 1898.
18. Rothwell PM, Howard SC, Dolan E, O'Brien E, Dobson JE, Dahlo¨f B, Sever PS,
35. Alviar CL, Devarapally S, Romero J, Benjo AM, Nadkarni G, Javed F,
Poulter NR. Prognostic significance of visit-to-visit variability, maximum systolic
Suryadevara R, Kang H, Messerli FH. Efficacy and Safety of Dual Calcium Channel
blood pressure, and episodic hypertension. Lancet 2010;375:895 – 905.
Blocker Therapy for the Treatment of Hypertension: A Meta-analysis. ASH, 2010.
19. Webb AJ, Fischer U, Mehta Z, Rothwell PM. Effects of antihypertensive-drug class
36. Messerli FH, Staessen JA, Zannad F. Of fads, fashion, surrogate endpoints and dual
on interindividual variation in blood pressure and risk of stroke: a systematic
RAS blockade. Eur Heart J 2010; Aug 3. [Epub ahead of print].
review and meta-analysis. Lancet 2010;375:906 – 915.
P.S. Sever and F.H. Messerli
37. Yusuf S, Teo KK, Pogue J, Dyal L, Copland I, Schumacher H, Dagenais G, Sleight P,
46. Kaplan N. Clinical Hypertension. In Kaplan NM, ed. 8th ed. Lippincott Williams
Anderson C; the ON-TARGET Investigators. Telmisartan, ramipril, or both in
and Wilkins, 2002, p247.
patients at high risk for vascular events. NEJM 2008;358:1547 – 1559.
47. Hypertension Detection and Follow-up Programme Cooperative Group (HDFP).
38. Oparil S, Yarrows SA, Patel S, Zhang J, Satlin A. Dual inhibition of the renin system
Five-year findings of the Hypertension Detection and Follow-Up programme:
by aliskiren and valsartan. Lancet 2007;370:1126 – 1127.
reduction in mortality in persons with high blood pressure, including mild hyper-
39. Alvarez-Alvarez B. Management of resistant arterial hypertension: role of spiro-
tension. JAMA 1979;242:2562 – 2571.
nolactone versus double blockade of the renin-angiotensin-aldosterone system.
48. Lindholm LH, Carlberg B, Samuelssson O. Should b blockers remain first choice
J Hypertens 2010; Jul 21. [Epub ahead of print].
in the treatment of primary hypertension? A meta-analysis. Lancet 2005;366:
40. Bailey RR, Neale TJ. Rapid clonidine withdrawal with blood pressure overshoot
1545 – 1553.
exaggerated by beta-blockade. BMJ 1976;6015:942 – 943.
49. Gupta AK, Arshad S, Poulter NR. Compliance, safety and effectiveness of fixed-
41. Chapman N, Chang CL, Dahlof B, Sever PS, Wedel H, Poulter NR, for the
dose combinations of antihypertensive agents: a meta-analysis. Hypertension 2010;
ASCOT Investigators. Effect of doxazosin gastrointestinal therapeutic system as
55:399 – 407.
third-line antihypertensive therapy on blood pressure and lipids in the
50. Bangalore S, Kamalakkannan G, Parkar S, Messerli FH. Fixed-dose combinations
Anglo-Scandinavian Cardiac Outcomes Trial. Circulation 2008;118:42 – 48.
improve medication compliance: a meta-analysis. Am J Med 2007;120:713 – 719.
42. ALLHAT Officers and Coordinators for the ALLHATT Collaborative Research
51. Wolf-Maier K, Cooper RS, Kramer H, Banegas JR, Giampaoli S, Joffres MR,
Group. Diuretic versus a-blocker as first-step antihypertensive therapy. Finalresults from the Antihypertensive and Lipid-Lowering Treatment to Prevent
Poulter NR, Primatesta P, Stegmayr B, Thamm M. Hypertension treatment and
Heart Attack Trial (ALLHAT). Hypertension 2003;42:239 – 246.
control in five European countries, Canada, and the United States. Hypertension
43. Chapman N, Dobson J, Wilson S, Dahlof B, Sever PS, Wedel H, Poulter NR, on
2004;43:10 – 17.
behalf of the ASCOT Trial Investigators. Effect of spironolactone on blood
52. Redon J, Coca A, Lazaro P, Dolores Aguila M, Cabanas M, Gil N,
pressure in subjects with resistant hypertension. Hypertension 2007;49:839 – 845.
Sanchez-Zamarano MA, Arand P. Factors associated with therapeutic inertia in
44. Lv Y, Zou Z, Chen GM, Jia HX, Zhong J, Fang WW. Amlodipine and angiotensin-
hypertension: validation of a predictive model. J Hypertens 2010;28:1770 – 1777.
converting enzyme inhibitor combination versus amlodipine monotherapy in
53. Sever PS. Is systolic blood pressure all that matters? BMJ (Head to Head Debate)
hypertension: a meta-analysis of randomised control trials. Blood Press Monit
2009;339:138 – 139.
2010;15:195 – 204.
54. Falaschetti E, Chaudhury M, Mindell J, Poulter NR. Continued improvement in
45. Messerli FH, Grossman E. Pedal edema-not all dihydropyridine calcium antagon-
hypertension management in England. Results from the Health Survey for
ists are created equal. Am J Hypertens 2002;15:1019 – 1020.
England 2006. Hypertension 2009;53:480 – 486.
Source: https://tmt-topics.sproutlabs.com.au/log/track/40
431076MSJ0010.1177/1352458511431076Langdon et al.Multiple Sclerosis Journal Research Paper Multiple Sclerosis Journal0(0) 1 –8 Recommendations for a Brief © The Author(s) 2012Reprints and permissions: sagepub.co.uk/journalsPermissions.nav International Cognitive Assessment for Multiple Sclerosis (BICAMS)
Rapid oscillometric blood pressure measurement compared toconventional oscillometric measurementSteven A. Yarowsa, Ketul Patelb and Robert Brooka Background There have been few reports studying the necessary interval between blood pressure Oscillometric blood pressure measurement has largely measurements, after the initial rest period.