Froum.qxd
Froum.qxd 1/23/06 10:57 AM Page 71
A Retrospective Study of 1,925 Consecutively Placed
Immediate Implants From 1988 to 2004
Barry Wagenberg, DMD1/Stuart J. Froum, DDS2
Purpose: The purpose of the present study was to evaluate implant survival rates with immediateimplant placement (IIP) into fresh extraction sockets and to determine risk factors for implant failure.
Materials and Methods: A retrospective chart review was conducted of all patients in whom IIP wasperformed between January 1988 and December 31, 2004. Treatment required atraumatic toothextraction, IIP, and mineralized freeze-dried bone allograft with an absorbable barrier to cover exposedimplant threads. Implant failure was documented along with time of failure, age, gender, medical his-tory, medications taken, postsurgical antibiotic usage, site of implant placement, and reason forimplant failure. Statistical analysis was performed using chi-square and logistic regression analysismethods. Results: A total of 1,925 IIPs (1,398 machined-surface and 527 rough-surface implants)occurred in 891 patients. Seventy-one implants failed to achieve integration; a total of 77 implantswere lost in 68 patients. The overall implant survival rate was 96.0% with a failure rate of 3.7% pre-restoration and 0.3% postrestoration. Machined-surface implants were twice as likely to fail as rough-surface implants (4.6% versus 2.3%). Men were 1.65 times more likely to experience implant failure.
Implants placed in sites where teeth were removed for periodontal reasons were 2.3 times more likelyto fail than implants placed in other sites. Patients unable to utilize postsurgical amoxicillin were 3.34times as likely to experience implant failure as patients who received amoxicillin. Conclusions: With a1- to 16-year survival rate of 96%, IIP following tooth extraction may be considered to be a predictableprocedure. Factors such as the ability to use postsurgical amoxicillin and reason for tooth extractionshould be considered when treatment planning for IIP. INT J ORAL MAXILLOFAC IMPLANTS 2006;21:71–80
Key words:
age factors, dental implants, gender, implant surfaces, implant survival, penicillin allergy,smoking
Ahigh level of predictability for implants placed rates of 99.1% in the mandible and 84.9% in the
into fully and partially edentulous patients has
maxilla.2 Unfortunately, during this extended postex-
been demonstrated in many long-term studies.1–9
traction healing phase, resorption of the residual
The procedure used in most of these studies includes
bone occurs.
a 6- to 12-month healing period following tooth
Studies have demonstrated that approximately
extraction to allow implant placement into mature
45% of the residual alveolar ridge may be resorbed
bone.1,10 Albrektsson and associates stated that this
after tooth extraction, with the majority of resorption
protocol resulted in 5- to 8-year implant success
occurring during the first 6 months after extrac-tion.11,12 Without treatment, resorption is observed inall dimensions of the residual alveolar ridge follow-ing tooth extraction.13–15 Left uncontrolled, this
1Director of Dental Education, Newark Beth Israel Hospital,
resorption could prevent routine implant placement.
Newark, New Jersey; Associate Clinical Professor, Department of
Immediate implant placement (IIP) into an extrac-
Periodontology and Implant Dentistry, New York University, New
tion socket has been proposed as a method to pre-
York, New York.
2Clinical Professor and Director of Clinical Research, Department
serve bone at the surgical site.16–18 Other advantages
of Periodontology and Implant Dentistry, New York University
of IIP are a reduction in treatment time and the ability
Dental Center, New York, New York.
to place the implants in positions that are favorable forthe final prosthesis.19 In addition, patient acceptance
Correspondence to: Dr Stuart J. Froum, 17 West 54th Street,
from the reduced number of surgeries and reduced
Suite 1C/D, New York, NY 10019. Fax: +212 586 7599. E-mail:
[email protected]
treatment time is an advantage of this method.20
The International Journal of Oral & Maxillofacial Implants
COPYRIGHT 2005 BY QUINTESSENCE PUBLISHING CO, INC.
PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY.
NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM
WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER.
Froum.qxd 1/23/06 10:57 AM Page 72
Two literature reviews found similar implant sur-
1. Apical or lateral stabilization. Upon surgical place-
vival rates for immediate and delayed implant place-
ment, the implants achieved stability in host
ment. 19,21 Likewise, bone fill occurred with sub-
bone. Dehiscence with thread exposure at the
merged and nonsubmerged implant placement.22
time of implant placement did not prevent inclu-
Studies describe a variety of techniques resulting in
sion in the study if initial stability was obtained.
survival rates of immediate implants ranging from
2. Lack of residual infection. The extraction socket
89% (for molar replacement only) to 100%, with
was examined after a thorough curettage remov-
study durations ranging from 1 to 11 years.23–33
ing all residual fibers from the apical area and the
Comparison of success rates and analysis of the
lateral walls.
