Introduction
ESSEX PALLIATIVE AND SUPPORTIVE CARE NETWORK
FORMULARY AND GUIDELINES FOR MANAGEMENT
Updated April 2010
CONTENTS
Introduction
General Principles
Principles of Prescribing in Palliative care
Syringe Drivers
Emergencies in Palliative Care
Steroids in Palliative Care
Care of the Dying
Pain Control
Gastrointestinal Symptoms
Anorexia and Cachexia
Nausea and Vomiting
Constipation
Diarrhoea
Bowel Obstruction
Malignant Ascites
Mouth Care
Respiratory Symptoms
Breathlessness
Cough
Hiccups
Other Common Symptoms
Urinary Symptoms
Agitation
Skin Care (including pressure and wound care)
Lymphoedema
General References and Further Reading
INTRODUCTION
"Palliative care is an approach that improves the quality of life of patients and their families facing the
problem associated with life-threatening illness, through the prevention and relief of suffering by means of
early identification and impeccable assessment and treatment of pain and other problems, physical,
psychosocial and spiritual" WHO (2002)
Generic palliative care (the palliative care approach) is provided by all health care professionals and is an
integral part of clinical practice.
The specialist palliative care team becomes involved with patients with an extraordinary level of need. This
often reflects an intensity or complexity of problems across the physical, psychological or spiritual domains.
Fast and effective palliation of symptoms is of utmost importance in ensuring best possible quality of life in
individuals for whom cure is not possible. The following formulary has been written not as a comprehensive
text but as a guide on first line management of common symptoms encountered in palliative care for adults.
Advice is based on clinical evidence (where possible) and nationally and internationally accepted guidelines
for best practice. The authors acknowledge that symptom control and other issues should be approached in
a holistic way, taking into account not only physical signs but also social, spiritual and emotional dimensions.
Users who wish to gain greater depth and breadth of reading are advised to refer to specialist palliative care
texts (see further reading).
This formulary was devised on behalf of the Essex Palliative and Supportive Care Network by a small
working party with representation from the Acute Trusts, Community Trusts and Voluntary Sector health
care providers across the Network.
For further specialist advice please contact:
Hospital Macmillan Teams
Monday – Friday 9am –5pm
Basildon Hospital:
extension 3088 (hospital switchboard 0845 1553111)
Broomfield Hospital:
extension 4503 (hospital switchboard 08448220002)
Essex County Hospital (Colchester): 01206 744018 Southend Hospital:
Community Macmillan Teams
Mid- Essex:
Monday – Friday
South West Essex:
Monday – Friday
South East Essex:
Monday – Friday
St Francis Hospice (for Brentwood): 01708 758610 Monday – Friday
Out of Hours Specialist Palliative Care Telephone Advice Service
Mid Essex
Farleigh Hospice:
North Essex
St Helena's Hospice: 01206 845566
South East and South West Essex
Southend Hospital:
01702 435555 and ask for consultant on call for palliative medicine
Brentwood
St Francis Hospice: 01708 753319
Hospice contacts
Fair Havens Hospice, Southend
Fair Havens Hospice-at Home
Farleigh Hospice, Chelmsford
St Francis Hospice, Romford
St Helena's Hospice, Colchester
St Luke's Hospice, Basildon
St Luke's Hospice-at Home
PRINCIPLES OF PRESCRIBING IN PALLIATIVE CARE
1. Assess the symptom(s) adequately 2. Establish a realistic management plan with the patient and family 3. Choose drugs based on underlying pathology and physiology 4. Choose an appropriate route of drug administration 5. Avoid polypharmacy where possible 6. Review
7. Ensure appropriate quantities of medication are available
SYRINGE DRIVERS
Syringe drivers are small battery operated pumps that allow continuous, subcutaneous drug infusions. This
permits parenteral drug administration with minimal patient burden and has the advantage of steady plasma
levels for a wide range of drugs available for symptom control. They are not just for use in the terminal
phase but in any situation where the oral route is inappropriate or unreliable. There are 3 syringe driver
models currently in use across the network. These are the Graseby MS16A, Graseby MS26 and McKinley
T34. For guidance regarding setting up a syringe driver use the Syringe Driver Care Pathway and refer to
local policies.
THE USE OF GRASEBY AND MCKINLEY SYRINGE DRIVERS IN PALLIATIVE CARE
ENTRY CRITERIA FOR ACTIVATION OF PATHWAY
Patient has symptom control needs and
is not tolerating or absorbing medication
or 2. the drug is unavailable as an oral medication
Assess current symptom control needs
• Give PRN dose of appropriate drug if required
Explain to patient/family rationale for using syringe driver
Convert oral medication to 24 hour subcutaneous route (see palliative care section in local drug formulary for guidance)
Decide which type of syringe driver you will be using?
Prescribe syringe driver
Rate should be written as length in mms of liquid over 24 hours for Graseby syringe drivers
The volume of drugs and diluent combined in a McKinley T34 pump will normally be to 15 mls unless otherwise stated
Check compatibility of drugs in syringe driver (maximum of 4 drugs mixed at any one time)
Check diluent – most drugs for subcutaneous administration should be mixed with water for injection or normal saline
Ensure PRN medications available for subcutaneous use for break-through symptoms
McKinley T34
Blue model rate delivered in mm per
The rate is delivered as mls
Green model rate delivered as mm over 24
hour, length in mm ÷ time of drug delivery
per hour over 24 hrs
i.e. 24 hrs = rate in mm per hour
Gather equipment required
Mix drugs and diluent in luer lock syringe and attach to 22 g butterfly giving set.
For Graseby syringe drivers, measure syringe contents length in mms to work out rate and prime the line.
Ensure syringe driver is in good working order e.g. battery is
working, syringe driver has been serviced in the last year.
Fit the syringe securely to the driver (see Graseby or Mckinley T34
Instruction Manual for further information). With a McKinley T34, this
must be done before siting the needle.
In discussion with the patient, choose an appropriate subcutaneous site to
insert the butterfly and secure in place, avoiding oedematous areas, bony
prominences, skin folds and irradiated or broken skin
Ensure the syringe driver is running correctly
Monitor the syringe driver regularly as per local policy
If not working correctly, refer to instruction manual and local syringe driver policies for "trouble shooting"
Complete clinical incident form if there is a problem with the timing of drug delivery
Monitor the infusion site for signs of in
t on or leakage at cannula sit
on or leak
age at cannula sit (
e the cannula
sited if ther is the presence of the above
esence of the above .
itation of drugs in
icular if using a co
Are patients symptoms adequately controlled?
Use PRN medications to control
Adjust 24 hour dose/drug requirements in syringe driver
• Review regularly
Consider referral to the Palliative Care Team
• If stable for long periods
or Pain Team (depending on patient's underlying condition)
can oral medications be
reinstated and syringe driver
(return to entry criteria)
EMERGENCIES IN PALLIATIVE CARE
Where possible it is always desirable to pre-empt problems that could arise. However, sometimes
unpredictable or unavoidable emergencies happen. When managing palliative care emergencies, always
consider the following when determining what level of intervention is appropriate
The nature of the emergency
Performance status of patient
Disease status and prognosis
Effectiveness and potential toxicity of treatment
Wishes of patient and carers and the capacity of the patient to consent to treatment
Hypercalcaemia
Hypercalcaemia is the commonest life threatening metabolic disorder occurring in patients with advanced
cancer.
Definition – corrected calcium >2.6mmol/1.
Often only symptomatic >3.0mmol/1.
Levels of >4.0mmol/1 will cause death in a few days if untreated.
Incidence is 10% overall, but varies depending on the primary malignancy
Can be 20-40% in breast cancer, lung cancer (not small cell) haematological malignancies and some
squamous cell carcinomas.
Pathophysiology
Local osteolytic effect (20%) metastatic tumour grows in the bone and activates osteoclasts.
Humeral mechanisms (80%) promote osteoclast activity and bone resorption.
It is a poor prognostic factor, with 80% patients surviving less than 1year from onset.
Assessment
Clinical features:
Symptoms are often mistaken for opioid effects or attributed to the underlying malignancy, so a high index of
suspicion is needed
Check U&Es and corrected calcium
Mild (calcium <3.0)
Moderate(calcium 3.0-4.0) Severe (calcium .4.0)
Lethargy Fatigue Dehydration
Nausea and vomiting
Polyuria and polydipsia
SYMPTOMS AND SIGNS OF HYPERCALCAEMIA
There may be some overlap as presentation varies between individuals
Management
Treatment is for symptomatic purposes – it will not affect the course of the underlying disease but if left
untreated impairs quality of life and may hasten death. There is a need to consider the overall clinical
condition and prognosis of patient before instigating treatment: it may not be appropriate to treat a moribund
patient
Should consider treatment if: Plasma calcium is >2.8 Symptomatic
First episode of hypercalcaemia or significant interval since previous episode
Acute treatment
Mild hypercalcaemia (corrected calcium<3.0mmol/1)
Rehydration
Encourage oral intake.
Only treat further if symptomatic, then manage as below
Moderate or severe hypercalcaemia (corrected calcium >3.0mmol/1)
Rehydration
Consider IV fluids 3-41/24h if oral intake inadequate.
Can lower calcium by 0.3mmol/1.
Adjust rate if renal or cardiac failure present.
Replace potassium as necessary.
Repeat U&E daily and adjust fluids as necessary.
Stop drugs causing hypercalcaemia
Vitamin D compounds Thiazide diuretics
Drug therapy
Drugs affecting bone mineralisation and metabolism:
Intravenous bisphosphonates (first line therapy) Calcitonin: give in addition to bisphosphonates for severe life threatening hypercalcaemia when rapid response is needed. Corticosteroids (for potentially steroid sensitive tumours)
Symptomatic management
Antiemetics (see section on nausea and vomiting)
Laxatives or rectal intervention (see section on constipation)
Mouthcare
Consider maintenance therapy Refer to oncologist for consideration of disease modifying treatment/anti tumour therapy Hormonal therapy. Chemotherapy Radiotherapy. Regular bisphosphonates IV bisphosphonates every 3-4 weeks. There is no need to limit dietary calcium intake, as intestinal calcium absorption is suppressed
Pharmacological management
1. Bisphosphonates
These act by inhibiting osteoclast activity and bone resorption
Disodium Pamidronate
90mg IV in 250ml N. Saline over 2-4 h
Adjust rate in renal failure
If U&Es abnormal need to prehydrate
Takes 36-48 hours for serum calcium to start to respond
Maximum effect after 5-7 days
Duration of action approx. 3 weeks
Zolendronic acid
4mg IV in 100ml N. Saline over 15 min
Same dose in mild-moderate renal failure (serum creatinine <400).
If U&Es abnormal need to prehydrate
Takes 24-36 h for serum calcium to respond
Maximum effect after 5-10 days
Duration of action 3-4 weeks
2. Calcitonin
Inhibits osteoclast activity and renal tubular reabsorption of calcium
200-400 units SC qds for 24-48 h. Acts within 12h. Duration of action 2-3 days Relapse may be delayed by concurrent use of steroids if the tumour is steroid sensitive
3. Corticosteroids
Can be used in conjunction with calcitonin for potentially steroid sensitive tumours
Take 3-4 days to work
Spinal Cord Compression
Compression of the spinal cord or cauda equina (nerve roots below L1) can lead to permanent paraplegia or
quadriplegia
Incidence – 3-5% overall, more common in myeloma, prostate, breast and lung cancers.
It is a poor prognostic factor with 70% of patients dying within 1 year.
