4ousl.dt
The new england journal
of medicine
Alastair J.J. Wood, M.D.,
Editor
Management of Overactive Bladder
Joseph G. Ouslander, M.D.
From the Division of Geriatric Medicine
veractive bladder is a symptom complex that includes uri-
and Gerontology, Wesley Woods Center,
nary urgency with or without urge incontinence, urinary frequency (voiding
Center for Health in Aging, Emory Univer-
eight or more times in a 24-hour period), and nocturia (awakening two or
sity, and the Birmingham/Atlanta VeteransAffairs Geriatric Research Education Clini-
more times at night to void).1-3 The International Continence Society classifies over-
cal Center — both in Atlanta. Address re-
active bladder as a syndrome for which no precise cause has been identified, with local
print requests to Dr. Ouslander at the Wes-
abnormalities ruled out by diagnostic evaluation.4,5 This review extends beyond the In-
ley Woods Center of Emory University, 1841Clifton Rd., NE, Atlanta, GA 30329, or at
ternational Continence Society's current definition of overactive bladder, since a broad-
er approach to this syndrome is essential for optimal management.6,7
Because overactive bladder is a recently defined syndrome, its prevalence and natural
N Engl J Med 2004;350:786-99.
Copyright 2004 Massachusetts Medical Society.
history have not been well studied. In a telephone survey of 16,776 adults who were 40years of age or older in Europe, 16 percent of men and 17 percent of women reportedsyndromes suggestive of overactive bladder. The prevalence was 3 percent among men40 to 44 years of age, 9 percent among women 40 to 44 years of age, 42 percent amongmen 75 years of age or older, and 31 percent among women 75 years of age or older.9Similar data on the prevalence of overactive bladder have been reported in the UnitedStates.10
Patients with symptoms of overactive bladder tend to curtail their participation in so-
cial activities and to isolate themselves and are predisposed to depression. Nocturia isassociated with sleep disruption, which decreases the quality of life.11-14 Postmeno-pausal women with urge incontinence have a substantially higher risk of falling andsustaining a fracture than women without urge incontinence.15 The costs of overactivebladder are probably high but have not been studied systematically. The total costs ofurinary incontinence in the United States in 1995 were estimated to be approximately$26 billion. A substantial proportion of this cost is attributable to urge incontinence,one of the cardinal symptoms of overactive bladder.16
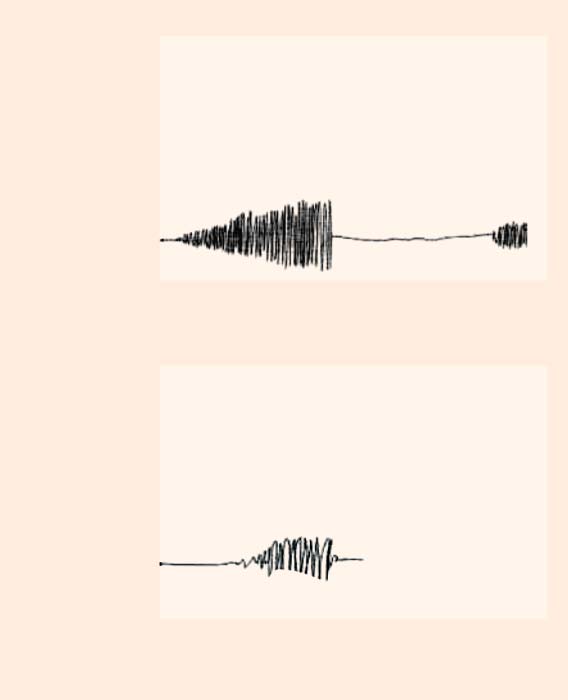
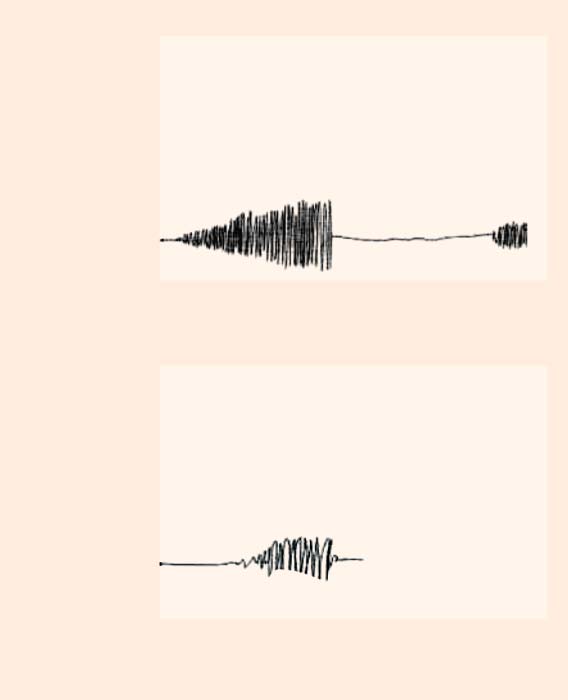
The symptoms of overactive bladder have many potential causes and contributing factors(Table 1).1-3 Urination involves the higher cortex of the brain; the pons; the spinal cord;the peripheral autonomic, somatic, and sensory afferent innervation of the lower urinarytract; and the anatomical components of the lower urinary tract itself. Disorders of anyof these structures may contribute to the symptoms of overactive bladder. The normalbladder functions like a compliant balloon as it fills, with pressure remaining lowerthan urethral resistance. With the initiation of normal urination, urethral resistance de-creases and a phasic contraction of the detrusor muscle empties the bladder (Fig. 1A).
The symptoms of overactive bladder are usually associated with involuntary contractionsof the detrusor muscle (Fig. 1B). Overactivity of the detrusor muscle, whether neuro-genic or idiopathic, can result in urgency or urge incontinence, depending on the re-
february 19, 2004
Downloaded from www.nejm.org at BERKSHIRE MED CTR on August 21, 2006 .
Copyright 2004 Massachusetts Medical Society. All rights reserved.
sponse of the sphincter.17 Detrusor overactivity may
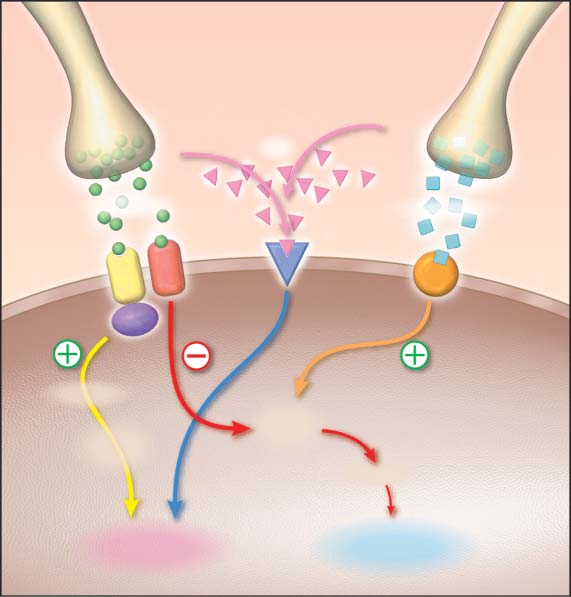
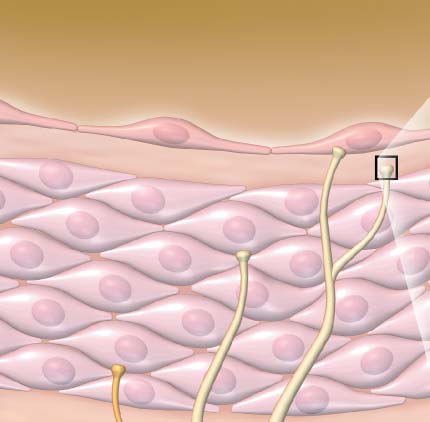
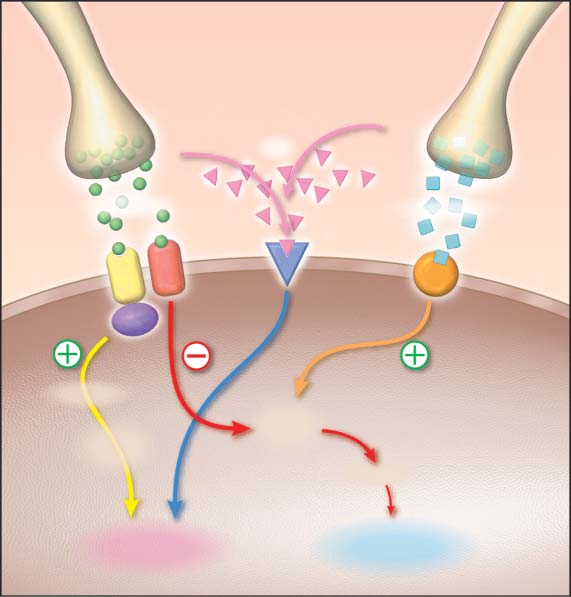
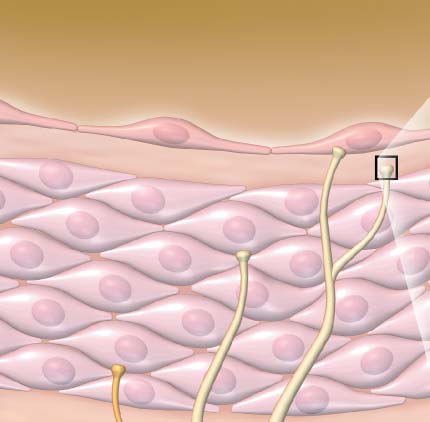
Increasing attention has been paid to the role of
also have a myogenic origin.18 Detrusor contrac- sensory afferent nerves in normal voiding and detru-tions can be weak as a result of impaired contract- sor overactivity.20-22,29 During bladder filling, affer-ibility. Urodynamic testing indicates that up to half ent activity from the bladder and urethra reaches theof elderly patients with detrusor overactivity empty spinal cord predominantly by means of the pelvicless than one third of their bladder contents with nerve. Sensory input during bladder filling resultsan involuntary bladder contraction19; incomplete in an increase in sympathetic tone, which inhibitsemptying can contribute to urinary frequency by bladder parasympathetic motor nerves, causinglowering the functional capacity of the bladder.