factors important for implant survival is difficult with
3. Continuous function for a period of 1 year
the many variables included in the aforementioned
postrestoration. If an implant failed prior to
studies (ie, implant surface, use of bone graft and/or
restoration placement this implant was included
membrane barrier, primary closure of wound, reason
in the statistical analysis and considered as a fail-
for tooth extraction). In the present retrospective
ure prior to final restoration.
study, protocol variation was controlled; the sametechniques (bone grafting and membrane use) were
A consistent surgical protocol was followed. Local
utilized for placement of all implants. The purpose of
anesthesia was achieved through infiltration tech-
the present study was to evaluate survival rates of
niques (no regional block anesthesia) using lidocaine
implants placed immediately into fresh extraction
with 1:50,000 epinephrine (Abbott Laboratories)
sockets and restored for a minimum of 1 year. An
unless medically contraindicated. In patients where
additional purpose was to correlate implant failure
epinephrine was contraindicated, mepivacaine 3%
rates with the age and gender of the patients,
(Abbott Laboratories, North Chicago, IL) was used.
implant position, smoking habits, medications taken,
Full-thickness flaps were elevated with minimal
penicillin allergy, and reason for tooth failure.
palatal elevation in the maxilla. Vertical incisions wereutilized as necessary. The teeth to be removed wereextracted atraumatically whenever possible. Molars
MATERIALS AND METHODS
were sectioned and roots removed separately. Usinga bur, a trough was made around the circumference
A retrospective chart review was conducted on all
of the root through the ligament. The roots were
patients treated with implants placed immediately
removed with an elevator using minimum pressure.
into tooth extraction sites by a single periodontist.
Sockets were thoroughly degranulated with curettes
Patients were identified through analysis of the
or burs and inspected. All remnants of fibers and soft
office database and through evaluation of data
tissue were removed from the sockets.
recorded in an implant tracking software program
Standard protocol and the manufacturer's recom-
(Implant Tracker, West Hartford, CT). Once patients
mendations were followed for drilling. Implant place-
were identified, individual charts and radiographs
ment varied by area and position of the remaining
were evaluated, and the following data were
bone. Implants in the esthetic zone were placed
recorded: age at implant placement, date of implant
slightly to the palatal, especially between the maxil-
placement, gender, medical history, smoking history,
lary right and left canines. Implants in the premolar
medication usage, medical allergies, reasons for ini-
area in the maxilla were placed to the palatal, but api-
tial tooth failure, location of implant placement, addi-
cally, through the remaining septum. In the mandibu-
tional surgical procedures (eg, sinus lift), implant
lar premolar area implants were placed into the cen-
dimensions, implant manufacturer, date of abutment
ter of the socket. In the maxillary and mandibular
connection, date of final restoration seating, and,
molar areas implants were placed slightly to the
when applicable, date of and reasons for implant fail-
mesial of the interradicular bone (most often utilizing
ure. Restorative clinicians were contacted via tele-
a wide implant, but not necessarily in contact with the
phone survey to confirm the dates of restoration and
buccal and lingual plates of bone). When sinus lifts
determine whether there were any unreported com-
were performed, either lateral windows were opened
plications or failures of the immediately placed
or osteotomes were utilized to complete the implant
implants. Up-to-date monitoring with recall visits to
preparation. An appropriate-length implant was
the surgeon and restorative clinicians was performed
placed, leaving the platform 1 to 2 mm apical to the
for all patients and all implants placed through
most coronal height of the remaining crest.
December 2004.
Mineralized freeze dried bone allograft (FDBA)
Implants included in this review met the following
(Miami Tissue Bank, University of Miami; Miami, FL)
inclusion criteria:
was tightly packed into the residual spaces around
Volume 21, Number 1, 2006
COPYRIGHT 2005 BY QUINTESSENCE PUBLISHING CO, INC.
PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY.
NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM
WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER.