Cause: 80% due to extradural compression e.g. collapse of vertebral body caused by destructive lesion. 20% due to intradural compression e.g. primary spinal cord tumour. Site: 70% thoracic 20% lumbar 10% cervical
Assessment
Have a high index of suspicion in view of need for rapid treatment to avoid permanent neurological deficit
Usually in a patient with known metastatic disease
Clinical features
Above L1 – upper motor neurone signs
Below L1 – lower motor neurone signs.
SYMPTOMS & SIGNS OF SPINAL CORD COMPRESSION
Symptoms
Back pain (early) >80
Local bone pain Root compression pain Radicular pain, worse on Coughing Altered sensation >50%
• Pins and needles
Upgoing plantars
Sphincter disturbance (late) 40
Urinary retention
• Urinary retention
• Constipation
Loss of saddle sensation (late)
SYMPTOMS & SIGNS OF CAUDA EQUINA COMPRESSION
Symptoms
Sciatic pain (often bilateral
Peri-anal numbness
Loss of Saddle sensation (late)
Investigations
Urgent MRI of the whole spine
Management
Start treatment as soon as the diagnosis is suspected, do not delay until there is radiological confirmation
Steroids
Dexamethasone 16mg PO/IV stat. Continue 16 mg/day orally (or IV if patient unable to take orally) Urgent referral to appropriate team for consideration of
Radiotherapy or
Surgical decompression
Severity of symptoms and time to commencement of treatment determine outcome
If ambulatory, 70% remain so.
If paraplegic, 5% become ambulatory.
CHOOSING APPROPRIATE COURSE OF MANAGEMENT
Poor performance status
Good performance status
Likely prognosis <3 months
Likely prognosis >3 months
Multiple sites of compression
Well localised site of compression
Radiosensitive tumours
Radio-resistant tumours
Helps pain control
Need for tissue for diagnosis
Superior Vena Caval Obstruction (SVCO)
Venous obstruction usually due to tumour within the mediastinum
Incidence – 3-5% in lung cancer and lymphoma
It is a poor prognostic factor with >80% of patients dying within 1 year.
Causes
Extrinsic pressure
Direct invasion of vessel wall
Intraluminal clot
Assessment
Clinical features
Chest x-ray
CT scan
CLINICAL FEATURES OF SVCO
Dyspnoea
Tachypnoea
Headache
Suffused injected conjunctivae
Dizziness
Cyanosis
Distended non pulsatile neck veins
Dilated collateral superficial veins of upper
Visual changes
Swelling
(esp.peri-orbital
Facial and peri-orbital
• Arms and hands
Management
Dexamethasone 16mg IV / PO stat.
Continue 16mg / day orally (or IV if patient unable to take orally)
Urgent referral to appropriate team for consideration of
Radiotherapy
Chemotherapy in chemo-sensitive tumours e.g. small cell lung cancer
SVC stent insertion
Symptomatic management
Oxygen
Opioids +/- benzodiazepines for dyspnoea (see section on respiratory symptoms).
Severe Haemorrhage
In a patient already close to death, occurrence of a severe haemorrhage is often a terminal event and
resuscitation measures are not appropriate. Such a haemorrhage is perhaps one of the most dreaded of all
terminal events and, if witnessed, can be extremely distressing to all involved. The goal of management of
the event must be to minimise anxiety and ensure death with dignity, providing a calm reassuring
atmosphere
Major Forms
Haematemesis/malaena
Haemoptysis
Rectal bleeding
Vaginal bleeding
Erosion of major blood vessels by malignant ulcer
Guidelines for the event in hospital
It is important that the following equipment is available
Suction as appropriate
Call bell: for support for staff to aid with administration of medication
Gloves and apron
Green/blue or other dark towels
Reassurance for carers
Professional presence
Patients should be nursed in a side ward to avoid shock and distress to other patients and relatives where
possible
Guidelines for the event at home
It is important that the following equipment is available in the event of a severe haemorrhage at home. They
should be stored discreetly but be readily available and accessible
Gloves and apron
Green/blue or old dark towels
Suction as appropriate
Yellow waste bags
Treatment
Anxiolytic (e.g. midazolam 5 – 10mg IV/IM, diazepam 10mg PR/IM)
If there is an element of pain give:
Analgesic (e.g. diamorphine 5 – 10mg IV/IM or patient's usual breakthrough dose
What to do
1. Above all, do not panic. Try to keep the patient calm, stay with them, talk gently to them and hold their hand. If possible try to keep them in one place i.e. laid on the bed or sat in the chair. 2. Apply towels/pillows to bleeding site to absorb the bleeding if possible 3. Administer medication 4. Call for assistance.
After the event
Stay with relatives for a chance to de-brief and support as appropriate. Staff will also need support after the event and may need to talk through the incident fully with a healthcare professional of their choice
Subject Specific References
Kovacs C S. Hypercalcaemia of malignancy in palliative care patients: A treatment strategy.
Journal of Pain
and Symptom Management1995;
10(3): 224-232
Ralston S. Management of cancer associated hypercalcaemia.
European Journal of Palliative Care 1(4):
170-174
Feber, T.
Head of Neck Oncology Nursing. London: Whurr Publishers Ltd, 2000
Smith A M.
Emergencies in Palliative Care. Annals Academy of Medicine, 1994;
23 (2): 186-190.
STEROIDS IN PALLIATIVE CARE
Steroids are used for a variety of specific and non-specific reasons in patients with progressive
malignancies. Up to 40% of patients may require them at some stage of their illness.
Indications
INDICATIONS FOR USE OF STEROIDS IN ADVANCED MALIGNANCY
Specific Non-specific
Spinal cord compression (SCC)
Superior vena cava obstruction (SVCO)
Raised intra-cranial pressure (ICP)
Nausea and vomiting
Cerebral tumours
Malignant pyrexia
Lymphangitis carcinomatosis
Oesophageal obstruction
Bowel obstruction
Biliary obstruction
Liver capsule pain
Nerve compression pain
Obstructive lymphadenopathy
Choice of steroid
Current practice is to use dexamethasone in patients with advanced malignancy.
It has mainly glucocorticoid action.
High relative glucocoticoid potency means lower doses are needed compared with other steroids.
Drug
Relative dose
Biological half-
life
Hydrocortisone 20mg
Prednisolone 5mg 18-36h Methyl-
prednisolone Dexamethasone 0.75mg
Initiating steroids
Monitor patient closely for symptomatic response.
Wean to lowest effective dose to minimise potential side effects.
When reducing dose, allow time on new dose to assess whether there is any deterioration (at least 3-4
days).
Consider use of gastro-protection, especially if on concurrent NSAIDs.
Regular urinalysis for glucose in all patients and closely monitor BMs if known diabetic.
Dose
There is little evidence-based data on dosage. These guidelines follow current conventional best practice.
DEXAMETHASONE DOSE FOR SPECIFIC INDICATIONS
Up to 16mg
Anorexia Lymphangitis
Nausea and vomiting
Nerve compression pain
Cerebral tumours
Biliary obstruction
Malignant pyrexia
Bowel obstruction
Liver capsule pain
Oesophageal obstruction
Route:
Dexamethasone is available in injectable form for IV or SC use and as tablets or syrup for oral use.
Oral is as effective as IV/SC if there are no concerns about oral drug absorption.
If dysphagia or vomiting give SC either stat or as a continuous infusion.
Frequency:
Dexamethasone has a long biological half-life so can be given once daily.
Single daily dose in morning or if on high dose can split dose twice daily.
Give all doses before lunchtime to avoid insomnia (e.g. 0800 for once daily or 0800 and 1200 for twice daily
dosing).
Side effects:
Doses of 4mg of dexamethasone /day or more are likely to lead to side effects after several weeks:
Fluid retention.
Cushingoid changes e.g. moon face.
Skin changes e.g. bruising and striae.
Increased risk of infection.
Neuro-psychiatric side effects e.g. insomnia and euphoria.
Gastric irritation when used in conjunction with NSAIDS.
Hyperglycaemia, either worsening of pre-existing diabetes or new onset.
Proximal myopathy (medium term use).
Osteoporosis (long term use).
Stopping steroids:
If no symptomatic benefit within 1 week of starting treatment, discontinue.
Often have a limited duration of action (2-4 weeks) so need to review response regularly and stop once no
longer benefiting.
If on treatment for less than 2 weeks and dose<6mg dexamethasone equivalent can stop abruptly.
If on treatment for more than 2 weeks or dose >6mg dexamethasone equivalent need to titrate down to avoid
adrenal crisis.
CARE OF THE DYING
Recognition of the terminal phase
Increasing weakness and immobility
Loss of interest in food and fluid
Difficulty in swallowing
Often develops over days to weeks
Care should be guided by an integrated care pathway for the last days of life (e.g. Liverpool Care Pathway)
Assessing the needs of the patient
Focus on what the patient perceives as problems
Remember symptoms are often under-reported
Non-verbal cues of distress may be present
Explore fears
Assessing the needs of the family
Check their understanding of the situation
Address any fears or misunderstandings
Ensure they have adequate professional support
Think about risk factors for a difficult bereavement
Principles of symptom control in the terminal phase
Rationalise regular medication – can/should anything be stopped?
Anticipate the route of drug administration - does parenteral medication need to be used/available?
Ensure the availability of drugs for new symptoms that may arise
Review regularly
Noisy respiration
Often occurs because patient is too weak to clear secretions Usually more distressing for carers than for patient May respond to appropriate positioning (semi-recumbant) Can use anticholinergics:
Hyoscine hydrobromide 0.4mg stat and 1.2-2.4mg/24hrs (SC)
Hyoscine butylbromide 20mg stat and 60-120mg/24hrs (SC) Glycopyrronium 0.2mg stat and 0.6-1.2mg/24hrs (SC)
If possibility of heart failure consider furosemide 40mg stat
Where possible continue previously effective analgesia
May need to consider change in route- injections, continuous subcutaneous infusions, suppositories
Opioids
Diamorphine or morphine sulphate is the usual drug of choice for parenteral administration, unless the patient
is already maintained on an alternative step 3 opioid or is in renal failure
Divide total daily dose of oral morphine by 3 to give equivalent daily dose of parenteral diamorphine
Remember to prescribe parenteral breakthrough analgesia at 1/6th of the equivalent daily dose of regular
opioid
NSAIDs
Some can be given as suppositories e.g. diclofenac
Injectable forms (diclofenac, ketorolac) can be given as single injections or as a continuous subcutaneous
infusion
Neuropathic pain
Continue oral agents where possible
Clonazepam (injectable form) can be used subcutaneously (as a daily injection or as a continuous
subcutaneous infusion) if oral agents are not practical (0.5-4mg/24hrs)
Restlessness and agitation
Exclude reversible cause's e.g. urinary retention, drug therapy, hypercalcaemia Treat contributory symptoms e.g. pain Ensure calming environment If symptoms persist consider drug therapy midazolam 2.5-5mg stat and 10-120mg/24hrs (SC)
levomepromazine 12.5-25mg stat and 12.5-150mg/24hrs (SC) haloperidol 2.5mg – 5mg stat and 5-20mg/24hrs (SC)
Nausea and vomiting
Think about the likely cause
Reverse the reversible if appropriate
Choose an anti-emetic based on the probable cause – see nausea and vomiting.
Dry mouth
See Mouth Care
There is no evidence that parenteral fluids improve a dry mouth
Anticipatory prescribing
Ensure medication is prescribed and available on an as required basis for symptoms that commonly arise
during the terminal phase. This would usually include:
Analgesic: diamorphine (or oxycodone) sc at 1/6 total 24 hour dose
Antiemetic: cyclizine 50mg sc, haloperidol 1.5-5mg sc, levomepromazine 6.25-25mg sc
Anxiolytic: midazolam 2.5-5mg sc, levomepromazine 12.5 -25mg sc
Anti-sialogogue: hyoscine hydrobromide 0.4mg sc, hyoscine butylbromide 20mg sc, glycopyrronium 0.2mg sc
Subject Specific Reference
National Council for Hospice and Specialist Palliative Care Services.
