Neonatal abstinence syndrome – risk factors, recognition, and management
Neonatal Abstinence Syndrome – Risk Factors, Recognition, and Management Lauren A. Johnson-Robbins, MD
Associate in Neonatology Janet Weis Children's Hospital
Identify risk factors based on prenatal and
neonatal history for NAS
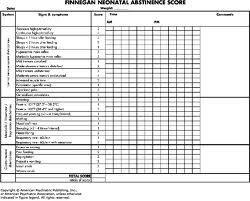
Discuss the application of the Finnegan
score in managing NAS
Review the preferred agents for medically
In the news -
STORY HIGHLIGHTS
Tennessee ranks among the top states
dealing with prescription drug abuse
About half of all babies in intensive care at one
hospital suffer from drug withdrawal
Opioids, like oxycodone, are the
main drugs in these babies' systems
Most are diagnosed with
neonatal abstinence syndrome, or NAS
Number of US newborns
with drug withdrawal triples
Researchers find that a baby is born
every hour in the US with signs of
opiate drug withdrawal
Actually not surprising: Number of newborns
in drug withdrawal triples in last decade
12:18 pm May 1, 2012, by Theresa Walsh Giarrusso
From 2000-2009 in the US, 5-fold increase
in rate of mothers using opioids at time of delivery
Antepartum opioid use increased from 1.19 to
5.63 per 1,000 births.
NAS from 1.2 to 3.39 per 1,000 births
Concurrently costs to provide care rose
Neonatal Abstinence Syndrome
What is NAS? NAS refers to a constellation of
typical signs & symptoms of withdrawal that occur in infants that have been exposed to, and have developed dependence to, certain illicit drugs or prescription medications during fetal life.
Characterized by CNS irritability, gastrointestinal
dysfunction, and autonomic abnormalities.
Maternal Risk Factors
No prenatal care Preterm Labor Previous unexplained fetal demise Intermittent hypertensive episodes Cerebrovascular accidents Severe mood swings or bizarre behavior Placental abruption or repeated spontaneous
History of STD's History of physical and/or sexual abuse History of substance abuse Incarceration Clinical evidence of substance abuse in family
But the reality is that many women
do not fit into one of these categories.
Neonatal Risk Factors
Unexplained IUGR or prematurity
Unexplained microcephaly
Abnormal CNS exam (jitteriness,
hypertonicity, irritability, poor state control)
Unexplained cerebral infarct
Vomiting and diarrhea associated with
typical symptoms of withdrawal
Drugs & Substances of Abuse
Drugs/substances of abuse based on frequency
Cigarettes (most common) Alcohol Marijuana Non-medical uses of prescription drugs Cocaine Hallucinogens Heroin (least common)
Substances associated with NAS
Opiates/opioids – heroin, morphine, codeine,
opium, methadone,buprenorphine, fentanyl, demerol, percodan, darvon, oxycodone,….
Benzodiazepines – valium, librium, placidyl,
xanax, atarax,….
Barbiturates
Substances
not associated with NAS
Cocaine, antidepressants (except SSRI's), and/or
amphetamines - may experience symptoms that resemble NAS but are actually toxic effects of these drugs on the CNS
Caffeine, marijuana, tobacco, and volatile
substances have been associated with abnormal neurobehavioral findings that typically subside within a few days & for which only supportive care is indicated.
Selective inhibitor of neuronal reuptake of
serotonin (ex. Paxil, Prozac).
Literature showing an association with
withdrawal, particularly with paroxetine.
At peak use, up to 20 to 30% of babies exposed
in utero to SSRI's
WHO in February 2005 came out recommending
Paxil not be used during pregnancy.
Treatment for Substance Abuse during Pregnancy -
Methadone first used to treat drug dependency in the 1960's. Began using in pregnancy in the 1970's. Methadone clearance changes during pregnancy typically
leading to a need to increase the dose.
Suboxone/Subutex
Buprenorphine is a C-III controlled substance Prescribing this agent to outpatients requires special approval
Providers must undergo training program and then complete the
DEA application process
Use during pregnancy instead of methadone increasing
Subutex/Suboxone Use in Pregnancy
MOTHER Study – NEJM 2010
Randomized treatment-naïve pregnant women
to methadone vs. buprenorphine
Buprenorphine-exposed newborns had an
average LOS of 10 days vs.17.5 for methadone-exposed
Conclusion: Safe alternative to methadone
during pregnancy
Neonatal Screening
Committee on Substance Abuse of the American
Academy of Pediatrics recommends a comprehensive medical and psychological history including specific information related to maternal drug use as part of every newborn evaluation.
Most states do not require (including PA) written
consent from parents to obtain a tox screen in a newborn but hospitals may have their own guidelines/requirements.
Screening of all patients at delivery is not
Timing of onset of symptoms is variable
and depends on the drug(s), timing, and amount of last maternal use, as well as maternal and infant metabolism, and rate of excretion.
Majority of withdrawal start within 72 hours
ONSET of SYMPTOMS
Neonatal Evaluation
Collect meconium and/or urine for toxicology
screen – know what your drug screen tests for.
Begin NAS scoring 2 to 4 hours after birth If clinically indicated - CBC, sepsis work up,
metabolic screen, and/or neurologic evaluation.
Screen for hepatitis B, HIV, and STD
Precludes early discharge.
Certain facilities keep infants through day of life 5.