Froum.qxd 1/23/06 10:57 AM Page 73
the implant. A periodontal probe was utilized to
Göteborg, Sweden, and Implant Innovations/3i, Palm
push the bone into narrow spaces. Bone grafts were
Beach Gardens, FL). The mean patient age at the time
utilized in all cases in which there was a residual
of surgery was 57.9 years, with a range of 14 to 94
space around the implant. A Vicr yl membrane
years. A total of 1,925 implants were placed in fresh
(Ethicon/Johnson & Johnson, Somerville, NJ) was cus-
extraction sockets immediately following tooth
tom cut, extended 5 to 7 mm beyond the margins of
extraction. As of December 31, 2004, a total of 1,854
the defects and tucked under the flaps both labially
implants had been restored for at least 1 year. A total
and palatally (lingually) without suturing. The flaps
of 1,398 machined-surface and 527 rough-surface
were closed using chromic 4-0 gut sutures. No
implants were placed. Thir teen implants in 10
attempt was made to advance the flaps and cover
patients were placed in conjunction with lateral-win-
the membrane (Figs 1a to 1g). Patients were premed-
dow sinus lifts, and 148 implants in 111 patients were
icated with amoxicillin (500 mg 4 times daily; TEVA
placed using an osteotome internal sinus augmenta-
Pharmaceuticals USA, Sellersville, PA) starting 2 days
tion procedure. Nineteen implants in 7 patients were
prior to the procedure and continuing for 10 days
immediately loaded following placement. Forty-five
postsurgery. Penicillin-sensitive patients were pre-
implants in 40 patients received immediate nonoc-
medicated with clindamycin (300 mg 4 times daily;
clusally loaded provisional restorations following
Watson Laboratories, Corona, CA) prior to surgery
placement. The follow-up period varied between 12
and continuing for 10 days. The patients utilized
and 193 months after delivery of the final prosthesis,
.12% chlorhexidine gluconate (Peridex, Vila Pharma-
with a mean follow-up period of 71 months. Failure
ceutical, Phoenix, AZ) on a cotton tip to lightly clean
to achieve or maintain osseointegration was seen in
any exposed membrane area 3 times daily until the
68 patients, some of whom experienced more than 1
membrane was absorbed.
failure. A total of 77 implants were lost (42 in male
Most implants were allowed to heal for 3 months
patients; 35 in female patients). Of these failed
in the mandible and 6 months in the maxilla prior to
implants, 71 (92%) failed to achieve osseointegration
second-stage surgery. In most cases final restoration
and 6 (8%) failed to meet success criteria after final
began within 3 weeks of second-stage surgery. Of
restorations were placed.34 Nine patients experi-
the implants that were immediately restored with
enced multiple failures—1 patient lost 2 implants to
provisional restorations, the same IIP protocol was
progressive bone loss, 3 patients lost 2 implants each
followed as to position of placement, use of graft and
to nonintegration, 4 patients lost 2 implants each to
membrane, and flap closure.
infection, and in 1 patient, 2 implants were removed
Implant failure was recorded as "before final
because of paresthesia. The reasons for implant fail-
restoration" or "after final restoration." Whenever pos-
ure as well as the reasons for the tooth loss that pre-
sible the reason for implant failure was recorded.
cipitated the need for implant placement were docu-
Implant survival was checked at the abutment con-
mented (Table 1). The overall implant survival rate
nection stage and at various intervals after place-
was 96.0%, with implant failure rates of 3.7% prior to
ment of the final restoration. Implant survival was
restoration and 0.3% after restoration (Table 2).
defined by the criteria proposed by Albrektsson and
Of the 1,398 machined-surface implants placed,
65 failed (4.6%). Of the 527 rough-surface implants
Data analysis methods included chi-square analy-
placed, 12 failed (2.3%). There was a statistically sig-
sis for the evaluation of statistical significance and
nificant difference in implant failure rate between
logistic regression analysis for the evaluation of
rough- and smooth-surface implants (
P = .02). A total
impact of demographic and clinical variables on
of 1,602 implants were placed in nonsmokers, 1,162
implant survival. Data analysis software used was
with machined surfaces and 440 with rough sur-
JMP 5.0.1.2 (SAS Institute, Cary, NC). The level (alpha)
faces. A statistically significant difference between
of statistical significance was .05.
the failure rates of smooth- and rough-surface (4.5%versus 1.8%) implants was documented (
P = .01) innonsmokers.
A total number of 323 implants were placed in
patients with a self-described smoking habit. Of these,
Eight hundred ninety-one consecutively treated
18 failed (5.6%). Nonsmokers received a total of 1,602
patients (381 men and 510 women) in whom imme-
implants of which 59 (3.7%) failed. The difference in
diate implant surgery was performed between Janu-
implant failure rate between smokers and nonsmok-
ary 1988 and December 31, 2004 were evaluated
ers was not statistically significant (
P = .342). There
through the study. All patients were treated with
was no difference in the failure rate of rough-surface
implants made by 2 manufacturers (Nobel Biocare,
implants and that of smooth-surface implants in
The International Journal of Oral & Maxillofacial Implants
COPYRIGHT 2005 BY QUINTESSENCE PUBLISHING CO, INC.
PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY.
NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM
WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER.
Froum.qxd 1/23/06 10:57 AM Page 74
smokers (
P = .6492). Fifty-one immediate implants
Reasons for Tooth and Implant Loss
were utilized to replace failed implants. Two of these
failed, for a 3.9% failure rate, which was not signifi-
cantly different than the failure rate in the general sur-
vey population (
P > .05).
Of the 1,094 implants placed in women, 34 failed
for a 3.1% failure rate. Forty-three of the 831 implants
placed in men failed, for a 5.2% failure rate. The rela-
tive risk of implant failure in men was 1.65 times that
for women (
P = .0314, CI [1.04, 2.61]).