Changing Gear – Guidelines for
Managing the Last Days of Life in Adults. London:
National Council for Hospice and Specialist Palliative Care
Services, 1997.
PAIN CONTROL
"Pain is what the patient says hurts" (Twycross, 1997)
Cancer pain may be due to:
1. The disease itself 2. Treatment (e.g. radiotherapy, chemotherapy) 3. Unrelated to either the cancer or its treatment
An understanding of the underlying pathophysiology of the pain will aid its treatment
Pain assessment
Site
Severity
Timing
Quality/description
Radiation
Provoking factors
Relieving factors
Analgesic history
Analgesics tried
Dosages
Timing
Duration of treatment
Efficacy
Side effects
Classification of pain
Nociceptive - Somatic
Visceral
Neuropathic - Nerve compression
Nerve
Principles of analgesic use:
By mouth where possible: avoid intramuscular/intravenous routes where possible in palliative care patients –
subcutaneous absorption is generally as good
By the clock (i.e. regularly)
By the WHO ladder
Remember to prescribe appropriate analgesia for breakthrough pain at 1/6th total 24 hour dose
Monitor response to treatment and modify accordingly
WHO Analgesic Ladder
Opioid for moderate to severe pain +/-non-opioid +/- adjuvants
Opioid for mild-moderate pain
+/-non-opioid +/- adjuvants
Step 1. Non-opioid: Paracetamol/ NSAID Adjuvants: Tricyclic antidepressants,
Anticonvulsants, antiarrhythmics, corticosteroids.
Step 2. Opioids for mild-moderate pain: codeine (co-codamol 8/500, co-codamol 30/500),
dihydrocodeine (codydramol 10/500), tramadol
Step 3. Opioids for moderate-severe pain: morphine, oxycodone, hydromorphone,
fentanyl, diamorphine, methadone, buprenorphine
Paracetamol
Preparations:
Tablets: 500mg
Dispersible tablets: 500mg
Oral suspension: 250mg/5ml
Suppositories: 500mg, 1g
Dose:
1g qds not more often than 4hrly, maximum dose 4g/24hrs
Indications:
Mild-moderate pain
Pyrexia
Non-steroidal anti-inflammatory drugs (NSAIDs)
Of particular benefit in pain associated with inflammation
Choice of NSAID often dictated by benefit: adverse effect profile
Suggested drugs:
Diclofenac 150mg/24hrs (tablets, dispersible tablets, suppository, continuous subcutaneous infusion)
Ibuprofen 400-600mg tds-qds (tablets)
Naproxen 250-500mg bd (tablets, suspension)
Ketorolac 30-60mg/24hrs via continuous subcutaneous infusion (for severe inflammatory pain)
Consider concurrent use of a gastroprotective agent for at risk patients
Opioid analgesics
Morphine sulphate
The opioid of first choice for moderate to severe cancer pain
Oral Preparations;
Immediate release: liquid 10mg/5ml and 100mg/5ml or tablets 10mg, 20mg, 50mg
Sustained release over 12 hours: tablets 5mg, 10mg, 15mg, 30mg, 60mg, 100mg, 200mg; capsules 10mg, 30mg, 60mg, 100mg, 200mg; or granules 20mg, 30mg, 60mg, 100mg, 200mg Sustained release over 24 hours (capsules): 30mg, 60mg, 90mg, 150mg, 200mg
Injectable preparations Morphine sulphate 10mg/ml, 15mg/ml, 20mg/ml and 30mg/ml available in 1ml and 2ml ampoules Approximately 2 x as potent as oral morphine sulphate
Guidelines for use:
Initiating morphine analgesia
Talk to the patient: allay any fears or concerns
Start a low dose of regular morphine (5-10mg 4 hourly in patient previously on weak opioids)
Write dose in mg not mls
Remember to prescribe breakthrough analgesia (1/6th of total 24 hour dose available up to hourly if needed)
Co-prescribe a laxative
Ensure an anti-emetic is available eg haloperidol 1.5-5mg
Assess for pain relief and side effects
If pain still present and opioid sensitive, increase dose by 30-50%
When analgesic requirements are stable convert to a sustained release preparation
Diamorphine
Injectable Preparation: Injection (powder for reconstitution): 5mg, 10mg, 30mg, 100mg, 500mg ampoules Diluent: water for injection
Indications: First choice strong opioid if injectable form required (alternative to morphine sulphate injection)
Guidelines for use: Can be given as single injections or as continuous subcutaneous infusion via syringe driver Approximately 3 times more potent than oral morphine, therefore to convert oral morphine to subcutaneous diamorphine give 1/3 of the oral dose
Oxycodone
Oral Preparations;
Immediate release: liquid 10mg/10ml and 100mg/10ml; or capsules 5mg, 10mg, 20mg
Sustained release over 12 hours (tablets): 10mg, 20mg, 40mg, 80mg
Indications;
Patients with opioid sensitive pain experiencing side effects (particularly psychogenic) with morphine
Patients with moderate renal failure or for breakthrough dosing in patients with severe renal failure
Guidelines for use;
See morphine For dose conversion from morphine refer to table
Injectable Preparations 10mg/ml solution: 1ml and 2ml ampoules, 50mg/ml solution Can be given as single injections or as continuous subcutaneous infusion via syringe driver Approximately twice as potent as oral oxycodone therefore to convert oral oxycodone to subcutaneous oxycodone give ½ of the oral dose Has approximately the same potency as subcutaneous diamorphine therefore when converting from subcutaneous diamorphine use the same dose (NB be aware of potential differences in dose with different dose conversion methods)
Fentanyl, transdermal
Preparations;
Self-adhesive patch. Different patch sizes deliver 12, 25, 50, 75 and 100mcg/hr
Indications;
Patients with opioid sensitive pain experiencing side effects with morphine
Patients unable to take oral opioids
Patients with intractable morphine-induced constipation despite regular use of appropriate laxatives
Patients in renal failure
Guidelines for use;
Patch changed every 72 hours
Takes 36-48 hours to reach steady state plasma concentrations
Elimination plasma half life is 15-17 hours
Inappropriate for patients who need rapid titration of severe uncontrolled pain
For dose conversion from morphine refer to table.
Fentanyl, transmucosal
Available in oral, buccal and sublingual preparations
Indications;
Rapidly escalating, unpredictable breakthrough pain in patients already on regular strong opioids e.g. incident
pain
Not intended as first choice breakthrough analgesia for patients on transdermal fentanyl
Guidelines for use; Pain relief occurs rapidly (5-15 minutes) Dose titration needed in each patient under supervision from specialist palliative care team. Dose cannot be predicted from dose of regular strong opioid. Doses of each preparation are not equivalent.
Methadone
Preparations;
Tablets: 5mg
Linctus: 2mg/5ml
Solution: 1mg/ml, 10mg/ml, 20mg/ml
Injection: 10mg/ml in 1ml, 2ml, 3.5ml and 5ml ampules
Indications;
Patients with opioid sensitive pain experiencing side effects with morphine
May be more effective than morphine for neuropathic pain
Guidelines for use;
Long and unpredictable plasma half-life (8-75 hours)
Highly lipophilic, accumulates in tissues creating potentially extensive reservoir
Dose requirements should be titrated under specialist palliative care supervision, usually as an in-patient
When dose requirements stable, taken 8 hourly or 12 hourly
Injectable form can be given by continuous subcutaneous infusion, give ½ of the daily oral dose over 24 hours
Alfentanil
Synthetic derivative of fentanyl with a short plasma half life (100mins) metabolised in liver to inactive
compounds
10 times more potent than diamorphine
Used mainly via CSCI for patients in renal failure who require regular step 3 opioids where there is evidence of
morphine toxicity
For use under specialist palliative care supervision
Buprenorphine
A partial opioid agonist
Self-adhesive patch delivers drug transdermally and changed every 4 days (TransTec)
Special pain situations
Neuropathic pain
Variable opioid sensitivity. Try WHO analgesic ladder.
Consider co-analgesia:
Tricyclic antidepressants:
Amitripyline 10-75 mg nocte Lofepramine 70-210 mg nocte Start at low dose and increase as tolerated. May take up to one week before analgesic effect apparent
Anticonvulsants: Clonazepam 0.5-4mg nocte Sodium Valproate 0.2-1g nocte Gabapentin 0.3 – 0.8g tds Pregabalin 75 – 300mg bd Start at low dose and increase as tolerated. May take up to one week before analgesic effect apparent.
Anti-arrhythmics:
Mexilitine 50-200mg tds Start at low dose and increase as tolerated. May take up to one week before analgesic effect apparent
Consider: TENS, nerve blocks
Bone pain
Use WHO analgesic ladder and consider:
NSAIDs: as above
Steroids: Dexamethasone 8mg daily
Bisphosphonate: Disodium Pamidronate 90mg or Zolendronic acid 4mg by IV infusion repeated every 3-4
weeks if effective
Bisphosphonates should be given in conjunction with calcium supplements and vitamin D. Assess dental state
prior to commencing bisphosphonates and suspect osteonecrosis of the jaw if the patient develops jaw pain.
Other measures to consider: radiotherapy, surgery for actual or potential long bone fractures
Liver capsule pain
Use WHO analgesic ladder and consider: Steroids: dexamethasone 8mg daily NSAIDs: as above
Bowel colic
Relatively opioid insensitive Consider hyoscine butylbromide (Buscopan): 10-20mg qds PO, 40-120mg/24hrs by continuous subcutaneous infusion See section on bowel obstruction for management of colic in this situation
Muscle spasm
Relatively opioid insensitive Consider:
Diazepam 2-10mg tds PO
Baclofen 5-30mg tds (start at 5mg tds and increase by 5mg tds every 2-3 days: avoid in patients with cerebral
metastases/tumour due to risk of fits)
TENS may be useful
KETAMINE
May be useful as a co-analgesic in neuropathic, inflammatory or ischaemic pain.
Available in hospitals and in the community on a named patient and named pharmacy basis
Should be initiated and titrated under specialist palliative care supervision
Dose range 10-200mg tds-qds PO or 100-2400mg/24hrs via continuous subcutaneous infusion
References:
Grond S et al. Assessment and treatment of neuropathic cancer pain following WHO Guidelines
. Pain 1999;
79: 15-20.
Hanks, GW et al. Morphine and alternative opioids in cancer pain: the EAPC recommendations
. British Journal
of Cancer 2001;
84(5): 587-593.
Mannix, K et al. Using bisphosphonates to control the pain of bone metastases: evidence based guidelines for
palliative care.
Palliative Medicine 2000;
14: 455-461
McQuay, H et al. Anti-convulsant drugs for the management of pain: a systematic review.
British Medical
Journal 1995;
311: 1047-52
McQuay, HJ et al. A systematic review of antidepressants in neuropathic pain.
Pain 199
6; 68: 217-227.