contraction of the bladder base and urethra. Adre-
A variety of efferent and afferent neural pathways, nergic activity may also cause relaxation of the detru-
reflexes, and central and peripheral neurotransmit- sor muscle through the stimulation of
b -adrener-
ters are involved in urine storage and bladder empty- gic receptors (Fig. 2).30 Myelinated A delta sensorying. The relation among these factors is incomplete- fibers respond to passive distention and actively understood. The role of central neurotransmitters contraction of the detrusor muscle. Unmyelinatedin the voiding cycle has been studied in animals.20-22 C sensory fibers have a higher mechanical thresholdGlutamate is an excitatory neurotransmitter in path- and respond to a variety of neurotransmitters (Fig.
ways controlling the lower urinary tract. Serotoner- 3). C fibers are relatively inactive during normal void-gic activity facilitates urine storage by enhancing the ing, but they may have a critical role in symptoms ofsympathetic reflex pathway and inhibiting the para- overactive bladder in patients with neurologic andsympathetic voiding pathway. Dopaminergic path- other disorders. Several types of receptors have beenways may exert both inhibitory and facilitatory ef- identified on afferent nerves, including vanilloid re-fects on voiding. Dopamine D1 receptors appear to ceptors, which are activated by capsaicin and possi-have a role in suppressing bladder activity, whereas bly by endogenous anandamide; purinergic recep-dopamine D2 receptors appear to facilitate voiding. tors (P2X), which are activated by ATP; neurokininOther neurotransmitters, such as
g-aminobutyric receptors, which respond to substance P and neuro-acid and enkephalin, inhibit voiding in animals.
kinin A; and receptors for nerve growth factor (trk-A
Acetylcholine, which interacts with muscarinic receptors).20,31 Other substances, including nitric
receptors on the detrusor muscle, is the predomi- oxide, calcitonin gene–related protein, and brain-nant peripheral neurotransmitter responsible for derived neurotropic factor, may also have an impor-bladder contraction. Of the five known muscarinic tant role in modulating the sensory afferents in thesubtypes (M1 through M5), M3 appears to be the human detrusor.20-22 A better understanding of themost clinically relevant in the human bladder.20 Ace- complex interplay among these various neurotrans-tylcholine interacts with the M3 receptor, initiating mitters and other substances derived from uroepi-a cascade of events that results in contraction of the thelium, detrusor-muscle cells, and afferent fibersdetrusor muscle (Fig. 2). Data from studies of rat themselves should yield new and more specific tar-bladders suggest that the M2 receptor may also fa- gets for drug treatment of overactive bladder.
cilitate bladder contraction by reducing intracellularlevels of cyclic adenosine monophosphate.23
Pathologic states can alter sensitivity to musca-
rinic stimulation. For example, bladder-outflow ob- Effective treatment of patients with symptoms ofstruction appears to enhance responsiveness to ace- overactive bladder necessitates a targeted diagnostictylcholine, a phenomenon similar to denervation evaluation. Guidelines for the management of uri-suprasensitivity.20 Normally, only a small propor- nary incontinence32 and benign prostatic hyper-tion of the bladder contraction is resistant to atro- plasia33 are relevant to the evaluation of symptomspine, probably as a result of the interactions of ATP of overactive bladder. A focused history that includeswith purinergic receptors. However, ATP may have information about past genitourinary disorders anda more prominent role in bladder contraction in pa- other conditions outlined in Table 1 should be elic-tients with overactive bladder.20-22 Anatomical cor- ited from all patients. A symptom index for benignrelates of detrusor overactivity have also been de- prostatic hypertrophy (recommended by the Amer-scribed. For example, the bladders of patients with ican Urological Association) or a similar symptomdetrusor overactivity appear to have abnormal gap index is helpful to include as part of the evaluationjunctions between smooth-muscle cells.24-28 Such in older men.34,35 A variety of questionnaires re-correlates require further study.
garding lower urinary tract symptoms have also
n engl j med 350;8
february 19, 2004
Downloaded from www.nejm.org at BERKSHIRE MED CTR on August 21, 2006 .
Copyright 2004 Massachusetts Medical Society. All rights reserved.
The new england journal
of medicine
Table 1. Conditions That Can Cause or Contribute to Symptoms of Overactive Bladder.
Mechanisms or Effect
Implications for Management
Lower urinary tract conditions
Urinary tract infection
Inflammation with activation of sensory
Treat infection before other interventions are con-
afferent innervation can result.
Obstruction can contribute to detrusor
Consider surgical intervention.
overactivity and urinary retention.
Impaired bladder contractility
Urinary retention and reduced functional
Avoid drugs that decrease bladder contractility.
bladder capacity can result.
Teach patients to enhance voiding (e.g., Credé's
Intermittent catheterization is helpful in selected
Bladder abnormalities or inflammation Intravesical abnormalities can precipitate
Sterile hematuria and risk factors for bladder
(e.g., tumors, calculi, interstitial
cancer should prompt further evaluation.
Estrogen deficiency
Inflammation from atrophic vaginitis and
Topical estrogen may ameliorate symptoms.
urethritis can contribute to symptoms.
Sphincter weakness
Leakage of urine into proximal urethra
Topical estrogen and pelvic-muscle exercises may
may precipitate urgency.
help strengthen the sphincter.
Ability to inhibit detrusor by sphincter
Periurethral injections or surgical procedures may
contraction may be diminished.
be helpful in selected patients.
Prostate enlargement
Benign or malignant prostate enlarge-
Evaluation and treatment for prostate cancer
ment can contribute to detrusor
should be considered.
Alpha-adrenergic blockers may improve symptoms.
5
a-Reductase inhibitors may reduce prostate size.
Surgical removal of obstructing prostate may be
Stroke, Alzheimer's disease, multi-
Higher cortical inhibition of the bladder
Management must include a means of compensa-
infarct dementia, other dementias,
is impaired, causing neurogenic
tion for impaired cognition, impaired mobility,
Parkinson's disease, multiple sclerosis
Multiple sclerosis, cervical or lumbar
Neurogenic detrusor overactivity or urinary Presence of neurologic symptoms or signs may
stenosis or disk herniation, spinal
retention can result.
require further evaluation.
Urodynamic testing is often indicated for diag-
nostic purposes.
Peripheral innervation
Diabetic neuropathy, nerve injury
Urinary retention and low functional blad-
History suggestive of nerve injury or neurologic
der capacity can result.
signs require further evaluation.
been developed for women.36 In addition, diaries lected patients. The presence of residual urine aftercan be helpful in determining the frequency, vol- voiding should be determined in patients with riskume, and pattern of voiding, as well as providing factors for urinary retention (diabetes, spinal cordclues to underlying causes and contributing fac- disease, and benign prostatic hypertrophy). This cantors.37,38 All patients should undergo a focused be accomplished by sterile in-and-out catheteriza-physical examination that includes genitourinary, tion. A portable ultrasonographic device is availablepelvic, and rectal examinations; a clean urine spec- that permits noninvasive identification of clinicallyimen should be obtained to rule out hematuria and significant residual urine (>100 ml), with an accu-infection.
racy rate of more than 90 percent; it costs approxi-
Further evaluation should be considered in se- mately $8,000.39 Patients with sterile hematuria or
february 19, 2004
Downloaded from www.nejm.org at BERKSHIRE MED CTR on August 21, 2006 .
Copyright 2004 Massachusetts Medical Society. All rights reserved.
Table 1. (Continued.)
Mechanisms or Effect
Implications for Management
Congestive heart failure, venous
Volume overload can contribute to urinary
Proper timing of diuretics may ameliorate symptoms.
frequency and nocturia when patient
Use of leg elevation, support hose, and salt
restriction may be helpful.
Diabetes mellitus
Poor blood glucose control can contribute
Improved blood glucose control may ameliorate
to osmotic diuresis and polyuria.
Sleep disorders (sleep apnea, periodic
Sleep disorders can contribute to nocturia.
Reports of sleep disruption or heavy snoring may
require further evaluation.
Abnormalities of arginine vasopressin
Impaired secretion or action of vasopressin Carefully selected patients may benefit from desmo-
may cause polyuria and nocturia.
pressin therapy.
Functional and behavioral conditions
Excess intake of caffeine, alcohol;
Polyuria and urinary frequency can result.
Modification of fluid intake is critical for successful
Poor bowel habits and constipation
Fecal impaction can contribute to symptoms. An appropriate bowel regimen will reduce the inci-
dence of fecal impaction.
Impaired mobility (e.g., in patients with Impaired mobility can interfere with toilet-
Treatment of underlying disorders, including physi-
degenerative joint disease, Par-
ing ability and precipitate urge incon-
cal therapy, should be optimal; the use of urinals,
kinson's disease, severe osteo-
bedside commodes, and bedpans can be helpful.
porosis, or muscle weakness)
Psychological conditions
Chronic anxiety and learned voiding dys-
The diagnosis should be considered on the basis of
function can cause symptoms of over-
a patient's history and physical examination.
active bladder.
Side effects of medication
Diuretics, especially rapid-acting agents Diuretics cause a rapid increase in bladder
Changing to a longer-acting diuretic, altering the
volume, which may precipitate urgency
timing of the dose, or discontinuing the drug,
and detrusor overactivity.
if appropriate, can ameliorate symptoms.
Anticholinergic agents, narcotics,
These agents decrease bladder contractility
Such drugs should be discontinued whenever
calcium-channel blockers
and may cause urinary retention, with a
decreased functional bladder capacity.