Two of 51 immediate implants placed to replace a
failing implant failed, for a failure rate of 3.92%.
The mean age of women in this study was 57
years. The mean age of men was 59 years. This repre-
sents a statistically significant difference in age in the
study population (
P < .001) No correlation was found
between implant failure and age of the patient
(
P > .06).
There was no statistically significant correlation
between implant failure and any single medication
or combination of medications taken by patients in
this study in whom implant failure occurred (
P =
.895). A significantly greater implant failure rate was
linked to the high infection rate in patients who were
unable to use postsurgical penicillin due to allergy,
with penicillin-allergic patients demonstrating a rela-
tive risk of 3.3 when compared to patients who were
able to utilize penicillin (
P < .01). Patients with an
allergy to penicillin were 5.7 times more likely to
experience implant failures due to infection than
patients without allergy to penicillin (Table 3). There
was no significant difference in implant failure rate
associated with any medical condition of patients
included in this study (
P = .967).
A total of 383 implants were used to support sin-
gle crowns. The remaining 1,471 implants were used
Failure Rate of Implants Before and After
Total implants placed
Total implants failed
Postrestoration failures
Failures prerestoration
Table 1 notes: Universal (FDI) tooth numbers shown. AB-PD = abscess periodontal
disease; AB-PDD = periodontal abscess; ATI = adjacent tooth infection; D = distal;
DEC = decay; FBG = failed block graft; I = infection; IL = immediate load; ISL =
internal sinus lift; ITR = immediate tooth replacement; M = mesial; NI = noninte-
PBL-VHS gration; O-O = occlusal overload; P = parasthesia; PAP = periapical pathology; PBL
PBL-VHS = progressive bone loss; PDD = periodontal disease; RAB = refused antibiotic; RF
= root fracture; TEP = trauma–epileptic patient; TLC = trauma from a loose crown;
VHS = very heavy smoker; WSL = window sinus lift.
*After 9 y.
†After 5 y.
Volume 21, Number 1, 2006
COPYRIGHT 2005 BY QUINTESSENCE PUBLISHING CO, INC.
PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY.
NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM
WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER.
Froum.qxd 1/23/06 10:57 AM Page 75
in restorations supported by multiple implants, with
Implant Failure in Patients with Penicillin
2 or more implants splinted to support the definitive
prosthesis. There were no failures in the single-unit
Number placed Number failed
group, while 16 implant failures were seen in thesplinted group. This difference was not significant
No penicillin allergy
(
P = .356).
Penicillin allergy
A significant difference in implant failure rate by
area of implant placement was seen (
P = .001) (Table4). The area with the highest percentage of failureswas the mandibular anterior area, while the lowestpercentage of failure occurred in the maxillary
Implant Failure by Location
canine area.
One hundred twenty-two teeth were lost because
of periodontal disease, while 1,803 teeth were lost
for other reasons. The difference in implant failure
between implants placed at the sites of periodon-
tally diseased teeth and those placed in nondiseased
sites was statistically significant (
P = .02). Implants
placed after tooth extraction because of periodontal
causes were 2.3 times more likely to fail than
implants placed after tooth extraction for nonperio-
dontal reasons (Table 5).
The 96.0% survival rate of the 1,925 implants placed
Implant Failure and Etiology of Tooth
in the present study is similar to reports for implants
placed in healed bone.35 This study reports on
restorations that were in place at least 1 year post-
loading, with a follow-up from 1 to 16 years, whichalso compares favorably with the time of follow-up
in other studies. Using 2 electronic databases and
having 1 individual enter all of the data minimizedthe possibility of undetected failures.
The current study demonstrates a statistically sig-
shown that rough-surface implants can partially com-
nificant difference in favor of rough surface implants,
pensate for the negative healing response in
but both surfaces demonstrated survival rates in
smokers,46–48 the current study demonstrated no sig-
excess of 95%. When considering implant placement
nificant difference in implant failure in smokers,
in healed bone, no significant differences were seen
regardless of the type of implant surface. A number of
relative to implant surface.36 With the reported
factors may explain this lack of difference in implant
advantage of roughened surfaces being improved
failure rate in smokers compared to nonsmokers. In
clot formation and increased bone-to-implant con-
the present study, patients were categorized as smok-
tact,37 it is possible that these factors play a role in IIP.
ers if they reported smoking more than 10 cigarettes
In addition, during the early phases of IIP, only
per day. There was no calculation made of how many
machine-surfaced implants were used; consequently,
of these patients smoked no more than 10 cigarettes.
a "learning curve" may have influenced implant fail-
This may be an important issue, as the findings of a
ure in that study group.
meta-analysis indicated that "light smoking" (average
Although some studies have reported decreased
of 12 cigarettes per day) did not affect the success
implant survival in smokers,38–45 only 1 immediate
rate of either machined or dual-acid-etched surface
implant study reported the effect of smoking and
implants.47 In the current study, absorbable mem-
implant survival.46 In contrast to other reports, the
branes were placed over FDBA and were often left
results in the present study show no significant differ-
exposed. Although smoking has been reported to
ence in implant failure rate between smokers and
have a detrimental effect on periodontal regenerative
nonsmokers. Likewise, while some studies have
procedures utilizing bioresorbable barriers in cases of
The International Journal of Oral & Maxillofacial Implants
COPYRIGHT 2005 BY QUINTESSENCE PUBLISHING CO, INC.
PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY.
NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM
WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER.




Froum.qxd 1/23/06 10:57 AM Page 76
Radiograph of maxillary left lateral incisor with a large periapical area.
Clinical photograph following extraction, debridement of the socket, and placement of the immediate implant.
Placement of mineralized FDBA to fill the defect.
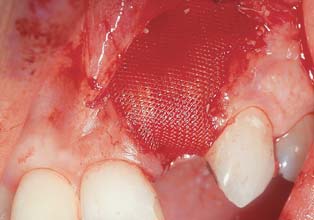
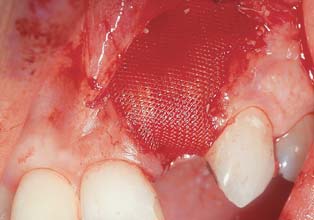
Placement of an absorbable membrane barrier over the graft and implant.
Closure with absorbable sutures.
Radiograph of the implant 5 years postloading.
Clinical photograph of the implant restoration 5 years postloading.
molar furcations, the healing process may differ fol-
Gender was seen as a significant risk factor for
lowing immediate implant placement as performed
implant failure (P = .0207) as the relative risk for fail-
in the present study.49 Oral hygiene in the current
ure in men showed a 5.05% failure rate compared to
study included localized applications of chlorhexidine
a 3.2% failure rate of IIP in women. The results of the
3 times a day until the membrane was absorbed. This
present study are in agreement with a previously
combined with the use of systemic antibiotics may
published report by Schwartz-Arad and coworkers28
have prevented the negative impact of bacterial colo-
of increased failure rate for IIP in men compared to
nization in the healing site. The fact that all patients
women, although that study evaluated a small num-
included in this study were treated for their periodon-
ber of implants and showed a much higher overall
tal disease prior to or in conjunction with their
failure rate than the current article.
implant treatment would present a population with a
The findings that there was no significant differ-
reduced risk for bacterial contamination from ongo-
ence in failure rate associated with any single med-
ing disease. The results of the present study are in
ication or combination of medications taken by
agreement with previous findings that rate of implant
patients who received IIP and that no medical condi-
failure was not correlated with age.50,51
tion was associated with a statistically significant dif-
Volume 21, Number 1, 2006
COPYRIGHT 2005 BY QUINTESSENCE PUBLISHING CO, INC.
PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY.
NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM
WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER.
Froum.qxd 1/23/06 10:57 AM Page 77
ference in implant failure are of interest. Some have
other failures occurred because of implants that were
questioned the effect of osteoporosis and medica-
immediately restored with nonoccluding provisional
tions used to treat osteoporosis on implant sur-
vival.52–55 The present study demonstrated no differ-
Ten of the 13 implant failures that occurred in the
ence in immediate implant survival related to the
maxillary molar area were due to nonintegration.
taking of bisphosphonates or a reported condition of
Nine of these were placed into bone augmented
osteoporosis. In fact, only 2 of the 75 implants placed
with 2 lateral window and 7 internal sinus lift proce-
patients with a history of osteoporosis failed (n = 34).
dures. In a study by Schwartz-Arad and colleagues27
The 24 patients that were taking Fosamax (Merck,
the cumulative survival rate (CSR) of all implants in
West Point, PA) experienced no implant failures.
the study was 92%. The 5-year CSR was 90% in all
An important part of the technique used in the
areas of the maxilla but only 72% in the posterior
present study was the use of a bioabsorbable mem-
maxilla.27 In the present study the high survival rate
brane barrier over which no attempt was made to
of immediately placed implants in the maxillary
achieve primary closure. The use of penicillin as a
anterior area may have been related to the easier
postsurgical antibiotic with these bioabsorbable bar-
access in this area for bone graft and membrane
riers may have decreased bacterial colonization, thus
placement, along with more effective oral hygiene
reducing infection postsurgery. There was a signifi-
for the patient.