Equivalent Doses of Morphine and Related Opioids
Oral treatment
Parenteral treatment
Transdermal
Morphine
Oxycodone
Morphine
Diamorphine
Fentanyl
4 Hour immediate
12 Hour controlled
24 Hour controlled
4 to 6 Hour immediate release
12 Hour modified release
72 Hour controlled
release tabs/liq
release tabs e.g.
release caps e.g.
caps/liq e.g. Oxynorm 5mg,
tabs e.g. OxyContin 5mg,
release patch e.g.
e.g. Sevredol, Oramorph
10mg, 20mg, 5mg/5ml
10mg, 20mg, 40mg, 80mg
Every 4 hours
Every 4 to 6 hours
Every 12 hours
Every 72 hours
100 micrograms/h
125 micrograms/h
175 micrograms/h
Note 1: When opioids are prescribed prophylactic laxatives should be prescribed concurrently to treat constipation, eg: Senna, Docusate. Note 2: When long acting preparations are used, always prescribe a short acting immediate release preparation equivalent to the plain release dose for breakthrough pain. Note 3: When starting opioid-based analgesia, nausea can occur for the first 7 – 10 days and an antiemetic may be required. Note 4: Oxycodone and Diamorphine may be considered equivalent, on a mg for mg basis, when given as a continuous infusion in a syringe driver. This chart is a guide only. For full details see individual data sheets.
Equivalent Doses of Morphine and Related Opioids
Oral treatment
Parenteral treatment
Additonal information
Morphine
Morphine
Alfentanyl
Oral Codeine and Oral Morphine
Oral Codeine may be considered to be 1/10 the potency of
4 Hour immediate release
12 Hour controlled
24 Hour controlled
4 Hour injection S/C
Continuous infusion S/C
Oral Morphine e.g. 10mg oral codeine = 1mg oral
release tabs e.g.
release caps e.g.
e.g. Sevredol, Oramorph
Morphine (ratios of 1/8 & 1/6 have been quoted so further adjustments may need to be made within the 1st 24hours)
Every 4 hours
Every 4 hours
Over 24 hours
Tramadol
Equivalence varies according to route:
Injection: 100mg Tramadol = 10mg Morphine
Oral: 50mg Tramadol = 10mg Morphine
Oral Transmucosal Fentanyl Preparations
e.g. Lozenges, sublingual tablets, orodispsersible tablets
There are currently no defined conversion ratios and for
this reason morphine/oxycodone are recommended for breakthrough pain when Fentanyl patches are being used.
Each of the oral transmucosal Fentanyl preparations need
to be individually titrated according to manufacturers recommendations.
Buprenorphine Patches
These are not recommended locally due to difficulties in
escalating doses and converting to other agents. Transtec is a 96hr patch licensed for cancer pain
Butrans is a 7day patch licensed for non-malignant pain.
Note 1: When opioids are prescribed prophylactic laxatives should be prescribed concurrently to treat constipation, eg: Senna, Docusate. Note 2: When long acting preparations are used, always prescribe a short acting immediate release preparation equivalent to the plain release dose for breakthrough pain. Note 3: When starting opioid-based analgesia, nausea can occur for the first 7 – 10 days and an antiemetic may be required. Note 4: Oxycodone and Diamorphine may be considered equivalent, on a mg for mg basis, when given as a continuous infusion in a syringe driver. This chart is a guide only. For full details see individual data sheets.
ANOREXIA-CACHEXIA SYNDROME AND FATIGUE
Anorexia-cachexia syndrome
Loss of appetite and weight loss are common in patients with malignancies, occurring in 70-80% of patients.
Due to a combination of direct tumour effects, systemic tumour effects and treatment.
Assessment Evidence of weight loss
Dietary history
Biochemistry e.g. serum albumin
Exclude/treat reversible causes
Oral problems e.g. candida
Nausea and vomiting
Dysphagia
Oesophagitis
Non-pharmacological management
Explanation and reassurance to patient and family.
Nutritional counselling and supplements.
May prevent further weight loss. No evidence for weight gain or improved quality of life.
Pharmacological management
1.
e.g. Dexamethasone 4mg od (give as single dose no later than lunchtime).
Improves appetite. Weight gain uncommon, may occur due to fluid retention. Decreases fatigue. Rapid onset of action. May have limited duration of action (approx. 4-6 weeks), but helpful in patients with short prognosis. Stop after 1 week if no benefit. If develop side effects or prognosis is longer than weeks, consider decreasing to 2mg.
Progestogens e.g. Megestrol acetate 160 – 800 mg od or split doses. e.g. Medroxyprogesterone 400mg –1600mg od.
Improves appetite.
Weight gain (both fat and lean muscle).
Decreases fatigue
Delayed onset of action (approx. 2-4 weeks), so limited use in patients with short prognosis.
Duration of action months.
If have longer prognosis but need rapid symptomatic benefit, can consider starting corticosteroid and
Progestogen simultaneously and tailing off steroids after 3-4 weeks as Progestogen starts to have effect.
3.
Prokinetic agents
e.g. Metoclopramide 10mg tds
Helpful in early satiety and chronic nausea related to gastroparesis.
Fatigue
Fatigue and lethargy are common symptoms in patients with malignancies. They have a significant impact on
both physical and psychological functioning in daily life. Causes are multi-factorial, related to both cancer and
its treatment.
Assessment
Activities of daily living
Exercise tolerance
Sleep patterns
Exclude/treat reversible causes
Anaemia
Biochemical abnormalities
Depression
Drug side-effects
Non-pharmacological management
Explanation and reassurance to patient and family
Exercise
• Aerobic exercise helpful both during and after treatment
There is no evidence currently to support energy conservation strategies or nutritional input.
Pharmacological management
Corticosteroids (see previous)
Progestogens (see previous)
Psychostimulants
• In limited situations under specialist guidance only
DRUGS USED IN THE TREATMENT OF NAUSEA AND VOMITING
SITE OF ACTION
MECHANISM
DRUG INDICATION/USE
DOSE/ROUTE
/RECEPTORS
CYCLIZINE
Raised intracranial pressure
Bowel obstruction
CSCI 100-150mg over 24h
HYOSCINE
Bowel obstruction
CSCI 1.2-2.4mg over 24h
5-HT2, Dopamine,
Broad spectrum, unknown cause PO 6.25-25mg od
Acetylcholine & Histamine
or treatment failure
SC 3.125-25mg tds
CSCI 12.5-75mg over 24h
BENZODIAZEPINE e.g.
Fear and psychological stimuli
LORAZEPAM
e.g. anticipatory nausea FIRST LINE
CEREBRAL CORTEX &
Anti-inflammatory
CORTICOSTEROID e.g.
GASTROINTESTINAL
Bowel obstruction
CSCI 4-16mg over 24h
Dopamine antagonist
HALOPERIDOL
Opioid-induced vomiting
Biochemical causes e.g.
hypercalcaemia, uraemia
CSCI 3-5mg over 24h
Dopamine, 5-HT3 antagonist,
Gastric stasis, squashed stomach PO 10-30mg tds/qds
and oesophageal reflux
GASTROINTESTINAL
CSCI 30-100mg over 24h
Opioid-induced vomiting
Biochemical causes SECOND LINE
Dopamine antagonist
DOMPERIDONE
Gastric stasis, squashed stomach PO 10-20mg tds/qds
and oesophageal reflux
PR 30-60mg tds/qds
FIRST LINE Opioid-induced vomiting Biochemical causes SECOND LINE
5-HT3 antagonist
Chemotherapy and radiotherapy
PO 8mg bd-tds/1mg bd
GRANISETRON
IV 8mg bd/1mg bd
But avoid otherwise in palliative CSCI 8-24mg over 24h care patients
GASTROINTERSTINAL
HYOSCINE
Bowel obstruction
SC 20mg tds CSCI 60-120mg over 24h
OCTREOTIDE
Bowel obstruction
SC 100-200mcg tds
Somatostatin analogue
Intractable vomiting
CSCI 300-600mcg over 24h
SC = subcutaneous CSCI = continuous subcutaneous infusion
IDENTIFYING SPECIFIC CAUSES OF NAUSEA AND VOMITING
Causes Examples
Drugs and metabolic
• Nausea & retching prominent
• Continuous symptoms
• No relief from vomiting
• Chemotherapy
• History of recent change in
• Hypercalcaemia
• Specific symptoms / signs of
• Renal failure
underlying cause
• Liver failure
• Upper abdominal tumour
• Bloating after food
• Hepatomegaly
• Vomiting after food
• Fullness & discomfort
• Epigastric discomfort
• Blood in stomach
• Resistant to antiemetics
• Drug history
Raised intracranial pressure
• Cerebral primary
• Cerebral metastases
Cranial radiotherapy
• Neurological signs
Intestinal obstruction
• Bowels not open and not
• Constipation
• Abdominal distension
• Colic • Vomiting often relieves nausea
• Faeculent vomiting
• Large volume vomits
Psychological and
• Distress exacerbates existing
• Rarely sole cause of nausea and
Pharyngeal stimulation
• Coughing results in muscle
spasm and vomiting
• Sputum or infection in pharynx
can trigger vomiting reflex
NAUSEA AND VOMITING
Nausea and vomiting are common symptoms in patients with cancer, affecting between 40-70% of patients.
Definitions
Nausea – feeling the need to vomit, often accompanied by autonomic symptoms such as pallor, cold sweat,
salivation and tachycardia.
Retching – laboured, spasmodic movement of the diaphragm and abdominal muscles, often culminating in
vomiting.
Vomiting – the forceful expulsion of gastric contents through the mouth. Involves co-ordinated activity of
diaphragm, GI tract and abdominal muscles, mediated via somatic nerves.
Assessment
It is essential to determine likely cause, as appropriate treatment will depend on this.
History
Pattern of nausea and vomiting
Site of primary and metastases
Ongoing/previous treatment e.g. surgery, radiotherapy
Potential reversible causes
Examination
Abdominal palpation e.g. obstruction
Rectal examination e.g. constipation
Fundoscopy e.g. papilloedema
Oropharynx e.g. candida
Investigations
Consider: FBC/U&E/Calcium
CAUSES OF NAUSEA AND VOMITING
Related to cancer
Related to treatment
Related to concurrent
illnesses or debility
Bowel obstruction
Gastric outflow obstruction
Metabolic disturbance
IDENTIFYING SPECIFIC CAUSES OF NAUSEA AND VOMITING
Causes Examples
Drugs and metabolic
• Nausea & retching
• No relief from vomiting
• Chemotherapy
• History of recent change
• Hypercalcaemia
• Specific symptoms /
signs of underlying
• Bloating after food
• Vomiting after food
• Hepatomegaly
• Fullness & discomfort
Raised intracranial pressure
• Cerebral primary
Cranial radiotherapy
• Neurological
Intestinal obstruction
• Bowels not open and
not passing flatus
• Constipation
• Blood in stomach
• Vomiting often relieves
• Large volume vomits
Psychological and
existing symptoms
• Rarely sole cause of
nausea and vomiting
• Coughing results in
muscle spasm and vomiting
• Sputum or infection in
paharynx can trigger vomiting reflex
Management
Identify and treat reversible causes;
Candidiasis – antifungals.
Constipation – laxatives.
Cough – anti-tussives.
Gastric irritation – H2 antagonist or proton pump inhibitor, stop NSAIDS.
Hypercalcaemia – hydration and bisphosphonates.
Infection – antibiotics.
Non-pharmacological measures;
Calm, reassuring environment.
Avoid sight and smell of food if this precipitates nausea.
Small snacks e.g. few mouthfuls and not big meals.
Complementary therapies e.g. acupuncture.
Pharmacological measures – Antiemetics;
Choose on basis of most likely cause of nausea and vomiting
(see table).
Reassess at regular intervals.
If first choice drug only partially successful or unsuccessful after 24-48h either increase dose or try second line
specific antiemetic.
Combination of antiemetics with different actions may be needed in up to 25% of cases especially where have
multi-factorial causes.
Do not use more than one drug from the same class.
Dexamethasone may be added in to enhance antiemetic effects of other drugs.