These agents could theoretically contribute
No clinical studies have documented such effects,
to detrusor overactivity by increasing
but they should be considered in patients in
whom symptoms develop after the initiation of one of these agents.
risk factors for bladder cancer should undergo cys- method of ruling out obstruction in older men.40toscopy, and their urine should be sent for cytologic More complex urodynamic testing may be necessaryanalysis. Cystoscopy is also indicated in patients in patients with nonspecific symptoms and may be awith a history of recurrent urinary tract infection. Al- more accurate approach to the diagnosis of obstruc-though some urologists and gynecologists suggest tion than less invasive testing. Because this test isthat all patients in whom symptoms of overactive relatively expensive and invasive, it is recommend-bladder develop should undergo cystoscopy to rule ed only to evaluate symptoms of overactive blad-out carcinoma in situ and other intravesical abnor- der in cases in which the findings will clearly influ-malities, the cost effectiveness of this approach is ence treatment, such as after the failure of initialuncertain. Because early prostate cancer can cause therapy.1-3,7symptoms of overactive bladder, the possibility ofprostate cancer should be assessed.
The role of urodynamic testing in the evaluation
of patients with symptoms of overactive bladder is Optimal therapy for overactive bladder depends oncontroversial. A noninvasive determination of the a thorough evaluation, followed by treatment of allurinary flow rate, combined with a measurement of the likely causes and contributing factors (Table 1).
residual urine after voiding, appears to be a sensitive The genesis of symptoms of overactive bladder is
n engl j med 350;8
february 19, 2004
Downloaded from www.nejm.org at BERKSHIRE MED CTR on August 21, 2006 .
Copyright 2004 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
mixed urge–stress incontinence. Educating patients
about bladder function, appropriate fluid intake
(avoidance of caffeine, maintenance of adequate hy-
dration, and the timing of fluid intake), and manag-ing constipation is important for all patients with
overactive bladder. Education may, in fact, underlie
the prominent placebo effects (approximately 30
percent improvement in symptoms) demonstratedrepeatedly in drug trials for incontinence and over-
Striated sphincter-
active bladder. Several randomized, controlled trials,largely involving middle-aged women and women
under 75 years of age who had urge or mixed urge–stress incontinence, suggest that cognitively intact,motivated patients have a positive response to pel-
vic-muscle exercises and "bladder training."41-43
Approximately 70 percent of patients have a reduc-
tion in the number of episodes of incontinence with-
Detrusor overactivity
in two to three months. The long-term effectiveness
of these interventions requires further study.
Many patients can be taught pelvic-muscle exer-
cises during a pelvic or rectal examination or can
learn them with the use of simple educational tools
Striated sphincter-
such as an audiotape or a booklet.42 A substantialproportion of older patients benefit from biofeed-back-assisted training. "Bladder training" generally
refers to a combination of patient education, sched-uled voiding and urge-suppression techniques, and
Figure 1. Normal Voiding Physiology (Panel A) and Involuntary Detrusor Con-
pelvic-muscle exercises.41 For some patients with
traction Commonly Associated with Symptoms of Overactive Bladder (Panel B).
cognitive impairment, limited mobility, or both,
Normally, as bladder volume increases, the detrusor muscle functions like a
the use of toileting-assistance protocols such as
compliant balloon and maintains a low intravesicular pressure (less than 10 cm
prompted voiding can be very helpful in the man-
of water) — substantially lower than urethral resistance pressure (Panel A). As bladder volume continues to increase, the activity of the striated muscles
agement of overactive bladder.44 All these behav-
of the urethral sphincter increases. At the time of normal voluntary voiding,
ioral interventions can also be effective adjuncts to
which generally occurs at a urinary volume of 300 to 400 ml, muscle activity in
drug therapy.
the sphincter ceases, urethral resistance decreases, and a phasic detrusor
Some patients with severe symptoms of overac-
contraction empties the bladder. In patients with symptomatic overactive
tive bladder that are refractory to proven behavioral
bladder, involuntary bladder contractions can cause urgency and may precip-itate urine loss, depending on the response of the sphincter (Panel B). Invol-
treatment may benefit from other nonpharmaco-
untary contractions may occur at any bladder volume, but they commonly oc-
logic interventions. A wide variety of highly absor-
cur at volumes of less than 200 ml. The sphincter-muscle activity depicted in
bent pads and undergarments are available that can
Panel B is a response to the involuntary contraction of the detrusor muscle
be effective and acceptable in selected patients with
(as opposed to detrusor–sphincter dyssynergy). Detrusor overactivity can be
refractory symptoms in order to maintain "social
neurogenic or idiopathic and can be accompanied by urgency or be without sensation.
continence" and good perineal hygiene.45,46 Onlylimited evidence of efficacy is available regardingmore invasive interventions. Electrical stimulationdelivered by vaginal or rectal probes can be helpful
commonly multifactorial, and multimodal therapy in teaching some patients the proper use of pelvicthat includes nonpharmacologic as well as pharma- muscles (an approach similar to biofeedback), andcologic interventions may be indicated.
lower-frequency stimulation can inhibit bladdercontraction.47 Sacral neuromodulation by means of
implantable stimulators is used in selected patients
Various clinical trials suggest that behavioral inter- with severe neurogenic detrusor overactivity.48 Mag-ventions are efficacious for managing urge and netic stimulation has also been approved for the
february 19, 2004
Downloaded from www.nejm.org at BERKSHIRE MED CTR on August 21, 2006 .
Copyright 2004 Massachusetts Medical Society. All rights reserved.
treatment of incontinence, but this requires multi-ple visits to a facility that has the stimulation equip-ment. Surgical procedures, including motor-nerve
ablation and augmentation cystoplasty, are usedonly in patients with the most severe symptoms.49,50
Many classes of drugs have been studied or pro-posed for the treatment of symptoms of overactive
bladder.1-3,20-22,51 The majority of clinical trials have
targeted the symptoms of urinary incontinence,
though more recent trials have specifically includedsubjects with overactive bladder. Several pitfalls lim-
it the quality of many studies. Expert groups have
proposed methodologic standards that should im-prove the science underlying drug therapy of over-active bladder.52-54
Table 2 lists drugs currently used to treat symp-
toms of overactive bladder and notes both evidence
of efficacy and recommendations based on the In-
ternational Consultation on Urological Diseases.7A recent review summarizes the efficacy of anticho-
Contraction of bladder
Relaxation of bladder
linergic drugs for the treatment of overactive blad-
smooth muscle
der as reported in 32 placebo-controlled trials thatincluded 6800 subjects, over 70 percent of whom
Figure 2. Current Concepts of Autonomic Efferent Innervation Contributing
to Bladder Contraction and Urine Storage.
All anticholinergic drugs can have bothersome
In the normal human bladder, acetylcholine is the predominant neurotrans-
side effects. Although dry mouth is the most com-
mitter that causes bladder contraction. Acetylcholine interacts with M3 mus-
mon, constipation, gastroesophageal reflux, blurry
carinic receptors and activates phospholipase C through coupling with G pro-teins, which generates inositol triphosphate, which in turn causes the release
vision, urinary retention, and cognitive side effects
of calcium from the sarcoplasmic reticulum and the contraction of bladder
can also occur. Both overactive bladder and demen-
smooth muscle. M2 receptors may contribute to bladder contraction by inhib-
tia are common in older patients. Since various
iting adenylate cyclase activity and decreasing intracellular cyclic adenosine
forms of dementia are routinely treated with cholin-
monophosphate (AMP) levels, which mediate bladder relaxation. In the nor-
esterase inhibitors, the potential for adverse cog-
mal human bladder, only a small proportion of muscle contraction is resistant to atropine. Resistance to atropine most likely results from the interaction of
nitive effects and delirium due to antimuscarinic
ATP with purinergic receptors, including P2X receptors. ATP and other non-
drugs is a particular concern in this population.58,59
cholinergically mediated processes may have a more important role in disor-
Although these drugs have not had major effects
ders that cause overactive bladder. Stimulation of b -adrenergic receptors
on cognition in clinical trials involving relatively
may also lead to relaxation of bladder smooth muscle. Plus signs indicate ac-
healthy older adults, more subtle but functionally
tivation, and minus signs inhibition. Data are from Morrison et al., Yoshimura and Chancellor,21 and Andersson and Hedlund.22
important changes could occur. Quantitative elec-troencephalographic data suggest that oxybutyninhas more central nervous system effects than tros-pium or tolterodine.60 Long-acting anticholinergic der muscles and has local anesthetic activity. It isagents and newer, more selective antimuscarinic available in immediate and extended-release forms,agents should be tested for clinically important cog- as well as in a transdermal patch. Immediate-releasenitive side effects, especially in older patients.
oxybutynin (usual adult dosage, 5 mg thrice daily)
Among the anticholinergic agents, only oxybuty- appears to be efficacious for the treatment of neu-
nin, propiverine, tolterodine, and trospium (Table 2) rogenic and non-neurogenic overactivity of the de-have the highest level of clinical recommendation trusor muscle with urge incontinence. Given in thisand evidence of efficacy; oxybutynin and tolterodine formulation, oxybutynin has led to a clinically sig-have been studied most extensively. Oxybutynin is a nificant improvement, defined as a reduction innonselective antimuscarinic agent that relaxes blad- incontinence episodes by more than 50 percent,
n engl j med 350;8
february 19, 2004
Downloaded from www.nejm.org at BERKSHIRE MED CTR on August 21, 2006 .
Copyright 2004 Massachusetts Medical Society. All rights reserved.