cant relationship between implant failure caused by
Several studies have documented high survival
infection and an inability to use postsurgical peni-
rates for conventionally placed implants in patients
cillin (P < .001). Dahlin56 reported better membrane
with different types of periodontal disease.60–62 In the
tolerance and less infection in patients able to take
present study implants replacing teeth that were
penicillin as opposed to 1 patient that had to be
extracted for periodontal reasons were 2.3 times
placed on erythromycin. All patients in the present
more likely to fail than implants replacing teeth
study who described no penicillin allergy were pre-
extracted for nonperiodontal reasons. These results
scribed amoxicillin starting 2 days prior to the proce-
are in agreement with a previous study and demon-
dure, and continued on the antibiotic for 10 days
strate significantly lower survival of implants when
postsurgery. Although some controversy57–59 exists
placed in sites from which periodontally involved
relative to the use of postsurgical antibiotics, the pro-
teeth were removed.63 In patients in whom teeth
tocol applied in this study used antibiotics for all
were lost for periodontal reasons, the disease may
patients following IIP. In the present study 30 implant
have decreased the available bone following tooth
failures were attributed to infection. Sixteen of the 30
extraction or resulted in the necessity to place the
patients who had implant failure due to infection
implant with a more exposed surface to achieve
were penicillin sensitive. Five additional "infection"
ideal prosthetic position. Both of these situations
failures were caused by infection of an adjacent
may have resulted in a greater implant failure rate.
tooth. Three of 5 of these patients were penicillin
This question warrants further research.
sensitive. It is doubtful that the difference in implant
The flap closure technique used in the present
success seen in penicillin-allergic patients was
study, with no attempt at primary closure, did not
caused by a biologic difference in these patients that
compromise the location of the vestibule and pre-
led to a greater implant failure rate. It is more likely
served the keratinized tissue at the site of the
that penicillin is a more effective antibiotic for
implant. However, this approach was frequently asso-
implant survival than the alternative antibiotics
ciated with membranes that were exposed to the
given to these patients.
oral environment. Although other authors describe
In the present study, a statistically significant differ-
the need for primary flap closure, a literature review
ence in failure rates was associated with placement in
concluded that survival of implants was not depen-
different locations in the maxilla and mandible. Failure
dent on primary closure.21 In the present study the
rates were lowest in the maxillary premolars, canines,
antimicrobial regimen may have avoided the
and incisors (2.81%, 2.07%, and 2.13%, respectively).
reported detrimental effects of membrane exposure.
Failure rates were highest in the mandibular incisor
Considering the high clinical sur vival rates
and maxillary molar areas (7.69% and 6.44%, respec-
observed in this and other studies, the immediately
tively). The higher failure rates in the mandibular ante-
placed implant should be considered a predictable
rior area may be related to overheating of the bone
protocol. The fact that the survival rate in the present
when long implants, 15 to 18 mm, were placed (type
study showed significant differences with regard to
1). Ten of the 14 failures occurred before 2000, when
gender, implant location, and implant surfaces
longer implants were routinely used. Nine of the 14
should be viewed in the context of clinical signifi-
failed implants were lost because of infection, and 2
cance, as survival was high even in the higher-risk
The International Journal of Oral & Maxillofacial Implants
COPYRIGHT 2005 BY QUINTESSENCE PUBLISHING CO, INC.
PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY.
NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM
WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER.
Froum.qxd 1/23/06 10:57 AM Page 78
groups. Patient selection, esthetic considerations,
and inability to use penicillin, as well as the reasonfor tooth loss, should be considered in deciding
1. Adell R, Lekholm U, Rockler B, Brånemark P-I. A 15-year study
whether or not to utilize an immediate or delayed
of osseointegrated implants in the treatment of the edentu-lous jaw. Int J Oral Surg 1981;10:387–416.
implant approach.
2. Albrektsson T, Dahl E, Enbonm I, et al. Osseointegrated oral
implants. A Swedish multicenter study of 8,139 consecutivelyinserted Nobelpharma implants. J Periodontol
3. Adell R, Ericksson B, Lekholm U, Brånemark P-I, Jemt T. A long-
term follow-up study of osseointegrated implants in the treat-
Based upon a retrospective chart review of patients
ment of the totally edentulous jaw. Int J Oral Maxillofac
receiving 1,925 endosseous implants placed on the
day of natural tooth extraction:
4. van Steenberghe D. A retrospective multicenter evaluation of
the survival rate osseointegrated implants supporting fixed
• Overall implant survival rate was 96%, with 71
partial prosthesis in the treatment of partial edentulism. JProsthet Dent 1989;61:217–222.
implants failing to achieve osseointegration and 6
5. Jemt T, Lekholm U, Tagnar A. Osseointegrated implants in the
implants failing to maintain integration.
treatment of partially edentulous patients: A preliminary
• Rough-surface implants survived at a significantly
study on 876 consecutive placed implants. Int J Oral Maxillo-
higher rate (97.7%) than did machined implants
fac Implants 1989;4:211–218.
(95.4%) (P = .02).