If still have treatment failure consider using a broad-spectrum second line agent such as levomepromazine as
a substitute.
Frequency;
Give regularly rather than only "as required".
Route
Prophylaxis
• Use oral route.
• Use parenteral route if there is established vomiting.
• Subcutaneously either as stat doses or by continuous subcutaneous infusion via a syringe driver.
• Can switch back to oral when symptoms controlled, but ensure oral antiemetics are restarted before
syringe driver is stopped.
• Rectal route can also be used.
CONSTIPATION
Defined as the passage of small hard faeces infrequently and with difficulty.
The aim of management is to achieve easy and comfortable defaecation.
Assessment;
When were bowels last open?
Characteristics of last stool? – loose, formed, pellets?
Pain on defaecation
Straining required, hard stool, rectal obstruction?
What is stool frequency now?
Is the urge to defaecate absent? (? colonic inertia)
Is there blood/mucus in the stool?(tumour?haemorrhoids)
Other signs – nausea? bloating? flatulence? abdominal pain? halitosis? faecal soiling?
Examination
Abdominal examination
Rectal examination – empty rectum does not exclude constipation, may be high up impaction.
Investigations
Abdominal X ray (for differential diagnosis of either constipation or obstruction).
Management
Prevention is better than cure
Non-pharmacological
If possible, increase fluid and fibre
Encourage mobility
Assess ability to get to and use the toilet (may need raised toilet seat or commode)
Pharmacological
Commence prophylactic laxatives when starting weak or strong opioids
Use oral laxatives in preference to rectal interventions.
Use a combination of stimulant laxative with a softener/osmotic laxative.
Titrate components to achieve optimum stool frequency and consistency.
If patient is in bowel obstruction – see section on intestinal obstruction.
Comments
management
management
management
Rectum full,
faeces soft
Co-danthramer suppository
Rectum full,
Arachis oil
faeces hard
contains
600 mg daily in 50mg/5ml
peanut oil -
Do not use in
patients with
Colon full,
with colic
Colon full,
with no colic
Impaction
following morning.
DIARRHOEA
Defined as an increase in the fluidity of faeces and possibly the frequency of bowel opening.
It is debilitating for patents with advanced disease and less common than constipation.
Assessment
Patient hydration status – is it appropriate to hydrate orally/parenterally
Exclude reversible causes:
Constipation with overflow
Drug induced diarrhoea (antibiotics, NSAIDs)
Infective diarrhoea
Examination
Palpate abdomen
Stool colour
PR examination to exclude overflow secondary to rectal loading with faeces
Investigations
Stool culture
Management
1. Treat reversible causes. 2. Encourage fluids 3. Loperamide 2 mg after each stool can increase from 2 mg qds. to 4mg qds. 4. Consider codeine 30 – 60 mg qds. if ineffective.
5. Use combination of Loperamide and Codeine.
6. Consider octreotide to reduce high output diarrhoea 300mcg -1000 mcg/24 hrs by continuous
subcutaneous infusion or 100-300mcg tds by SC injection. For patients requiring medium to long term octreotide consider using a depot preparation of octreotide or lanreotide
7. Steatorrhea/fat malabsorption – requires pancreatic enzymes plus PPI. 8. Encourage fluids, lemonade. 9. For patients on opioids - consider converting to SR tablets to IR preparation to improve absorption
INTESTINAL OBSTRUCTION
Assessment
Ascertain the likely site of obstruction based on clinical history and examination i.e. gastroduodenal junction, small bowel or large bowel.
Are there likely to be multiple sites of obstruction? e.g. in history of previous abdominal irradiation or surgery.
Is the patient fit for surgery? Remember that bowel obstruction may not be related to the patients known cancer and that a surgical opinion should be considered.
General principles
1
Drugs should be given parenterally if possible. A syringe-driver is an acceptable way of delivering a combination of drugs for most patients with bowel obstruction.
Avoid NG tubes where possible– these are disliked by patients. Patients often prefer to vomit several times a day rather than have an NG tube inserted.
Allow the patient to eat and drink freely as tolerated.
IV fluids often not necessary but should be considered in those patients who are at risk of rapid dehydration e.g. in gastric outflow and high small bowel obstruction.
Avoid ‘routine' blood tests – they are not necessary in the last few days of life or if the result does not alter clinical management.
6 Simple mouth care is important. 6
Stop all stimulant laxatives (codanthramer, senna) and GI motility stimulants such as metoclopramide and domperidone.
Management
Nausea
Use centrally acting anti-emetics such as:
Haloperidol 3-5mg/24 hrs via continuous subcutaneous infusion Cyclizine 100 – 150 mg/24 hours via continuous subcutaneous infusion Levomepromazine 5 – 15mg/24hrs via continuous subcutaneous infusion Metoclopramide and domperidone can potentially cause abdominal cramps in patients with complete obstruction because of their prokinetic actions. However they can be useful in patients with partial obstruction (use metoclopramide up to 90mg over 24hrs in syringe driver)
Vomiting
Drugs that are useful in reducing the volume of gastrointestinal secretions and therefore the frequency and
volume of vomits are:
Octreotide – start at 300mcg/24 hrs via continuous subcutaneous infusion, this can be increased to 1000mcg
over 24 hours if necessary. Once symptoms stable reduce to lower effective dose. For patients requiring
medium to long term octreotide consider using a depot preparation of octreotide or lanreotide
Hyoscine butylbromide (Buscopan) 60-120mg/24 hrs via continuous subcutaneous infusion
In gastric outflow and small bowel obstruction both drugs may be needed to reduce vomiting to an acceptable
level.
Pain
Hyoscine butylbromide (Buscopan)-
Used in colicky pain. Give stat does of 20mg SC then give 60/120mg/24hrs
Opioids – if the patient is already taking opioids then remember to convert to the appropriate dose of
diamorphine (see morphine conversion chart).
If patient is using fentanyl patches these may be continued rather then switching to diamorphine.
If patient is opioid naïve it may be necessary to add diamorphine to the syringe driver to aid pain control –
Start at a low dose (5 – 10mg/24 hrs) and increase further if appropriate via syringe driver.
Diclofenac – used for inflammatory pain e.g. if peritonitis has developed. Dose 75-150mg/24hrs via continuous subcutaneous infusion. NB Diclofenac does not mix with other drugs and needs a separate syringe driver.
Laxatives
Use ‘softener' laxative such as Docusate sodium 200 mg tds.
It may be necessary to use suppositories and/or enemas if these are tolerated by the patient.
Stop stimulant laxatives
Steroids
Consider 5 day trial Dexamethasone 8mg SC or by continuous subcutaneous infusion
FISTULAE
High output fistulae -
May respond to octreotide 100 mcg tds. by SC injection or 300 - 600 mcg/24 hrs by continuous subcutaneous infusion. For patients requiring medium to long term Octreotide consider using a depot preparation of octreotide or lanreotide
Large bowel fistulae –
Consider using anti-diarrhoeal drugs to constipate the patient.
Remember skin care is important - need to prescribe barrier cream.
MALIGNANT ASCITES
Treatment is aimed at symptom control consider:
Diuretics
Spironolactone100-500mg od If inadequate response add in loop diuretic furosemide 40-80mg od bumetanide
Paracentesis
Periteovenous shunt (for those relatively fit patients requiring repeat paracenteses)
Anticancer therapy
MOUTH CARE
Oral problems are a common feature of advanced disease. Complications frequently develop in the mouth
either as a direct result of malignancy or as an effect of treatment.
Risk Factors
• All advanced disease/debilitation
• Poor oral hygiene • Chemotherapy
• Radiotherapy (increased in local treatment of head & neck)
• Anorexia /reduced fluid /dehydration • Nausea & vomiting
• Drugs (anti emetics/opioids/diuretics/steroids/antibiotics)
Prevention
Regular preventative mouth care can prevent oral problems; promoting comfort Preventative measures should
include high quality oral status assessment and education in order to anticipate problems enhancing effective
management of mouth problems. Tooth brushing is the most effective hygiene care, however Chlorhexidine
helps with plaque control and can be used in control of infections and where brushing teeth is not possible.
People with their own teeth
After food brush teeth twice a day with toothpaste, rinsing well with water
If infection is present
Twice daily Corsodyl (chlorhexidine 0.2%) or Oraldene (hexetidine 0.1%) twice a day, after food. This can be
diluted with equal parts of warm water – all solution must be used. Instruct to swish this around their mouth
and spit it out. If possible, don't eat or drink for 20 minutes.
NB chlorhexidine solutions contain alcohol and should be avoided in patients receiving head and neck
radiotherapy. Alcohol can cause rebound dryness.
Sodium chloride solution or water is suggested for patients who are undergoing head and neck radiotherapy.
People without their own teeth (artificial teeth and other oral appliances)
Remove dentures prior to cleaning your mouth /using mouthwash
Use a very soft (babies) toothbrush or foam swab for cleaning the mouth.
If tooth brush cannot be tolerated prescribe antiseptic mouthwash (Chlorhexidine/ Oraldene) twice a day, after
food. This can be diluted with equal parts of warm water – all solution must be used. Instruct as above
Instruct to clean their dentures by brushing before soaking in denture solution for 30 minutes, brush again with
water. Remove dentures at night, and soak in water to prevent them from cracking or warping
Infection
Mouth infections are common in advanced disease. Consider mouth swabbing to assist in diagnosis and
prevent unnecessary medication. Measures to promote saliva should be considered due to healing properties
of salvia.
Saliva Promotion / replacement
• Sugar free chewing gum
• Oral balance gel four times day
• Foods that encourage chewing
Viral (Zoster or Herpes Simplex)
• Localised to lips topical aciclovir cream five times a day for five to ten days.
• Mouth ulcers may require systemic aciclovir - 200 mg four hourly for seven days – 400 mg if immuno-
Aphthous ulcers
• Tetracycline 250 mg TDS as 3min mouthwash,– (Break capsule into 10 mls water)
• Spit out after, but this can be swallowed.
• Consider steroids topically – hydrocortisone lozenge (pellet) 2.5mg qds for 5 days. Lozenge allowed to
dissolve at the site of the ulcer
Malignant Ulcer
• Characterised by ‘foul odour' suggesting anaerobic infection. Systemic Metronidazole 12 hourly 500
• Topical gel Metronidazole 1% if unable to tolerate systemically. Intention to assist in odour
Candida
Characterised by white adherent patches, angular chelitis, redness, soreness of mouth and throat, treat with
anti-fungals.
• Nystatin (100,000 units/ml) 2-5 ml qds 7 days – not of value prophylactically. Dentures must be
removed each time, and cleaned/sterilised prior to replacing (see before).
• When treated, where nystatin is used in conjunction with chlorhexidine it should be used at least 1 hour
after chlorhexidine used.
• Nystatin has low incidence of resistance, but is time and labour intensive in care situations and has
compliance issues.
Please note - due to the increasing resistance of azole antifungal agents careful consideration prior
to use is advocated.
•
Fluconazole 50 mg – 100 mg od – 7 – 14 days.
If resistant consider switch to Itraconazole 100mg od.
Painful Mouth
Identify cause of pain and manage appropriately. Local analgesics are of use but have relatively short
duration. Where symptoms are related to
head and neck cancer, contact Network Clinical Nurse Specialist
for further advice
Benzydamine spray or mouthwash (Difflam) up to 2 hourly (caution as solution is alcohol based).
Choline Salicylate (Bonjela) 8.7% apply1-2 cm topically 3 hourly
Morphine solutions- Sevredol is preferable to oramorph as it does not contain alcohol. 5-10 mg qds use as a mouthwash, can be swallowed- give specific direction.