The new england journal of medicine
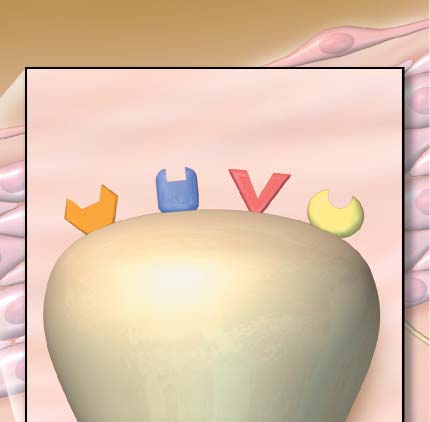
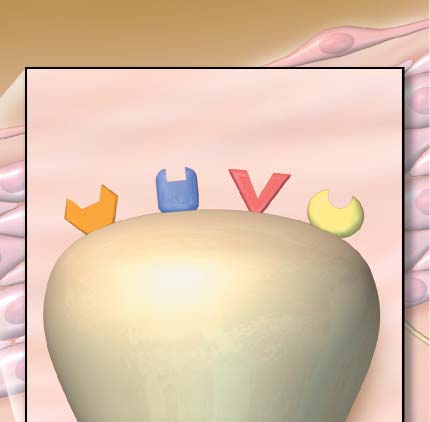
Uroepithelial cell
Vanilloid P2X2 or P2X3
C sensory fiber
Figure 3. Current Concepts of Sensory Innervation of the Bladder.
Myelinated A delta sensory fibers respond predominantly to mechanical stretching of detrusor muscle cells during blad-der filling. Unmyelinated C sensory fibers may help trigger the symptoms of overactive bladder in pathologic conditions. C fibers have receptors for a variety of neurotransmitters and substances that can be released from afferent nerves, de-trusor smooth muscle, and the uroepithelium. These receptors include vanilloid receptors, which can be stimulated by capsaicin and, possibly, endogenous anandamide; purinergic receptors (P2X and P2X ), which are activated by ATP;
neurokinin receptors, which are activated by neurokinin A and substance P; and trk-A receptors for nerve growth factor. The nerve growth factor produced by muscle cells, as well as nitrous oxide produced by the uroepithelium, may play key roles in modulating the responsiveness of afferent innervation in the bladder. Data are from Morrison et al.,20 Yoshimura and Chancellor,21 and Andersson and Hedlund.22
in approximately 60 to 80 percent of study sub- in episodes of urge incontinence by approximatelyjects.21,32,51,61 The efficacy of immediate-release 70 percent.43,63-66 A transdermal oxybutynin patchoxybutynin has been limited by antimuscarinic side is also available that is as efficacious as immediate-effects of the parent drug and its active metabolite release oxybutynin but with half the incidence of(N-desethyloxybutynin); dry mouth, for example, is dry mouth.67,68 In one placebo-controlled trial, thereported in up to two thirds of subjects in some clin- patch caused local skin erythema in more than halfical trials. Generic immediate-release oxybutynin is the subjects (3 percent of cases were severe) andrelatively inexpensive and may be useful for patients was associated with pruritus in up to 17 percent.68whose symptoms are best managed by a short-act-
Tolterodine is a muscarinic antagonist that is
ing drug (e.g., symptoms that are bothersome only available in short-acting (twice-daily) and long-act-when the patient is away from home or at night).
ing (once-daily) preparations. Both forms have had
A once-daily controlled-release formulation of statistically and clinically significant effects on
oxybutynin appears to have the same beneficial ef- symptoms of overactive bladder in multiple, ran-fects as immediate-release oxybutynin, with fewer domized, controlled clinical trials.69-77 Side effectsside effects — a benefit ascribed to the more con- are similar to those of short-acting oxybutynin, withstant levels of the parent drug and, possibly, a lower dry mouth in 20 to 25 percent of patients, and therate of conversion to the active metabolite in the rates of discontinuation due to side effects are sim-stomach and small intestine.62 Most studies of con- ilar to those for placebo (5 to 6 percent). Tolterodinetrolled-release oxybutynin have reported a reduction appears to be equally efficacious in old and young
february 19, 2004
Downloaded from www.nejm.org at BERKSHIRE MED CTR on August 21, 2006 .
Copyright 2004 Massachusetts Medical Society. All rights reserved.
Table 2. Drugs Used to Treat Symptoms of Overactive Bladder.*
Evidence/Grade of
Usual Adult Dose
Drugs with predominantly
anticholinergic or anti-
muscarinic effects
0.375 mg twice daily orally
The drug is also available in sublingual and
elixir forms; it has prominent anticho-linergic side effects.
2.5–5.0 mg thrice daily orally (short-acting)
Long-acting and transdermal preparations
5–30 mg daily orally (long-acting)
have fewer side effects than short-acting
3.9 mg over a 96-hr period (transdermal)
The transdermal patch can cause local skin
irritation in some patients.
15–30 mg 4 times daily orally
The drug has prominent anticholinergic side
15 mg thrice daily orally
The drug has complex pharmacokinetics with
several active metabolites; it is not current-ly available in the United States.
1–2 mg twice daily orally (short-acting)
The long-acting and short-acting preparations
4 mg daily orally (long-acting)
have similar efficacy.
20 mg twice daily orally
The agent is a quaternary ammonium com-
pound, which does not cross the blood–brain barrier and may have fewer cognitive side effects than other anticholinergic agents; it is not currently available in the United States.
Estrogen (for women)
Approximately 0.5 g cream applied topically
Local vaginal preparations are probably more
nightly for 2 wk, then twice per week
effective than oral estrogen, but definitive
Estradiol ring, replaced every 90 days
data on effectiveness are lacking.
Estradiol, 1 tablet daily for 2 wk, then 1 tablet
Alpha-adrenergic antagonists
(for men)
2.5 mg thrice daily orally
These agents are useful in men with benign
1–16 mg daily orally
1–10 mg twice daily orally
Postural hypotension can be a serious side
0.4–0.8 mg daily orally
1–10 mg orally each day at bedtime
Doses must be increased gradually to facilitate
Other drugs
10–25 mg thrice daily orally
This agent may be useful for mixed urge–
stress incontinence; it can cause postural hypotension and bundle-branch block.
20–40 µg of intranasal spray daily at bed-
The intranasal spray is used for primary noc-
turnal enuresis in children; hyponatremia
0.1–0.4 mg orally 2 hr before bedtime
occurs commonly in older adults, and se-rum sodium levels must be monitored closely.
* Not all drugs listed in this table have proven efficacy specifically for symptoms of overactive bladder.
† Levels of evidence are based on the Oxford System: a score of 1 indicates evidence from randomized, controlled trials; a score of 2 evidence
from good-quality prospective cohort studies; a score of 3 evidence from good-quality retrospective case–control studies; and a score of 4 ev-idence from good-quality case series.55,56 The grade of recommendations is based on the definitions used by the International Consultation on Urological Diseases7: A indicates consistent level 1 evidence; B consistent level 2 or 3 evidence or major evidence from randomized, con-trolled trials; C level 4 evidence or major evidence from level 2 or 3 studies or expert opinion based on the Delphi method; and D inconclusive, inconsistent, or nonexistent evidence or evidence based on expert opinion only.
‡ The rating is for symptoms of overactive bladder, not for overall symptoms of benign prostatic hyperplasia.
n engl j med 350;8
february 19, 2004
Downloaded from www.nejm.org at BERKSHIRE MED CTR on August 21, 2006 .
Copyright 2004 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
subjects and was well tolerated in one trial involving the efficacy of these drugs for overactive bladder, be-patients who were living in nursing homes.75,76,78 cause the outcomes of most clinical trials have beenTwo published studies, both industry-sponsored, based on composite scores that include symptomshave compared the long-acting forms of oxybutynin of both overactive bladder and obstruction.96-102and tolterodine. In one study, participating medi- Symptoms of overactive bladder tend to decreasecal practices were randomized,77 and in the other, with alpha-blocker therapy, but less so than dowomen (mean age, 60 years) were randomly as- symptoms of obstruction.102,103 Because alpha-signed to receive one or the other of these agents.79 blockers can cause postural hypotension, they re-The results of both trials suggest that the drugs quire a gradual titration of the dose and must behave similar efficacy and effectiveness. In addition, used carefully, especially in patients who are alreadyboth oxybutynin and tolterodine appear to be effec- taking antihypertensive agents.93,100-102tive when combined with various types of behavior-
Men who neither tolerate nor have a response to
alpha-blockers and who are not candidates for sur-
Randomized, controlled trials indicate that gical intervention may benefit from a trial of an anti-
propiverine and trospium are effective for the treat- cholinergic agent, provided they are carefully mon-ment of urge incontinence and have fewer side ef- itored for the development of urinary retention.
fects than short-acting oxybutynin.83-86 Neither Further research is needed to determine the optimaldrug is currently available in the United States (tros- use of alpha-blockers and anticholinergic drugs —pium is being evaluated in clinical trials in the Unit- alone, together, or combined with behavioral ther-ed States). Though hyoscyamine, like short-acting apy — as a treatment for overactive bladder in men.
oxybutynin, may be useful for some patients with in-
Treatment of nocturia, the most bothersome
termittent symptoms or under specific circumstanc- symptom of overactive bladder for many patientses, it can be associated with prominent side effects. of both sexes, depends on the primary underlyingPropantheline has proven efficacy for the treatment cause or causes — detrusor overactivity, nocturnalof urge incontinence,32,87,88 but the need for mul- polyuria, a primary sleep disorder, or some combi-tiple daily doses and the relatively high incidence of nation of these conditions.104,105 Nocturia that isside effects are drawbacks. Imipramine, a tricyclic primarily related to detrusor overactivity can be treat-antidepressant with both anticholinergic and alpha- ed with an anticholinergic agent. Nocturnal polyu-adrenergic effects and, possibly, a central effect on ria related to volume overload (e.g., venous insuffi-voiding reflexes, has been recommended for mixed ciency or congestive heart failure with peripheralurge–stress incontinence, which is common among edema) may respond to a small dose of a rapid-act-older women with overactive bladder. Imipramine ing diuretic taken in the late afternoon. Oral and in-can cause postural hypotension and cardiac-conduc- tranasal preparations of desmopressin are approvedtion abnormalities and thus must be used carefully. for use in children with nocturnal enuresis.