6. Jemt T, Lekholm U. Oral implant treatment in posterior par-
tially edentulous jaws: A five-year follow follow-up report. Int J
• There was no significant difference in implant fail-
Oral Maxillofac Implants 1993;8:635–640.
ure rate between smokers and nonsmokers
7. McGlumphy EA, Peterson LJ, Larsen PE, Jeffcoat MK. Prospec-
(P = .342).
tive of 429 hydroxyapatite-coated cylindric Omniloc implants
• Men were 1.65 times more likely to develop
placed in 121 patients. Int J Oral Maxillofac Implants
implant failures than women (P = .0314).
8. Buser D, Mericske-Stern R, Bernard JP, et al. Long-term evalua-
• Patients unable to take postsurgical penicillin
tion of non-submerged ITI implants. Part 1: 8-year life table
were 3.34 times more likely to have implant failure
analysis of a prospective multicenter study with 2359
than those who used postsurgical penicillin
implants. Clin Oral Implants Res 1997;8:161–172.
(P < .001).
9. Merickse-Stern R, Aerni D, Geering AH, Buser D. Long-term
• Implants placed after tooth extraction due to
evaluation of non-submerged hollow cylinder implants. Clini-cal and radiographic results. Clin Oral Implants Res
periodontal disease were 2.3 times more likely to
experience failure than implants placed after
10. Brånemark P-I, Zarb G, Albrektsson T. Tissue-Integrated Pros-
tooth extraction unrelated to periodontal disease
theses: Osseointegration in Clinical Dentistry. Chicago: Quin-
(P < .001).
tessence, 1985.
• No significant change in implant failure rate was
11. Carlsson GE, Persson G. Morphologic changes of the mandible
after extraction and wearing of the denture. Odontol Rev
associated with any medical condition of patients
included in this study.
12. Atwood D. Post extraction changes in the adult mandible as
illustrated by microradiographs of midsagittal section andserial cephalometric roentgenograms. J Prosthet Dent
13. Lekovic V, Kenney EB, Weinlaender M, et al. A bone regenera-
tive approach to alveolar ridge maintenance following tooth
The authors would like to acknowledge the encouragement and
extraction. Report of 10 cases. J Periodontol 1997;68:563–570.
support given by Dr Steven E. Eckert in the formulation of study
14. Lekovic V, Camargo PM, Kokkevold PR, et al. Preservation of
and preparation of the manuscript. The authors would also like to
alveolar bone in extraction sockets using bioabsorbable
thank the staff members who spent countless hours checking
membranes. J Periodontol 1998;69:1044–1049.
and rechecking the database. A special thanks to the restorative
15. Iasella JM, Greenwell H, Miller RL, et al. Ridge preservation with
dentists who researched placement dates and follow-up care of
freeze-dried bone allograft and a collagen membrane com-
the patients in the study.
pared to extraction alone for implant site development: A
The authors have been involved with research on many of the
clinical and histologic study in humans. J Periodontol
materials mentioned in this review. The authors have no financial
relationships with any commercial firms that manufacture or dis-
16. Shanaman RH. The use of guided tissue regeneration to facili-
tribute these materials.
tate ideal prosthetic placement of implants. Int J PeriodonticsRestorative Dent 1992;124:256–265.
17. Denissen HW, Kalk W, Veldhuis HA, Van Wass MA. Anatomic
consideration for preventive implantation. Int J Oral Maxillo-fac Implants 1993;82:191–196.
Volume 21, Number 1, 2006
COPYRIGHT 2005 BY QUINTESSENCE PUBLISHING CO, INC.
PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY.
NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM
WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER.
Froum.qxd 1/23/06 10:57 AM Page 79
18. Watzek G, Haider R, Mensdorff-Pouilly N, Haas R. Immediate
35. Eckert SE, Choi YG, Sanchez AR, Koka S. Comparison of dental
and delayed implantation for complete restoration of the jaw
implant systems: Quality of clinical evidence and prediction of
following extraction of all residual teeth: A retrospective study
5-year survival. Int J Oral Maxillofac Implants
comparing different types of serial immediate implantation.
Int J Oral Maxillofac Implants 1995;105:561–567.
36. Esposito M, Coulthard P, Thomsen P, Worthington HV. Interven-
19. Schwartz-Arad D, Chaushu G. The ways and wherefores of
tions for replacing missing teeth: different types of dental
immediate placement of implant placement of implants into
implants. The Cochrane Database of Systematic Reviews 2005,
fresh extraction sites: A literature review. J Periodontol
Issue 1. Article no.:CD003815.pub2.