Oral Balance gel four times a day. Mechanical protection is of value in adhering to ulcer surface, but difficult to apply. Cytoprotective agents adhere to the ulcer base to create a barrier.
Prescribed morphine in oral balance gel – refer to
specialist pharmacist for advice and
preparation
Carmellose paste (Orabase). Carbenoxolone gel – powder sprinkled onto ulcer
Sucralafate, paste/solution (used in inflammation/mucosistis).
If pain persists manage systemically. Will require frequent reassessment dependant on mouth status, refer to
chapter on pain control.
Dirty / Coated Mouth
The value of mouth hygiene cannot be understated. The use of toothbrush /pink foam swabs to clean teeth,
tongue and gingival mucosa is the most effective tool.
Mouth swabs containing glycerine should not be used as glycerine can cause a rebound drying effect. Swabs
and any product containing lemon or of a citrus nature will make oral ph more acidic and should not be used.
Saliva is the most effective way of maintaining a clean and healthy mouth.
Oral balance gel four times a day
Dry Mouth
This can be as a result of treatment and medication, and directly related to the effects of your illness.
Identify cause and treat where possible e.g. hypercalcaemia, review drug management exacerbating symptom
Sip water/ rinse frequently – moisture will promote comfort
Use sprays of water/ ice chips to refresh their mouth.
Sugar free chewing gum – consider prophylactically when prescribing drugs that will dry mouth – opiates etc.
Oral balance gel four times a day - If they wear dentures, apply to them before wearing. This can be used regularly, which can be especially useful prior to sleeping.
Foods that encourage chewing
Avoid alcohol, as this will increase mouth dryness
• Pilocarpine can be used for xerostomia related to radiotherapy/head and neck cancers and induced
dry mouth. Starting at 5 mgs TDS for drug induced dry mouth. If there is no improvement after 2 days stop. Note can cause side effects –see manufacturer's details.
Dying Person
Meticulous care should be offered as the person is able to tolerate. Where possible family/carer can be
educated and included.
Technique
•
Combine below with 2 hourly cleaning with water (or
patient's choice of liquid) as appropriate.
• Application of (yellow soft paraffin)Oral replacement gel lips
prior to mouth care
• Use of small soft toothbrush is the most effective tool
• If toothbrush not possible tongue, gingiva mucosa should be
cleaned using Pink foam stick or gloved gauze /swabbed finger.
• 12- 6 hourly cleaning of teeth and mouth either with toothbrush
and toothpaste or 'chlorhexidine /hexitidine solution
WELL with tap water (use suction only if
References
1.
Regnard C and Fitton S (1995) Mouthcare. In Regnard C and Hockley (Eds) Flow Diagram in Advanced Cancer and Other Diseases. Edward Arnold . Bath.
British Society for Disability of Oral Health (2000)
Guidelines for the Development of Local Standards of Oral Health Care for Dependent, Dysphagic, Critically Terminally ill Patients.
Multi-Disciplinary Guidelines for the Oral Management of Patients Following Oncology Treatment.
Regnard C and Tempest S (1998) A Guide to Symptom Relief in Advanced Disease. Hochland and Hochland England.
Twycross R, Wilcock A, Charlesworth S and Dickman A (2002) Palliative Care Formulary 2. Radcliffe medical press. Cornwall.
Heals D (1993) A Key to Well Being. Oral Hygiene in Patients with Advanced Cancer. Professional Nurse March 391-398.
British National Formulary.
Twycross R, Wilcock A, Thorp S (1998) Palliative Care Formulary Radcliff
Medical Press Oxon.
Ransier A, Enstein J, Lunn R and Spinelli J (1995) A Combined Analysis of Toothbrush, Foam Stick and a Chlohexidine Soaked Foam Brush in Maintaining Oral Hygiene. Cancer Nursing 18 (5) 393-395
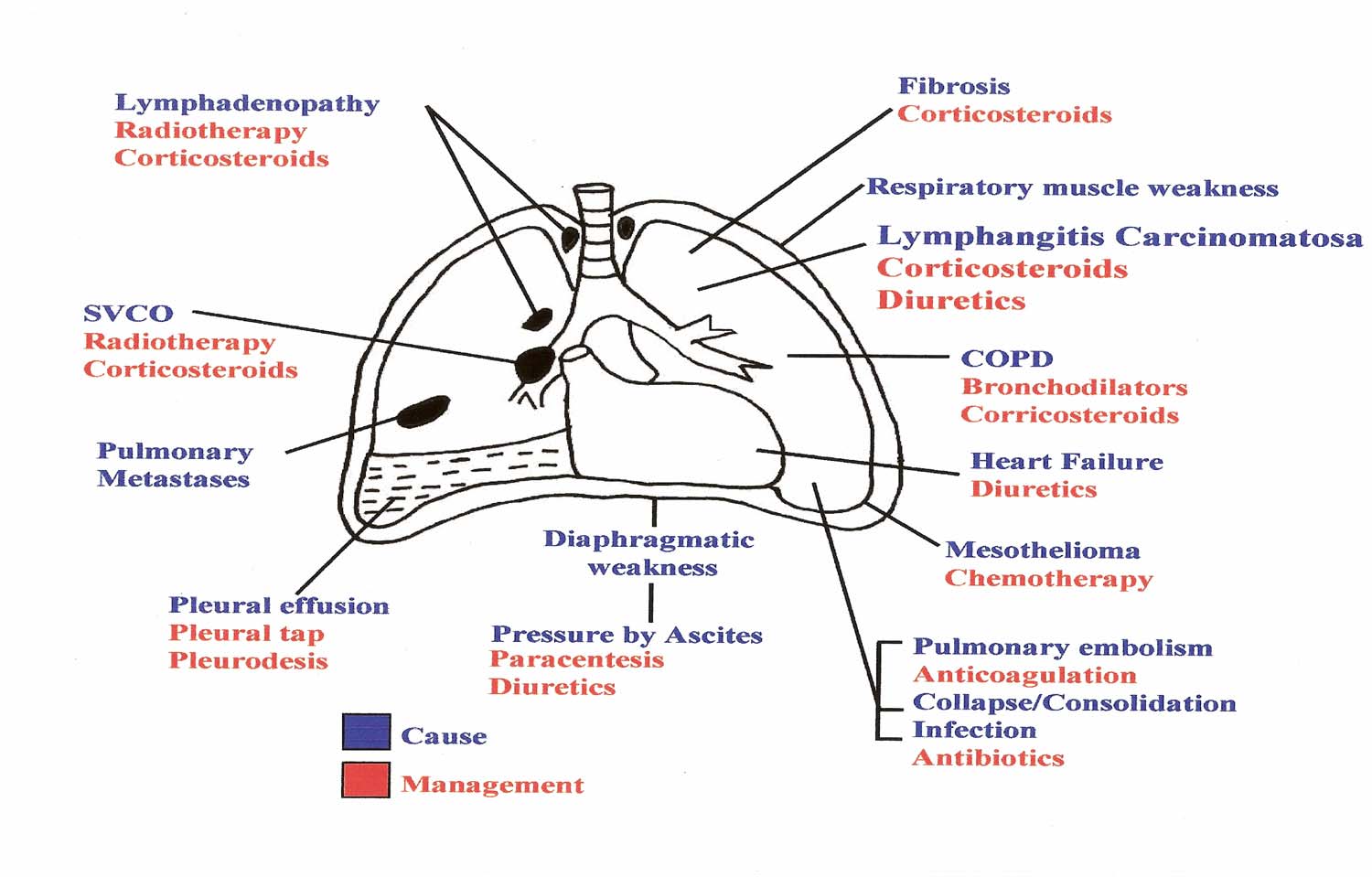
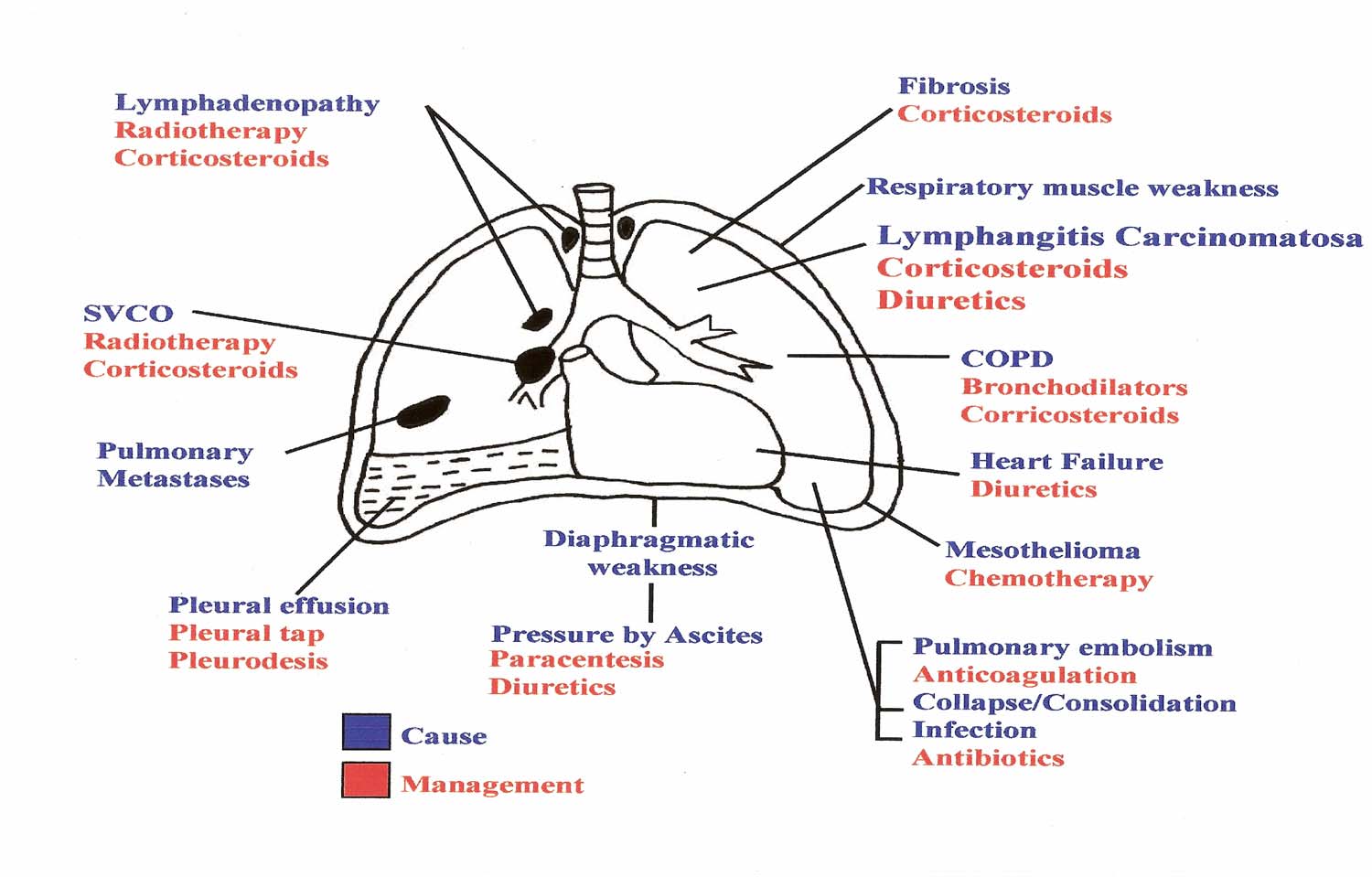
RESPIRATORY SYMPTOMS
BREATHLESSNESS
The pathophysiology of breathlessness is a complex process and one which is not fully understood.