Postmenopausal women with symptoms of over-
Data supporting an association among noctur-
active bladder are commonly treated with oral or nal polyuria, nocturia, abnormal diurnal respon-topical estrogen, but few data document the effica- siveness to vasopressin, and levels of endogenouscy of these agents.89-92 Among men, symptoms of arginine vasopressin in adults are limited and con-overactive bladder overlap with those of benign flicting.106-109 However, two randomized, con-prostatic hypertrophy.93-95 In clinical practice, the trolled trials suggest that orally administered des-approach to men with symptoms of overactive blad- mopressin can reduce nocturia in both womender depends on several factors, such as the degree (mean age, approximately 57 years)110 and mento which specific symptoms bother the patient, the (mean age, approximately 65 years).111 Both trialspatient's preferences, evaluation of the risk–benefit used a three-week run-in dose-titration design (0.1ratio, and the physician's bias. Treatment decisions to 0.4 mg), during which approximately one thirdare further complicated by the fact that complex of the patients were excluded. Among patients withurodynamic studies are required to rule out blad- some responsiveness and ability to tolerate desmo-der-outlet obstruction as a cause. Men with isolated pressin during the dose-titration phase, one thirdsymptoms of overactive bladder — in whom pros- of the women and the men had at least a 50 percenttate cancer and obstruction have been ruled out — reduction in the number of nighttime voiding epi-are often treated initially with alpha-adrenergic sodes (as compared with 3 percent of patients inblockers (alpha-blockers). It is difficult to determine the placebo group) and a significant increase in the
february 19, 2004
Downloaded from www.nejm.org at BERKSHIRE MED CTR on August 21, 2006 .
Copyright 2004 Massachusetts Medical Society. All rights reserved.
duration of sleep before their first nighttime voiding nist, has been used in patients with the detrusor hy-during the three-week double-blind phase. Side ef- perreflexia associated with spinal cord disorders.
fects were mild; hyponatremia occurred in approx- Direct injection of botulinum toxin into the detru-imately 5 percent of patients but only during the sor muscle, which inhibits acetylcholine at the pre-three-week dose-titration phase. On the basis of synaptic cholinergic junction, appears to amelioratethese data, oral desmopressin has been approved detrusor hyperreflexia in patients with spinal cordfor the treatment of nocturia in several countries in injury112,113; it may have some therapeutic value inEurope, but it is not yet approved for this indication selected patients with severe refractory symptomsin the United States.
of overactive bladder. Although currently available
Because of their mechanisms of action, several beta-agonists have not been shown to be useful for
classes of drugs used for other conditions are of overactive bladder, more selective b -agonists may
potential therapeutic value for patients with over- have therapeutic value.
active bladder, but data from randomized, con-
There are several promising directions for the
trolled clinical trials are lacking. Such drug classes development of drugs to treat overactive bladder (Ta-include calcium-channel blockers, prostaglandin- ble 3). At least two antimuscarinic drugs (darifena-synthesis inhibitors, dopamine D1–receptor ago- cin and solifenacin) with selective M3-receptor–nists, beta-adrenergic (particularly b ) agonists, and antagonist actions and, theoretically, fewer systemic
g-aminobutyric acid (GABA) agonists (Table 3).20-22 anticholinergic side effects than currently availableFor example, pergolide, a D1-receptor agonist, may agents are being studied. Oxybutynin has been in-benefit patients with Parkinson's disease and lower stilled intravesicularly through a catheter to treat se-urinary tract symptoms, and baclofen, a GABA ago- vere overactivity of the detrusor muscle,114 and a
Table 3. Examples of Classes of Drugs under Investigation for the Treatment of Symptoms of Overactive Bladder.*
Drug Classes and Actions
in Humans
Drugs used for other conditions
Calcium-channel blockers
Agents inhibit bladder contraction by decreasing calcium available for
smooth-muscle contraction; there is no evidence that these agents
are effective for symptoms of overactive bladder.
Inhibitors of prostaglandin synthesis
Prostaglandins may increase the contraction of bladder smooth muscle;
no currently available agents have proven efficacy.
g-Aminobutyric acid–receptor agonists
Stimulation of g-aminobutyric acid receptors inhibits the voiding reflex.
Neuromuscular-junction inhibition
Botulinum toxin A injections have been used for refractory symptoms.
of acetylcholine release
Drugs in development
Antimuscarinic agents more selective
for M3 receptors than other anti-
muscarinic agents
These agents decrease spontaneous detrusor-muscle contractions and can
have clinically significant effects on blood pressure; potassium-channel gene therapy has also been studied.
Serotonergic agonists
The central serotonergic effects of these agents increase urethral striated
Vanilloids and other afferent-nerve
These agents cause desensitization of unmyelinated C fibers; other
afferent-nerve inhibitors may be useful.
D1-receptor stimulation inhibits the voiding reflex.
Nerve growth factor inhibitors
Nerve growth factor modulates sensory afferent function; antibody-based
gene therapy to suppress nerve growth factor has also been studied.
Opioid peptides, including enkephalin, suppress the voiding reflex; therapy
with the herpes simplex virus proenkephalin gene has been studied.
* Drugs listed in this table do not have proven efficacy in the treatment of overactive bladder and should not be prescribed until data from clin-
ical trials are published.
n engl j med 350;8
february 19, 2004
Downloaded from www.nejm.org at BERKSHIRE MED CTR on August 21, 2006 .
Copyright 2004 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
bladder pump is being developed that can deliver a verse consequences such as injurious falls. Theconstant dose of intravesicular oxybutynin for up symptoms may be caused by myriad factors, includ-to 30 days.21 Such a device may make this method ing disorders of the lower urinary tract, neurologicof drug delivery more practical and acceptable and conditions, behavioral factors such as caffeine in-may result in fewer systemic anticholinergic side take, and a variety of commonly prescribed drugs.
effects.
The pathophysiologic process in an individual pa-
Drugs that act by means of potassium-channel tient is often multifactorial. Diagnostic evaluation
transporters to hyperpolarize smooth muscle and includes a focused history taking, targeted physi-decrease spontaneous bladder contractions may be cal examination, and urinalysis. Selected patientsuseful for suppressing involuntary bladder contrac- should have a post-void residual determination, andtions without interfering with normal voiding.115 some should undergo cystoscopy (such as thoseHowever, first-generation agents in this class have with hematuria) or complex urodynamic testinghad effects on vascular smooth muscle and can (such as those with urinary retention or neurologiccause hypotension. Duloxetine is an inhibitor of se- disorders).
rotonin and norepinephrine that appears to act cen-
Patients with overactive bladder often benefit
trally, increasing tone in the striated smooth muscle from supportive measures such as education,of the external urethral sphincter.116 Although it is changes in fluid intake, and the use of bedside com-being studied primarily for the treatment of stress modes or urinals, especially at night. Behavioralincontinence, duloxetine may also have therapeutic treatments such as pelvic-muscle exercises andbenefits in patients with mixed stress–urge inconti- bladder training are efficacious and can enhance thenence. Drugs that act on sensory afferent pathways benefits of drug therapy. The mainstay of drug ther-are also being developed and hold promise when apy is antimuscarinic agents. The two best-studiedused either alone or in combination with other agents are oxybutynin and tolterodine; both havedrugs. Capsaicin and resiniferatoxin desensitize well-proven efficacy in short- and long-actingC-fiber afferents and have been administered ex- forms. The extended-release formulations and theperimentally by the intravesicular route. Resinifer- oxybutynin skin patch are generally well tolerated,atoxin appears to be more potent and less irritating but all antimuscarinic drugs can have bothersomethan capsaicin and may be more useful clinical- anticholinergic side effects. The effects of thesely.55,117,118 Other drugs that block receptors on sen- agents on cognitive function are a particular concernsory afferents, such as neurokinin-receptor antago- in older adults. Men with symptoms of overactivenists (Fig. 3), might not cause urinary retention, bladder in association with benign prostatic hyper-which can occur with antimuscarinic agents.
plasia may benefit from treatment with alpha-block-ers. Promising future directions in drug therapyinclude the development of more specific anti-
muscarinic agents, new drug-delivery systems, and
Symptoms of overactive bladder are common, can drugs that affect the sensory innervation of the low-be distressing, and are associated with serious ad- er urinary tract.
r e f e r e n c e s
Abrams P, Wein AJ, eds. The Overactive
D, et al. The standardisation of terminology
the symptoms of an overactive bladder and
Bladder: From Basic Science to Clinical Man-
in nocturia: report from the Standardisation
how are they managed? A population-based
agement Consensus Conference. Urology
Sub-committee of the International Conti-
prevalence study. BJU Int 2001;87:760-6.
nence Society. Neurourol Urodyn 2002;21:
[Erratum, BJU Int 2001;88:807.]
Idem. Overactive Bladder and Its Treat-
10. Stewart W, Herzog R, Wein A, et al. Prev-
ments Consensus Conference. Urology
Blaivas JG. Overactive bladder revisited.
alence and impact of overactive bladder in
Neurourol Urodyn 2002;21:523.
the US: results for the NOBLE program. Neu-
Staskin DR, Wein AJ, eds. New perspec-
Abrams P, Cardozo L, Khoury S, Wein A,
rourol Urodyn 2001;20:406. abstract.
tives on the overactive bladder. Urology 2002;
eds. Incontinence. 2nd ed. Plymouth, En-
11. Kobelt G. Economic considerations and
gland: Health Publications, 2002.
outcome measurement in urge incontinence.