A tool that gives a quantitative measure of
the severity of symptoms of withdrawal.
Tracks progression and then response to
Attempts to standardize.
Requires nursing staff to be proficient in
the use and application of this tool.

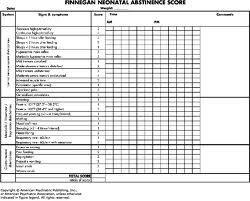


Finnegan Scoring -
CNS symptoms – Irritability Tone Sleep pattern

Treatment First try supportive non-pharmacological
interventions – successful <30% of the time
Quiet, private environment for care w/ dim lighting. Frequent feedings of regular or hypercaloric formula
(methadone is not contraindicated in breast feeding)
Swaddling, rocking, swinging. Soft music Pacifier Soft bedding to minimize excoriations – contradicts
SIDS recommendations.
Frequent diaper changes
Pharmacologic Therapy
Drug therapy must be individualized. Infants with Finnegan scores below 7 do not
require drug therapy.
Pharmacologic therapy is indicated when scores
are consistently (three consecutive scores) above 8 despite comfort measures.
Vomiting & diarrhea associated with dehydration
due to narcotic withdrawal are indications for treatment even in the absence of high abstinence scores.

Drugs for the Treatment of NAS
Drug choice determined by
Availability
Agent from which infant is withdrawing –
opiates are only for opiate withdrawal.
Personal preference
AAP supports oral morphine or tincture of
Oral Morphine Solution
Must be diluted to 0.4 mg/ml (available as 4
mg/ml or 2 mg/ml)
Equivalent to tincture of opium and paregoric
Has no additives or high alcohol content
Has a short half life making it ideal for treatment
Has the least effect on sucking
Tincture of Opium
Has no additives or high alcohol content
Must dilute to 0.4 mg/ml (available as 10 mg/ml)
Has a short half life
Improves sucking quickly
Superior treatment for GI symptomatology
Associated with a lower incidence of seizures
than with any other drugs.
Drug of choice for non-opiate and alcohol
Suppresses agitation well Has no effect on diarrhea or other GI symptoms High doses may impact feeding Has a long half life Does not prevent seizures due to opiate
Several small studies looking at neonatal
Still at the feasibility stage
Non-narcotic that effectively reduces
withdrawal symptoms
Should be used with caution with a short
Several small feasibility trials where it was
found to shorten amount/time opioids were used for NAS
Dosing for Oral Morphine or Tincture of Opium
Dose (give q 4 hours)
If scores continue to increase, or an
adequate response is not achieved within 12 hours, the dose may be increased by 0.16 mg/kg/day increments.
Consider adding Phenobarbital if CNS
symptoms cannot be controlled with opiates alone. Phenobarbital: load with 10-15 mg/kg followed by 3-5 mg/kg/day.
Not contraindicated with methadone
Contraindicated with cocaine, heroin, and heavy alcohol use
Conflicting recommendations on suboxone Contraindicated in HIV-positive mothers Mother's with hepatitis should be
counseled that while breastfeeding is not contraindicated, theoretically viral transmission may occur.
Discharge Planning
Length of hospitalization varies depending on
drug used, severity of withdrawal, and social factors.
Need to establish close follow up with PCP Parental education should be ongoing
throughout the hospitalization and must include signs & symptoms of withdrawal.
Early Intervention and/or Developmental Follow

Questions…….
Source: http://www.dauphincms.org/NeonatalAbstinenceSyndrome.pdf
PHARMACOLOGICAL PRINCIPLESPsychopharmacology, one of the most active and developing areas of psychiatric research, is the use of psychotropic medication to treat psychiatric disorders. Psychiatric–mental health nurse practitioners (PMHNPs) must have a thorough understanding of the science and art of prescribing—of the pharmacokinetic and pharmacodynamic actions of a given drug, as well as the client's motivation to take the drug. The basic pharmacological principles are discussed in this chapter.
Part 13: First Aid: 2010 American Heart Association and American Red Cross International Consensus on First Aid Science With Treatment Recommendations David Markenson, Jeffrey D. Ferguson, Leon Chameides, Pascal Cassan, Kin-Lai Chung, Jonathan L. Epstein, Louis Gonzales, Mary Fran Hazinski, Rita Ann Herrington, Jeffrey L. Pellegrino, Norda Ratcliff and Adam J. Singer