Normal breathing is maintained by regular rhythmical activity in the respiratory centre in the brain stem. This is
stimulated by mechanical stretch receptors in the airways, intercostal muscles and diaphragm, and by hypoxia
and hypercapnia.
In malignant lung disease breathlessness is usually due to distortion and stimulation of the mechanical
receptors.
Breathlessness occurs in 70% of lung cancer patients and in 50% of all patients with a cancer diagnosis. Breathlessness occurs most commonly in cancers of the lung, breast, prostate, colon and rectum. It is often an alarming and distressing symptom and requires prompt and effective palliation.
Symptomatic Management
Non-Pharmacological Measures;
Help patient to address their feelings and fears about the symptom.
Offer reassurance and a calming presence
Cool draft of air across the face e.g. use of a fan
Explain that becoming breathless in itself is not dangerous
Relaxation techniques
Breathing exercises/ re-training
Complementary therapies e.g. massage, reflexology
Advice on modifying activities of daily living
Advice to informal carers on promoting the above measures
Appropriate referral to members of the multi-professional team.
Bronchodilators;
An element of reversible bronchoconstriction may be present.
Try:
Salbutamol 2.5mg-5mg 4 hourly via nebuliser
Ipratropium 250-500 micrograms 6-8 hourly via nebuliser
Saline may alleviate tenacious secretions via nebuliser
Corticosteroids;
Reduction of peri-tumour oedema may improve breathlessness due to multiple lung metastases and in
lymphangitis.
Try:
Dexamethasone 4-8 mg PO daily
Opioids;
Morphine reduces inappropriate and excessive respiratory drive and reduces the ventilatory response to
hypoxia and hypercapnia.
By slowing the respiratory rate, breathing becomes more efficient and reduces the sensation of
breathlessness.
Try:
Morphine 2.5mg PO prn and titrate as for pain
For patients already on regular opioids a dose of the 4 hourly equivalent should be used.
Nebulised opioids
Controlled trials of nebulised opioids suggest they are no more effective than nebulised saline or systemically
administered opioids.
Benzodiazepines
Useful where there is an element of anxiety or panic in a patient who is breathless.
Can be used effectively with opioids.
Try:
Lorazepam 0.5mg- 2mg sublingual prn
Diazepam 2-5mg PO bd-tds +/- prn
Midazolam 2.5-10mg SC prn
Oxygen Therapy
Oxygen may help dyspnoea in patients who are hypoxic either at rest or on exertion. If oxygen saturations are
measured, a trial of oxygen can be given to patients with saturations below 90%. If saturations are above 90%
a beneficial effect is less likely but might still lead to a subjective improvement in selected patients.
Severe COPD patients who have chronic hypoxia should not be given more than 28% oxygen. Blood gas
analysis will identify patients who retain CO2.
Injudicious use of oxygen can lead to CO2 retention in COPD patients, dry airways, pressure sores from nasal
cannulae and masks, restricted mobility and psychological dependency.
Oxygen is a drug and should be prescribed.
Oxygen dries the mucous membranes and humidification should be given if oxygen is required for more than
30 mins at a time. E45 cream can be applied to the nasal area to prevent dryness.
Domiciliary Oxygen
Intermittent or continuous oxygen at home can be prescribed for palliation of breathlessness.
An oxygen concentrator may be required if oxygen is needed for more than 8 hours a day unless it is only for a
short time.
A backup cylinder should be dispensed at the same time as the concentrator.
Oxygen Concentration
Nasal Cannulae 1L/min 24%
2L/min 28%
Venti Mask 2L/min 24%
4L/min 28%
6L/min 35%
References
Booth S., Moosavi SH, Higginson I, The etiology and management of intractable breathlessness in patients
with advanced cancer: a systematic review of pharmacological therapy. Nature Clinical Practice Oncology
2008; 2 (5) 90 – 100
Uronis HE et al; Oxygen relief of dyspnoea in mildly- or non-hypoxemic patients with cancer: a systematic
review and meta-analysis; British Journal of Cancer 2008; 98 (2) 294 - 299
Mcgregor A et al, Oxygen Therapy; End of Life Care 2007; 1 (1) 28-29
COUGH
Cough occurs as a result of mechanical and chemical irritation of receptors in the respiratory tract. The cough
reflex involves afferent nerve transmission to the medulla and efferents to the respiratory muscles.
Persistent episodes of coughing can be exhausting and frightening for the patient.
Causes of Cough:
Treat underlying causes where appropriate.
Cause of cough
Management
Infection Antibiotics
Radiotherapy/chemotherapy/ corticosteroids
LVF / Pulmonary oedema Diuretics Asthma / Bronchospasm
Bronchodilators Corticosteroids
Oesophageal reflux Metoclopramide
Proton pump inhibitor
Refer to speech therapy to assess swallow
Pleural effusion Drainage Radiotherapy induced pulmonary fibrosis
pneumonitis
Symptomatic Management
Productive Cough
For patients still able to cough effectively:
• Nebulised saline 0.9% 2.5-5ml qds and prn to help liquefy tenacious secretions.
• Physiotherapy input to promote effective expectoration.
• Bronchodilator for bronchospasm.
For patients who are too weak to cough and who are dying:
• Antimuscarinic drug to dry secretions e.g. hyoscine hydrobromide 400mcg SC prn • Antitussives (see below)
Dry Cough
Nebulised saline 2.5-5ml qds helps to reduce irritation of dry airways.
Antitussive Drugs:
1
Simple linctus 5-10ml tds
Pholcodine 10ml tds
Codeine 30mg-60mg qds
Morphine 2.5-5mg 4 hourly PO or morphine SR 10mg 12 hourly PO or diamorphine 5-10mg SC over 24 hours via syringe driver.
Consider trial of methadone linctus 2mg/5mls 2.5-5ml od-bd if other measures ineffective.
Nebulised local anaesthetics have been used with some success but have not been well evaluated. Bupivacaine 0.25% or lidocaine 2% 5ml tds can be used but must be administered under close supervision in view of the risk of aspiration. Patients should be pre-treated with nebulised salbutamol to reduce risk of bronchospasm.
HICCUPS
Hiccup is characterized by diaphragmatic spasm.
Persistent hiccups can be a source of significant distress for patients and has the potential to interfere with
normal daily activities of talking, dietary intake and sleeping.
Causes of Hiccup
Vagus Nerve Involvement
Gastic Distention
Gastritis/ Oesophageal reflux
Hepatomegaly
Ascites
Bowel obstruction
Pancreatitis
Phrenic Nerve Irritation
Mediastinal tumour
Diaphragmatic tumour involvement
CNS
Brain stem lesions
Intracranial tumours
Meningitis
Systemic
Renal failure
Addisons disease
Alcohol
Symptomatic Management
Non-pharmacological measures to produce pharyngeal stimulation
For example:
Swallowing dry bread or crushed ice
Forceful tongue traction
Drugs
Metoclopramide 10mg tds
Antiflatulent e.g. asilone 10ml qds if caused by gastric distension
Chlorpromazine 10-50mg tds
Dexamethasone 4-8mg od
Haloperidol 1.5-5mg od tds
Baclofen 5mg-10mg tds
Antacid and / or proton pump inhibitor for gastritis-induced hiccup
OTHER COMMON SYMPTOMS
URINARY SYMPTOMS
Frequency and urgency
Treat reversible causes e.g. infection
Address exacerbating factors e.g. diuretics, hypercalcaemia, hyperglycaemia
Consider practical approaches e.g. proximity to toilet, availability of bottle, commode
Consider anticholinergics
oxybutynin 2.5-5mg bd-qds
Hesitancy
Address reversible causes e.g. anticholinergics, constipation
Consider alpha-adrenoceptor antagonists
indoramin 20mg nocte-bd tamsulosin 0.4mg od (may cause initial hypotension)
AGITATION
Aim is to reduce agitation sufficiently for comfort and to find a treatable cause if possible. 42% of terminal
cancer patients develop terminal agitation.
Consider reversible causes.
Drug induced
Full bladder
Full rectum
Hypoxia
Pain/discomfort
Fear/anxiety
Alcohol withdrawal
Sedation for terminal agitation or distress should be prompt. Consider moving the patient to a visible area or
do not leave unattended for those at risk of harm to themselves or others. Do not use opioids to treat
agitation.
Agitation and restlessness
Midazolam 2.5 - 10 mg SC stat
Midazolam 10 – 120 mg over 24 hours via continuous subcutaneous infusion.
If fear is the only feature for minimal sedation use lorazepam 0.5 - 1mg sublingually or orally.
Agitation, psychosis and hallucinations
Levemepromazine 12.5-25 mg stat dose SC and 12.5-150 mg over 24 hours via continuous subcutaneous
infusion. Titrate dose according to response, usual max dose 300 mgs over 24 hours.
Haloperidol 2.5-5mg stat dose by SC injection or 5-20 mg over 24 hours via continuous subcutaneous infusion
WOUND CARE
Cancer and cancer treatments produce physiological changes, which can cause problems in wound healing.
Each malignant ulcer requires individual assessment.
Healing may be possible, but comfort is the primary aim.
Aetiology
Fungating malignant wounds results from infiltration of the skin and it's supporting blood and lymph vessels.
The tumours may be locally advanced, metastatic or recurrent. There is the potential for massive damage to
the skin through a combination of proliferate growth, loss of vascularity and ulceration.
As the tumour enlarges it causes the capillaries to rupture or become occluded, resulting in necrosis of the
skin and the formation of a cutaneous wound.
Assessment and Evaluation
Assessment, documentation and evaluation are key components of the clinical role in any aspect of patient
care. A thorough assessment ensuring that the plan of care is appropriate for each individual patient.
There are many factors to consider when managing the patient with a complex wound. Much depends on the
position of the wound, the size, whether it is malodorous or painful, bleeding or infected and the general
condition of the patient.
Assessment
Relevant history
Cause and stage of the disease
Present treatment
Physical limitations
Nutritional status
Emotional considerations
Self perception
Patient/carer/families knowledge of diagnosis
Family carer influences
Environmental influences
Support systems available
Local wound surface and associated symptoms.
Management Aims
To promote comfort
Improve the quality of life
Control the symptoms
As with any wound the underlying cause of the wound, the tumour in this instance, needs to be diagnosed and
treated. Symptom control measures, both local and systemic, together with wound dressings are the
mainstays of management once curative treatment has been exhausted.
The priorities for dressing choice should be:
Patient comfort and acceptability
Minimising slough and necrotic tissue
Minimising infection
Containing odour
Containing exudate
Dressing choice
Rationale
Hydrocolloid
Absorb low/medium exudate
Semi-permeable film Foam Silicone NA Alginate Absorb
Hydrofibre Foam Calcium alginate dressings
Haemostatic properties
Topical metronidozole
Deodorising properties
Dressings containing activated Charcoal Topical metronidozole
Antibacterial/antiseptic properties
Iodine based products Fungating wounds usually present with multiple symptoms: Slough/Necrosis Infection Exudate Malodour Bleeding
Pain (at wound site)
Itching/Irritation
Decision Tree for Appropriate Use of Antimicrobial Products
Complete holistic wound assessment
Record wound aetiology
Record level of exudate
Record tissue types present at
wound bed (express as a %)
Is there evidence of clinical
Follow protocol for
wound infection?
Consider systemic
• Localised heat
antibiotics as a first line
Localised swelling
Increased exudate
Excessive bleeding
Special instructions:
If patient has a:
Diabetic Foot Ulcer
Atypical colour of exudate
General malaise of the
Consider use of topical
antimicrobials in conjunction
with systemic antibiotics.