Abrams P, Cardozo L, Fall M, et al. The
Garnett S, Abrams P. The natural history
standardisation of terminology of lower uri-
of the overactive bladder and detrusor over-
12. Brown JS, Posner SF, Stewart AL. Urge
nary tract function: report from the Standard-
activity: a review of the evidence regarding
incontinence: new health-related quality of
isation Sub-committee of the International
the long-term outcome of the overactive
life measures. J Am Geriatr Soc 1999;47:
Continence Society. Neurourol Urodyn 2002;
bladder. J Urol 2003;169:843-8.
Milson I, Abrams P, Cardozo L, Roberts
13. DuBeau CE, Kiely DK, Resnick NM.
van Kerrebroeck P, Abrams P, Chaikin
RG, Thuroff J, Wein AJ. How widespread are
Quality of life impact of urge incontinence
february 19, 2004
Downloaded from www.nejm.org at BERKSHIRE MED CTR on August 21, 2006 .
Copyright 2004 Massachusetts Medical Society. All rights reserved.
in older persons: a new measure and con-
29. Jung SY, Fraser MO, Ozawa H, et al. Ure-
domized controlled trial. JAMA 1998;280:
ceptual structure. J Am Geriatr Soc 1999;47:
thral afferent nerve activity affects the mictu-
rition reflex: implication for the relationship
44. Ouslander JG, Schnelle JF, Uman G, et
14. Dugan E, Cohen SJ, Bland DR, et al. The
between stress incontinence and detrusor
al. Predictors of successful prompted void-
association of depressive symptoms and
instability. J Urol 1999;162:204-12.
ing among incontinent nursing home resi-
urinary incontinence among older adults.
30. Igawa Y, Yamazaki Y, Takeda H, et al.
dents. JAMA 1995;273:1366-70.
J Am Geriatr Soc 2000;48:413-6.
Functional and molecular biological evi-
45. Johnson TM II, Kincade JE, Bernard SL,
15. Brown JS, Vittinghoff E, Wyman JF, et al.
dence for a possible beta3-adrenoceptor in
Busby-Whitehead J, DeFriese GH. Self-care
Urinary incontinence: does it increase risk
the human detrusor muscle. Br J Pharmacol
practices used by older men and women to
for falls and fractures? Study of Osteoporot-
manage urinary incontinence: results from
ic Fractures Research Group. J Am Geriatr
31. O'Reilly BA, Kosaka AH, Knight GF, et
the National Follow-up Survey on Self-Care
Soc 2000;48:721-5.
al. P2X receptors and their role in female id-
and Aging. J Am Geriatr Soc 2000;48:894-
16. Hu T-W. Moore K, Subak L, et al. Eco-
iopathic detrusor instability. J Urol 2002;
nomics of incontinence. In: Abrams P, Car-
46. Johnson TM, Ouslander JG, Uman GC,
dozo L, Khoury S, Wein A, eds. Incontinence.
32. Fantl JA, Newman DK, Colling J, et al.
Schnelle JF. Urinary incontinence treatment
2nd ed. Plymouth, England: Health Publica-
Urinary incontinence in adults: acute and
preferences in long-term care. J Am Geriatr
tions, 2002:3-20.
chronic management. Clinical practice
Soc 2001;49:710-8.
17. Fisser AJ, Walmsley K, Blaivas JG. Uro-
guideline. No. 2. 1996 update. Rockville,
47. Brubaker L. Electrical stimulation in
dynamic classification of patients with symp-
Md.: Agency for Health Care Policy and Re-
overactive bladder. Urology 2000;55:Suppl:
toms of overactive bladder. J Urol 2003;169:
search, March 1996. (AHCPR publication
17-23, 31-2.
48. Hohenfellner M, Dahms SE, Matzel K,
18. Brading AF. A myogenic basis for the
33. McConnell JD, Barry MJ, Bruskewitz
Thuroff JW. Sacral neuromodulation for
overactive bladder. Urology 1997;50:Suppl:
RC, et al. Benign prostatic hyperplasia: diag-
treatment of lower urinary tract dysfunction.
nosis and treatment. Clinical practice guide.
BJU Int 2000;85:Suppl 3:10-9, 22-3.
19. Resnick NM, Yalla SV. Detrusor hyper-
No. 8. Rockville, Md.: Agency for Health
49. Madersbacher H. Denervation tech-
activity with impaired contractile function:
Care Policy and Research, February 1994.
niques. BJU Int 2000;85:Suppl 3:1-6, 8-9.
an unrecognized but common cause of in-
(AHCPR publication no. 94-0582.)
50. Atala A. New methods of bladder aug-
continence in elderly patients. JAMA 1987;
34. Barry MJ, Fowler FJ Jr, O'Leary MP, et al.
mentation. BJU Int 2000;85:Suppl 3:24-34,
The American Urological Association symp-
20. Morrison J, Steers WD, Brading AF, et al.
tom index for benign prostatic hyperplasia.
51. Anderson K-E, Appell R, Awad S, et al.
Neurophysiology and neuropharmacology.
J Urol 1992;148:1549-57, 1564.
Pharmacologic treatment of urinary inconti-
In: Abrams P, Cardoza L, Khoury S, Wein A,
35. Peters TJ, Donovan JL, Kay HE, et al. The
nence. In: Abrams P, Cardozo L, Khoury S,
eds. Incontinence. 2nd ed. Plymouth, En-
International Continence Society "Benign
Wein A, eds. Incontinence. 2nd ed. Ply-
gland: Health Publications, 2002:86-163.
Prostatic Hyperplasia" Study: the bother-
mouth, England: Health Publications, 2002:
21. Yoshimura N, Chancellor MB. Current
someness of urinary symptoms. J Urol 1997;
and future pharmacological treatment for
52. Blaivas JG, Appell RA, Fantl JA, et al.
overactive bladder. J Urol 2002;168:1897-
36. Graham CW, Dmochowki RR. Ques-
Standards of efficacy for evaluation of
tionnaires for women with urinary symp-
treatment outcomes in urinary inconti-
22. Andersson KE, Hedlund P. Pharmaco-
toms. Neurourol Urodyn 2002;21:473-81.
nence: recommendations of the Urody-
logic perspective on the physiology of the
37. Wyman JF, Choi SC, Harkins SW, Wil-
namic Society. Neurourol Urodyn 1997;16:
lower urinary tract. Urology 2002;605:Suppl
son MS, Fantl JA. The urinary diary in evalu-
ation of incontinent women: a test-retest
53. Fonda D, Resnick NM, Colling J, et al.
23. Hedge S, Choppin A, Bonhaus D, et al.
analysis. Obstet Gynecol 1988;71:812-7.
Outcome measures for research of lower
Functional role of M2 and M3 muscarinic
38. Locher JL, Goode PS, Roth DL, Worrell
urinary tract dysfunction in frail older peo-
receptors in the urinary bladder of rats in vi-
RL, Burgio KL. Reliability assessment of the
ple. Neurourol Urodyn 1998;17:273-81.
tro and in vivo. Br J Pharmacol 1997;120:
bladder diary for urinary incontinence in
54. Payne C, van Kerrebroeck P, Blaivas JG,
older women. J Gerontol A Biol Sci Med Sci
et al. Research methodology in urinary in-
24. Elbadawi A, Hailemariam S, Yalla SV,
continence. In: Abrams P, Cardozo L,
Resnick NM. Structural basis of geriatric
39. Marks LS, Dorey FJ, Macairan ML, Park
Khoury S, Wein A, eds. Incontinence. 2nd
voiding dysfunction. VI. Validation and up-
C, deKernion JB. Three-dimensional ultra-
ed. Plymouth, England: Health Publica-
date of diagnostic criteria in 71 detrusor bi-
sound device for rapid determination of
opsies. J Urol 1997;157:1802-13.
bladder volume. Urology 1997;50:341-8.
55. De Ridder D, Chandiramani V, Dasgup-
25. Idem. Structural basis of geriatric void-
40. DuBeau CE, Yalla SV, Resnick NM. Im-
ta P, Van Poppel H, Baert L, Fowler C. Intra-
ing dysfunction. VII. Prospective ultrastruc-
proving the utility of urine flow rate to ex-
vesical capsaicin as a treatment for refracto-
tural/urodynamic evaluation of its natural
clude outlet obstruction in men with voiding
ry detrusor hyperreflexia: a dual center study
evolution. J Urol 1997;157:1814-22.
symptoms. J Am Geriatr Soc 1998;46:1118-
with long-term followup. J Urol 1997;158:
26. Elbadawi A, Yalla SV, Resnick NM.
Structural basis of geriatric voiding dysfunc-
41. Fantl JA, Wyman JF, McClish DK, et al.
56. Levels of evidence and grades of recom-
tion. I. Methods of a prospective ultrastruc-
Efficacy of bladder training in older women
mendation. Oxford, England: Centre for Ev-
tural/urodynamic study and an overview of
with urinary incontinence. JAMA 1991;265:
idence-Based Medicine. (Accessed January
the findings. J Urol 1993;150:1650-6.
27, 2004, at http://www.cebm.net/levels_ of_
27. Idem. Structural basis of geriatric void-
42. Burgio KL, Goode PS, Locher JL, et al.
ing dysfunction. II. Aging detrusor: normal
Behavioral training with and without bio-
57. Herbison P, Hay-Smith J, Ellis G, Moore
versus impaired contractility. J Urol 1993;
feedback in the treatment of urge inconti-
K. Effectiveness of anticholinergic drugs
nence in older women: a randomized con-
compared with placebo in the treatment of
28. Tse V, Wills E, Szonyi G, Khadra MH.
trolled trial. JAMA 2002;288:2293-9.
overactive bladder: systematic review. BMJ
The application of ultrastructural studies in
43. Burgio KL, Locher JL, Goode PS, et al.
the diagnosis of bladder dysfunction in a
Behavioral vs drug treatment for urge uri-
58. Edwards KR, O'Connor JT. Risk of delir-
clinical setting. J Urol 2000;163:535-9.
nary incontinence in older women: a ran-
ium with concomitant use of tolterodine
n engl j med 350;8
february 19, 2004
Downloaded from www.nejm.org at BERKSHIRE MED CTR on August 21, 2006 .
Copyright 2004 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
and acetylcholinesterase inhibitors. J Am
71. Drutz HP, Appell RA, Gleason D, Klim-
continence: a multicentre dose-optimizing
Geriatr Soc 2002;50:1165-6.
berg I, Radomski S. Clinical efficacy and
study. Scand J Urol Nephrol 1995;29:289-94.
59. Katz IR, Sands LP, Bilker W, DiFillipo S,
safety of tolterodine compared to oxybuty-
84. Madersbacher H, Halaska M, Voigt R,
Boyce A, D'Angelo K. Identification of med-
nin and placebo in patients with overactive
Alloussi S, Hofner K. A placebo-controlled,
ications that cause cognitive impairment in
bladder. Int Urogynecol J Pelvic Floor Dys-
multicentre study comparing the tolerability
older people: the case of oxybutynin chlo-
and efficacy of propiverine and oxybutynin
ride. J Am Geriatr Soc 1998;46:8-13.
72. Freedman S, Mitcheson HD, Antoci J,
in patients with urgency and urge inconti-
60. Todorova A, Vonderheid-Guth B, Dimp-
Primus G, Chancellor MF, Wein A. Toltero-
nence. BJU Int 1999;84:646-51.
fel W. Effects of tolterodine, trospium chlo-
dine, an effective and well tolerated treat-
85. Madersbacher H, Murtz G. Efficacy, tol-
ride, and oxybutynin on the central nervous
ment for urge incontinence and other over-
erability and safety profile in propiverine in
system. J Clin Pharmacol 2001;41:636-44.
active bladder symptoms. Clin Drug Invest
the treatment of the overactive bladder (non-
61. Yarker YE, Goa KL, Fitton A. Oxybuty-
neurogenic and neurogenic). World J Urol
nin: a review of its pharmacodynamic and
73. Van Kerrebroeck P, Kreder K, Jonas U,
pharmacokinetic properties, and its thera-
Zinner N, Wein A. Tolterodine once-daily:
86. Madersbacher H, Stohrer M, Richter R,
peutic use in detrusor instability. Drugs Ag-
superior efficacy and tolerability in the treat-
Burgdorfer H, Hachen HJ, Murtz G. Trospi-
ing 1995;6:243-62.
ment of the overactive bladder. Urology
um chloride versus oxybutynin: a random-
62. Gupta SK, Sathyan G. Pharmacokinet-
ized, double-blind, multicentre trial in the
ics of an oral once-a-day controlled-release
74. Malone-Lee J, Shaffu B, Anand C, Pow-
treatment of detrusor hyper-reflexia. Br
oxybutynin formulation compared with im-
ell C. Tolterodine: superior tolerability than
J Urol 1995;75:452-6.
mediate-release oxybutynin. J Clin Pharma-
and comparable efficacy to oxybutynin in in-
87. Holmes DM, Montz FJ, Stanton SL.
col 1999;39:289-96.
dividuals 50 years old or older with overac-
Oxybutynin versus propantheline in the man-
63. Anderson RU, Mobley D, Blank B,
tive bladder: a randomized controlled trial.
agement of detrusor instability: a patient-
Saltzstein D, Susset J, Brown JS. Once daily
J Urol 2001;165:1452-6.
regulated variable dose trial. Br J Obstet Gy-
controlled versus immediate release oxybu-
75. Malone-Lee JG, Walsh JB, Maugourd
tynin chloride for urge urinary inconti-
MF. Tolterodine: a safe and effective treat-
88. Thuroff J, Bunke B, Ebner A, et al. Ran-
nence. J Urol 1999;161:1809-12.
ment for older patients with overactive blad-
domized, double-blind, multicenter trial on
64. Gleason DM, Susset J, White C, Munoz
der. J Am Geriatr Soc 2001;49:700-5.
treatment of frequency, urgency and incon-
DR, Sand PK. Evaluation of a new once-daily
76. Zinner NR, Mattiasson A, Stanton SL.
tinence related to detrusor hyperactivity:
formulation of oxybutynin for the treatment
Efficacy, safety, and tolerability of extended-
oxybutynin versus propantheline versus pla-
of urinary urge incontinence. Urology 1999;
release once-daily tolterodine treatment for
cebo. J Urol 1991;145:813-7.
overactive bladder in older versus younger
89. Fantl JA, Cardozo L, McClish DK. Estro-
65. Birns J, Lukkari E, Malone-Lee JG.
patients. J Am Geriatr Soc 2002;50:799-807.
gen therapy in the management of urinary
A randomized controlled trial comparing
77. Sussman D, Garely A. Treatment of
incontinence in postmenopausal women:
the efficacy of controlled-release oxybutynin
overactive bladder with once-daily extend-
a meta-analysis: first report of the Hormones
tablets (10 mg once daily) with conventional
ed-release tolterodine or oxybutynin: the
and Urogenital Therapy Committee. Obstet
oxybutynin tablets (5 mg twice daily) in pa-
Antimuscarinic Clinical Effectiveness Trial
tients whose symptoms were stabilized on
(ACET). Curr Med Res Opin 2002;18:177-
90. Sultana CJ, Walters MD. Estrogen and
5 mg twice daily of oxybutynin. BJU Int 2000;
urinary incontinence in women. Maturitas
78. Ouslander J, Maloney C, Grasela T, Rog-
66. Appell RA, Sand P, Dmochowski R, et
ers L, Walawander C. Implementation of a
91. Fantl JA, Bump RC, Robinson D, Mc-
al. Prospective randomized controlled trial
nursing home urinary incontinence man-
Clish DK, Wyman JF. Efficacy of estrogen
of extended-release oxybutynin chloride and
agement program with and without toltero-
supplementation in the treatment of urinary
tolterodine tartrate in the treatment of over-
dine. J Am Med Dir Assoc 2001;2:207-14.
incontinence: the Continence Program for
active bladder: results of the OBJECT Study.
79. Diokno AC, Appell RA, Sand PK, et al.
Women Research Group. Obstet Gynecol
Mayo Clin Proc 2001;76:358-63.
Prospective, randomized, double-blind
67. Davila GW, Daugherty CA, Sanders SW.
study of the efficacy and tolerability of the
92. Ouslander JG, Greendale GA, Uman G,
A short-term, multicenter, randomized dou-
extended-release formulations of oxybuty-
Lee C, Paul W, Schnele J. Effects of oral es-
ble-blind dose titration study of the efficacy
nin and tolterodine for overactive bladder:
trogen and progestin on the lower urinary
and anticholinergic side effects of transder-
results of the OPERA trial. Mayo Clin Proc
tract among female nursing home residents.
mal compared to immediate release oral ox-
J Am Geriatr Soc 2001;49:803-7.
ybutynin treatment of patients with urge uri-
80. Burgio KL, Locher JL, Goode PS. Com-
93. Oesterling JE. Benign prostatic hyper-
nary incontinence. J Urol 2001;166:140-5.
bined behavioral and drug therapy for urge
plasia: medical and minimally invasive treat-
68. Dmochowski RR, Davila GW, Zinner
incontinence in older women. J Am Geriatr
ment options. N Engl J Med 1995;332:99-
NR, et al. Efficacy and safety of transdermal
Soc 2000;48:370-4.
oxybutynin in patients with urge and mixed
81. Ouslander JG, Schnelle JF, Uman G, et
94. DuBeau CE, Yalla SV, Resnick NM. Im-
urinary incontinence. J Urol 2002;168:580-6.
al. Does oxybutynin add to the effectiveness
plications of the most bothersome prosta-
69. Abrams P, Freeman R, Anderstrom C,
of prompted voiding for urinary incontinence
tism symptom for clinical care and outcomes
Mattiasson A. Tolterodine, a new antimus-
among nursing home residents? A placebo-
research. J Am Geriatr Soc 1995;43:985-92.
carinic agent: as effective but better tolerat-
controlled trial. J Am Geriatr Soc 1995;43:
95. Thomas AW, Abrams P. Lower urinary
ed than oxybutynin in patients with an over-
tract symptoms, benign prostatic obstruc-
active bladder. Br J Urol 1998;81:801-10.
82. Mattiasson A, Blaakaer J, Høye K, Wein
tion and the overactive bladder. BJU Int
70. Jonas U, Hofner K, Madersbacher H,
AJ, Tolterodine Scandinavian Study Group.
2000;85:Suppl 3:57-68, 70-1.
Holmdahl TH. Efficacy and safety of two
Simplified bladder training augments the
96. Debruyne FM, Witjes WP, Fitzpatrick J,
doses of tolterodine versus placebo in pa-
effectiveness of tolterodine in patients with
Kirby R, Kirk D, Prezioso D. The interna-
tients with detrusor overactivity and symp-
an overactive bladder. BJU Int 2003;91:54-60.
tional terazosin trial: a multicentre study of
toms of frequency, urge incontinence, and
83. Mazur D, Wehnert J, Dorschner W,
the long-term efficacy and safety of terazosin
urgency: urodynamic evaluation. World
Schubert G, Herfurth G, Alken RG. Clinical
in the treatment of benign prostatic hyper-
J Urol 1997;15:144-51. [Erratum, World
and urodynamic effects of propiverine in pa-
plasia. Eur Urol 1996;30:369-76. [Erratum,
J Urol 1997;15:210.]
tients suffering from urgency and urge in-
Eur Urol 1997;31:458.]
february 19, 2004
Downloaded from www.nejm.org at BERKSHIRE MED CTR on August 21, 2006 .
Copyright 2004 Massachusetts Medical Society. All rights reserved.