Review after 2 weeks
Consider use of topical
Is wound critically colonised?
Sudden/unexplained
increase in pain
Review after 2 weeks
Thick slough not
responding to treatment
Reassess current treatment regime
Appropriate level of
No cellulitis present
compression therapy?
Appropriate pressure relief?
Appropriate wound
Slough/Necrosis
Slough and necrotic tissue is essentially dead tissue that provides an environment in which anaerobic infection
thrives with resulting malodour and exudates.
The purpose of removing slough and/or necrotic tissue is to lessen the risk of infection occurring.
Methods of debridement are limited in the management of fungating wounds.
Surgical or sharp debridement is not generally an option because of problems associated with bleeding.
Enzymatic debridement is not recommended as fungating wound are often associated with bleeding and
there is a risk of absorption.
Autolytic debridement is more acceptable and less invasive. The principle is to provide a moist environment
by using a product that can donate fluid and absorb excess fluid, promoting autolysis (destruction of tissue)of
slough/necrotic tissue.
Patients with extensive wounds covered in eschar may not benefit from debridement if life expectancy is short
and the consequent exudate is profuse.
Infection
Due to the chronic nature of fungating wounds, a sudden increase in the patient's wound symptoms may be
the first indication of wound infection.
A wound swab will confirm the presence of infection in the wound. Systemic antibiotics may be used in
treating the infection, however, the blood supply to fungating wounds is often poor and the concentration of
antibiotic at the wound site may not be sufficient to have any effect. Topical metronidazole may have a role of
anaerobic infection is suspected or confirmed.
Exudate
Exudate is probably the most common problem associated with fungating wounds. Without control of exudate
interrelated problems such as leakage and soiling, peri-wound maceration and odour will not be managed.
Dressings used to contain exudate should have minimal bulk, whilst preventing leakage and creating an
acceptable cosmetic effect.
Protection of the surrounding skin is also of vital importance to prevent breakdown and enlargement of the
wound. Excessive amounts of exudate produced by these wounds will lead to maceration and excoriation.
Therefore dressings that absorb and contain exudate will prevent skin damage.
Stoma products can be used to protect surrounding skin such as a filler paste which can level out creases in
the surrounding tissue and help to maintain a good seal around the wound. When the exudate is excessive a
stoma bag may be more appropriate.
An alcohol-free barrier product, such as Cavilon, has been shown to assist healing of macerated skin, with a
reduction of unpleasant symptoms. Cavilon forms a sustained barrier against the effects of fluids on the skin.
Silver dressings are impregnated with slow-release silver. They are for use on wounds where critical
colonization is suspected and should not be used routinely on clinically infected wounds which will require
systemic antibiotics. They are effective against most micro-organisms. These dressings are very expensive
and prone to inappropriate usage. Prescribe dressings for 2 weeks only and review effectiveness. If no
improvement is evident, discontinue.
Malodour
There are three main approaches adopted for the management of odour.
Systemic antibiotic
Topical antibiotic
Charcoal dressings.
Systemic antibiotic
Metronidozole kills anaerobic bacteria responsible for odour production. However, treatment may cause side
effects such as nausea, alcohol intolerance and neuropathy.
Topical antibiotic
Is recommended as an alternative to systemic antibiotic. Metronidozole gel can be mixed with a hydrogel, in
equal quantities, to combine the properties of odour and slough management. A wound swab to confirm
infection is useful.
Charcoal dressings
Activated charcoal dressings can be used in conjunction with Metronidozole gel. They are used as a
secondary dressing as contact with moisture renders them ineffective.
Dressings that contain a layer of activated charcoal as well as an absorbent primary wound contact layer are
also available (e.g. Carboflex, Lyofoam C).
Bleeding
Bleeding in fungating wounds can be related to tumour activity or due to the application of inappropriate
dressings.
Attention to dressing application and removal techniques, maintenance of humidity at the wound/dressing
interface, cleaning techniques and the use of non-fibrous material can reduce the incidence of bleeding at
dressing changes.
Alginate dressings, which are considered to be haemostatic, can be applied to bleeding areas. To prevent the
dressing from drying onto the wound it may be moistened with 0.9% sodium chloride solution before
application. The wound should be irrigated with warmed saline prior to removal of the dressing to reduce the
risk of trauma.
Adrenaline 1:1000 can be applied topically, as an emergency measure. This must not be used liberally as it
can cause ischaemic necrosis.
PAIN
The assessment of pain from the wound site should be managed separately from any other pain that the
patient is experiencing.
Pain that occurs during dressing changes may be due to adherence of dressing. Thorough irrigation to soak
the dressing may ease removal; a review of dressing choice may be necessary.
It is important to distinguish between pain caused by the stimulation of nerve endings (nociceptive pain) and
pain caused by nerve dysfunction (neuropathic pain) because different treatments may be indicated.
Local anaesthetic for example lignocaine gel can be applied directly to the wound surface.
Short acting strong opioids at dressing changes can be used to optimise comfort.
Topical opiates can be used to palliate nociceptive pain and stinging from damaged and ulcerated skin.
Diamorphine 10mg or morphine sulphate 10mg can be mixed with a hydrogel 10ml and applied directly to the
wound surface.
Non-steroidal anti-inflammatory drugs (NSAID's) can be useful if pain is associated with local inflammation.
Pain due to maceration and excoriation may be reduced by the use of a non-alcoholic skin barrier such as
Cavilon.
Subject Specific References
Bale S. A Guide to Wound Debridement. Journal of Wound Care 1997; 6(4): 179-182.
Bennett GM and Moody M. Wound Care for Health Professionals. London: Chapman and Hall, 1995
The Care of Wounds. 2nd Edn. Oxford: Blackwell Science, 1999.
Gilchrist B. Wound Infection. In. Wound Management Theory and Practice. London: Nursing Times Books, 1999: 96-106.
Grocott P. The Management of Fungating Wounds. Journal of Wound Care 1999; 85: 232-234
Grocott P. The Palliative Management of Fungating Malignant Wounds.
Wound Care Society Educational Booklet, 2001; 8 (2)
Hallet A. Fungating Wounds. Wound Care Society Educational Leaflet, 1993; 12
Moody M, P Grocott. Let us extend our knowledge base, assessment and management of fungating
malignant wounds. Professional Nurse, 1993; June: 586-590.
Naylor W, Laverty D, Mallett J. The Royal Marsden Hospital Handbook of Wound Management in Cancer Care. London: Blackwell Science, 2001. SMTL . Dressing Data Cards (on line) Htlp:www.smtl.co.uk, 1999.
Thomas S. A structured approach to the selection of dressings. World Wide Wounds (online)
Care Pathway for the Management of Oedema
Exclude venous thrombosis and vena caval obstruction by tumour – treat
Is venous obstruction
appropriately.
Implement skincare, refer to Lymphoedema Service if oedema persists.
Antibiotics, if erysipelas suspected start Penecillin v or erythromycin. Nb, titrate dose to the size of the patient. Use prophylactic dose if recurrent
Is infection present?
infections occur. Implement, skincare, exercise, when infection resolved fit
with low compression garment e.g. 10 – 20 mmHg. Refer to Lymphoedema
Service.
Wash, dry thoroughly, moisturise. Apply appropriate dressing. Encourage exercise and fit with low compression hosiery over dressing if possible. Refer
Is the skin broken?
to Lymphoedema Service. If lymphorrhoea present *
If appropriate refer to Vascular consultant, organise doppler investigation. If
Is arterial insufficiency
>0.8 consider low compression <0.7 avoid compression. Implement skincare,
refer to Lymphoedema Service.
e.g. poor venous return, cardiac insufficiency, low albumin
Is this a low protein
Implement skincare, exercise, low compression garment,
diuretic therapy as appropriate.
Implement skincare, gentle or passive exercise, positioning, low compression
Is prognosis poor ?
garment, palliative lymphoedema bandaging (PLB) see below . NB analgesia. If fungating lesion present see below
Is oedema limited to head,
Implement skincare, exercise, refer to Lymphoedema Service.
neck, trunk or genitalia?
For penile swelling try large size conveen and for scrotal oedema try double layer tubifast.
Implement skincare, exercise medium compression e.g. 20- 30 mmHg and
refer to Lymphoedema Service.
Is this an upper limb swelling or true
* If lymphorrhoea present: Wash, dry thoroughly, moisturise with emollient eg Eucerin 3%. Apply hydrocolloid modified
If fungation and lymphorrhoea present: Consider
carmellose dressing eg Aquacel, absorbent pads and PLB I.e.
metronidazole gel and/ or charcoal dressings then if unable
Under cast wadding e.g. Velband, from toe to above knee then
to apply PLB, sanitary towels can be used to the axilla or
short stretch bandages e.g. Comprilan from toe to above knee.
groin to lock lymph away therefore maintaining the healthy
Nb FOR SUPPORT NOT COMPRESSION
When leakage stopped fit with low compression hosiery
LYMPHOEDEMA
1
Refer to South Essex Lymphoedema Services (S.E.L.S.) (Note patients will be seen locally after initial consultation)
Advise patients to wash and moisturise the affected limb(s) daily and to carry out muscle pumping exercises.
Diuretics can be effective.
Steroids can be useful if the affected limb is tumour obstructed.
Patients should follow preventative advice for infection. If signs of Acute Inflammatory Episode (AIE) occur, treat with antibiotics as appropriate. For recurrent AIE's prophylactic penicillin can be introduced.
For Lymphorrhoea – wash limb(s)
Moisturise Apply hydrocolloid dressing e.g. Aquacel or Cutinova Cavity then absorbent pads Refer to S.E.L.S
Subject Specific Reference
Mortimer P, Shankar S, and Marshall K. Skincare in Lymphoedema. British Lymphology Newsletter, 2000;
28: 5-8.
GENERAL REFERENCES AND FURTHER READING
The Association of Palliative Medicine and The Pain Society. The Use of Drugs Beyond Licence in Palliative Care and Pain Management. Southampton and London: The Association of Palliative Medicine and The Pain Society, 2002 Back I N. Palliative Medicine Handbook. Third Edition. Cardiff: BPM Books, 2001
Swinburne. R et al (eds) Oxford Textbook of Palliative Medicine. Fourth revised Edition. Oxford: Oxford University Press, 2009.
Fallon M and O'Neill W (eds). ABC of Palliative Care. London: BMA Books, 1998
Reynard C & Tempest. A Guide to Symptom Relief in Advanced Disease. England: Hochland and Hochland, 1998. Twycross R. Symptom Management in Advanced Cancer. Fourth Edition. Oxford: Radcliffe Medical Press, 2001. Twycross R et al. Palliative Care Formulary. Third Edition. Abingdon: Radcliffe Medical Press, 2007.
Source: http://www.essexcancernetwork.nhs.uk/pages/members/clinical-groups/Supportive-Palliative-and-End-of-Life/PALLIATIVE%20CARE%20FORMULARY%202010%201.pdf
Nazionale Padova, 10 -11 Ottobre 2013 Aula Magna, Palazzo del Bo Università degli Studi di Padova Corso Interattivo Il percorso della MEDICINA di GENERE nel Sistema DIABETE Padova, 12 Ottobre 2013 Aula Nievo, Palazzo del Bo Università degli Studi di Padova Il CUG e la Medicina di Genere
(El Medicamento Homeopático y su Teoría de aplicación) Material que recibe: CD-ROM con Curso completo, y CD´s que incluyen dos software de Homeopatía Francesa de regalo (en español), artículos formativos para la clínica homeopática y documentos de texto de Materia Médica Homeopática (4500 páginas) herramienta útil de consulta para facilitar la búsqueda del