97. Lepor H, Williford WO, Barry MJ, et al.
the Department of Veterans Affairs Cooper-
112. Smith CP, Franks ME, Phelan MW, et
The efficacy of terazosin, finasteride, or
ative Study Trial. J Urol 2003;170:145-8.
al. Botulinum toxin A: physiologic and clin-
both in benign prostatic hyperplasia. N Engl
104. Weiss JP, Blaivas JG. Nocturia. J Urol
ical effects on the lower urinary tract. J Urol
J Med 1996;335:533-9.
98. Lepor H, Kaplan SA, Klimberg I, et al.
105. Miller M. Nocturnal polyuria in older
113. Schurch B, Stohrer M, Kramer G,
Doxazosin for benign prostatic hyperplasia:
people: pathophysiology and clinical impli-
Schmid D, Gaul G, Hauri D. Botulinum-A
long-term efficacy and safety in hyperten-
cations. J Am Geriatr Soc 2000;48:1321-9.
toxin for treating detrusor hyperreflexia in
sive and normotensive patients. J Urol 1997;
106. Asplund R, Aberg H. Diurnal variation
spinal cord injured patients: a new alterna-
in the levels of antidiuretic hormone in the
tive to anticholinergic drugs? Preliminary
99. Lepor H. Phase III multicenter placebo-
elderly. J Intern Med 1991;229:131-4.
results. J Urol 2000;164:692-7.
controlled study of tamsulosin in benign
107. Idem. Desmopressin in elderly subjects
114. Brendler CB, Radebaugh LC, Mohler
prostatic hyperplasia. Urology 1998;51:
with increased nocturnal diuresis: a two-
JL. Topical oxybutynin chloride for relax-
month treatment study. Scand J Urol Neph-
ation of dysfunctional bladders. J Urol 1989;
100. Lepor H, Williford WO, Barry MJ,
rol 1993;27:77-82.
Haakenson C, Jones K. The impact of medi-
108. Ouslander JG, Nasr SZ, Miller M, et al.
115. Martin SW, Radley SC, Chess-Williams
cal therapy on bother due to symptoms,
Arginine vasopressin levels in nursing home
R, Korstanje C, Chapple CR. Relaxant ef-
quality of life and global outcome, and fac-
residents with nighttime urinary inconti-
fects of potassium-channel openers on nor-
tors predicting response. J Urol 1998;160:
nence. J Am Geriatr Soc 1998;46:1274-9.
mal and hyper-reflexic detrusor muscle. Br J
[Erratum, J Am Geriatr Soc 1999;47:481.]
101. Roehrborn CG, Van Kerrebroeck P,
109. Johnson TM II, Miller M, Pillion DJ,
116. Sharma A, Goldberg MJ, Cerimele BJ.
Nordling J. Safety and efficacy of alfuzosin
Ouslander JG. Arginine vasopressin and
Pharmacokinetics and safety of duloxetine,
10 mg once-daily in the treatment of lower
nocturnal polyuria in older adults with fre-
a dual-serotonin and norepinephrine re-
urinary tract symptoms and clinical benign
quent nighttime voiding. J Urol 2003;170:
uptake inhibitor. J Clin Pharmacol 2000;40:
prostatic hyperplasia: a pooled analysis of
three double-blind, placebo-controlled
110. Lose G, Lalos O, Freedman RM, van
117. Chancellor MB, de Groat WC. Intra-
studies. BJU Int 2003;92:257-61.
Kerrebroeck P, Nocturia Study Group. Effi-
vesical capsaicin and resiniferatoxin thera-
102. Boyle P, Robertson C, Manski R, Pad-
cacy of desmopressin (Minirin) in the treat-
py: spicing up the ways to treat the overac-
ley RJ, Roehrborn CG. Meta-analysis of ran-
ment of nocturia: a double-blind placebo-
tive bladder. J Urol 1999;162:3-11.
domized trials of terazosin in the treatment
controlled study in women. Am J Obstet
118. Silva C, Ribeiro MJ, Cruz F. The effect
of benign prostatic hyperplasia. Urology
of intravesical resiniferatoxin in patients
111. Mattiasson A, Abrams P, Van Kerre-
with idiopathic detrusor instability suggests
103. Johnson TM II, Jones K, Williford WO,
broeck P, Walter S, Weiss J. Efficacy of desmo-
that involuntary detrusor contractions are
Kutner MH, Issa MM, Lepor H. Changes in
pressin in the treatment of nocturia: a dou-
triggered by C-fiber input. J Urol 2002;168:
nocturia from medical treatment of benign
ble-blind placebo-controlled study in men.
prostatic hyperplasia: secondary analysis of
BJU Int 2002;89:855-62.
Copyright 2004 Massachusetts Medical Society.
apply for jobs electronically at the new nejm careercenter
Physicians registered at the new NEJM CareerCenter can now apply for jobs electronical-
ly using their own cover letters and CVs. You can now keep track of your job-application
history with a personal account that is created when you register with the CareerCenter
and apply for jobs seen online at our Web site. Visit www.nejmjobs.org for more
information.
n engl j med 350;8
february 19, 2004
Downloaded from www.nejm.org at BERKSHIRE MED CTR on August 21, 2006 .
Copyright 2004 Massachusetts Medical Society. All rights reserved.
Source: http://www.berkshirehealthsystems.net/documents/Internal%20Medicine%20Resident%20Curriculum/Appendix%20C%20-%20Supplemental%20Readings/Geriatrics/Management%20of%20Overactive%20Bladder.pdf
NCRD's Business Review : e-Journal, Volume 2, Issue 2 (Jan-Dec 2016) ISSN: 2455-0264 A STUDY ON YOUTH'S GREEN BUYING BEHAVIOR WITH SPECIAL REFERENCE TO DOMBIVLI, MUMBAI Mr. Mathew Lawrence, Ph.D Research Scholar ABSTRACT Business organizations need to contribute significantly to healthily environment through the adoption of green marketing. The activities of some of this business may result to environmental pollution which makes the environment becomes inimical to human habitation. India is still in its nascent stage of developing green and sustainable marketing strategies. In India majority population is young. Any behavioral change among youth can create a huge turnaround for any company as well as entire country. This study throws light on green marketing and its impact on youth. The research is conducted with probing questions on environmental awareness, knowledge, and perception of consumers towards green marketing and perceived barriers faced by consumers in adopting green marketing. Both primary and secondary data has been used for the research. Exploratory research was carried out; convening sampling technique has been used. Sample Size was 500 respondents from Dombivli area. Data has been analyzed using SPSS. Research findings reveal that green marketing is more effective than regular marketing. Keywords: Green Marketing, Youth, Attitude, Perception INTRODUCTION Industries around the world have started the green initiative to counter ill effects of business processes particularly transformation and consumption of products on natural environment and its inhabitants. Today citizens and policy makers across the world are focused on issues such as terrorism and economic meltdown. But at the same time environmental issues also remain high on list of concern. Green marketing research has come a long way. Consumers from the developed countries including USA and Western Europe were found to be more conscious about the environment (Curlo, 1999). Research in the last decade(Lee, 2008 2009, Rahbar and Wahid, 2011, D Souza 2004) has indicated those consumers are aware and are willing to pay more to "go green". Green marketing came into prominence in the late 1980s and early 1990s; it was first discussed much earlier. The American Marketing Association (AMA) held the first workshop on "Ecological Marketing" in 1975. The proceedings of this workshop resulted in one of the first books on green marketing entitled "Ecological Marketing". According to Polonsky (1994) green or environmental marketing consists of all activities, designed to generate and facilitate any exchange intended to satisfy human needs and wants, such that the satisfaction of these needs and wants occur with minimum detrimental impact on the natural environment. LITERATURE REVIEW Green marketing is a vital constituent of the holistic marketing concept today. It is particularly applicable to those businesses that are directly dependent on the physical environment. Changes in the physical environment may pose threat to fishing, processed foods tourism and adventure sports industries. (Yasmin and Shamshuddin; 2014) There is no one single strategy that will work for all companies, it all depends on the own individual objectives, target market, resources
Journal of Ecology 2012, 100, 950–957 Interspecific differences in determinants of plantspecies distribution and the relationships withfunctional traits Masahiro Aiba*†, Hino Takafumi and Tsutom Hiura Tomakomai Research Station, Field Science Center for Northern Biosphere, Hokkaido University, Takaoka,Tomakomai 053-0035, Japan 1. Environmental control and dispersal limitation are both essential processes in plant communityassembly and species distribution. Although numerous studies in the past decade have examinedtheir importance as determinants of community composition, remarkably little is known aboutinterspecific differences in the importance of these two processes.2. To quantify these interspecific differences, we compared the importance of environmental fac-tors and space as correlates of species distribution among 24 understorey plant species in a Japanesecool–temperate forest by performing variation partitioning at the species level. Specifically, wehypothesized that the importance of environment and space differs among species, and these differ-ences can be partly predicted from the functional traits and ⁄ or phylogenetic identity of each species.3. The unique contributions of both environment and space were significant in the community-levelanalysis. However, at the species level, the relative and absolute sizes of the unique contributions ofenvironment and space differed considerably among the 24 species. Environment and space werenot necessarily significant variables explaining the distribution of many species.4. No significant relationships were found between the unique contribution of environment and thefour functional traits tested, that is, dispersal mode, seed mass, plant height and specific leaf areaamong the 24 species. In contrast, the unique contribution of space was significantly larger in specieswith no dispersal mechanisms than in animal-dispersed species. No significant phylogenetic signalwas detected for the unique contribution of environment or space, suggesting that importance ofenvironmental control and dispersal limitation as determinants of species distribution is evolution-arily labile.5. Synthesis. Our results suggest that the relative and absolute importance of different processes ofcommunity assembly (i.e. environmental control and dispersal limitation) differs remarkablyamong species even within a single community. These interspecific differences may be explained inpart by interspecific differences in dispersal mode.