20. Rosenquist B, Grenthe B. Immediate placement of implants
37. Lazarra R, Testori T, Trisi P, Porter SS, Weinstein RL. A human his-
into extraction sockets: Implant survival. Int J Oral Maxillofac
tologic analysis of Osseotite and machined surfaces using
implants with 2 opposing surfaces. Int J Periodontics Restora-
21. Chen ST, Wilson TG Jr, Hammerle CF. Immediate or early place-
tive Dent 1999;19:117–129.
ment of implants following tooth extraction. Review of bio-
38. Bain CA, Moy PK. The association between the failure of dental
logic basis, clinical procedures and outcomes. Consensus
implants and cigarette smoking. Int J Oral Maxillofac Implants
statement. Int J Oral Maxillofac Implants
39. De Bruyn H, Collaert B. The effects of smoking on early
22. Krump JL, Barnett BG. The immediate implant. A treatment
implant failure. Clin Oral Implants Res 1994;5:260–264.
alternative. Int J Oral Maxillofac Implants 1991;6:19–23.
40. Jones JK, Triplett RG. The relationship of smoking to impaired
23. Gelb D. Immediate implant surgery: 3-year retrospective eval-
intraoral wound healing. J Oral Maxillofac Surg
uation of 50 consecutive cases. Int J Oral Maxillofac Implants
41. Gorman LM, Lambert PM, Morris HF, Ochi S, Winkler S. The
24. Mensdorff-Pouilly N, Haas R, Mallath G, Watzed G. The immedi-
effect of smoking on implant survival at second-stage
ate implant: A retrospective study comparing the different
surgery. Implant Dent 1994;3:165–168.
types of immediate implantation. Int J Oral Maxillofac
42. Lindquist LW, Carlsson GE, Joemt T. Association between mar-
ginal bone loss around osseointegrated mandibular implants
25. Becker BE, Becker W, Ricci A, Geurs N. A prospective clinical
and smoking habits: A 10 year follow-up study. J Dent Res
trial of endosseous screw shaped implants placed at the time
of tooth extraction without augmentation. J Periodontol
43. Bain CA. Smoking and implant failure—Benefits of a smoking
cessation protocol. Int J Oral Maxillofac Implants
26. Grunder U, Polizzi F, Goene R, et al. A 3-year prospective multi-
center follow-up report on the immediate and delayed-imme-
44. Lambert PM, Morris HF, Ochi S. The influence of smoking on 3-
diate placement of implants. Int J Oral Maxillofac Implants
year clinical success of osseointegrated dental implants. Ann
27. Schwartz-Arad D, Gulayen N, Chaushu G. Immediate versus
45. Wallace RH. The relationship between cigarette smoking and
non-immediate implantation for full arch fixed reconstruction
dental implant failure. Eur J Prosthodont Restor Dent
following extraction of all residual teeth: A retrospective com-
parative study. J Periodontol 2000;71:923–928.
46. Grunder U, Gaberthuel T, Boitel N, et al. Evaluating the clinical
28. Schwartz-Arad D, Grossman Y, Chaushu G. The clinical effec-
performance of the Osseotite implant: Defining prosthetic
tiveness of implants placed immediately into fresh extraction
predictability. Compend Contin Educ Dent 1999;20:628–640.
sites of molar teeth. J Periodontol 2000;71:839–844.
47. Bain C, Weng D, Meltzer A, Kohles, Stach RM. A meta-analysis
29. Gomez-Roman G, Kruppenbacker M, Weber H, Schulte W.
evaluating the risk for implant failure in patients who smoke.
Immediate post extraction implant placement with not-ana-
Compend Contin Educ Dent 2002;23:695–706.
log stepped implants: Surgical procedure and statistical out-
48. Bain CA. Implant installation in the smoking patient. Periodon-
come after 6 years. Int J Oral Maxillofac Implants
tol 2000 2003;33:185–193.
49. Luepke PG, Mellonig JT, Brunsvold MA. A clinical evaluation of
30. Wagenberg BD, Ginsberg TR. Immediate implant placement
a bioresorbable barrier with and without decalcified freeze-
on removal of the natural tooth. Retrospective analysis of
dried bone allograft in the treatment of molar furcation. J Clin
1,081 implants. Compend Contin Educ Dent 2001;22:399–410.
31. Prosper L, Gherlome EF, Redalle S, Quaranja M. Four-year fol-
50. Köndell PÄ, Nordenram Ä, Landt H. Titanium implants in the
low up at large diameter implants placed in fresh extraction
treatment of edentulousness: Influence of patient's age on
sockets using a resorbable membrane or a resorbable allo-
prognosis. Gerodontics 1988;4:280–284.
plastic material. Int J Oral Maxillofac Implants
51. Dao TTT, Anderson JD, Zarb GA. Is osteoporosis a risk factor for
osseointegration of dental implants? Int J Oral Maxillofac
32. Covani U, Crespi R, Cornelini R, Barone A. Immediate implant
supporting single crown restoration. A 2-year prospective
52. Starck WJ, Epker BN. Failure of osseointegrated dental
study. J Periodontol 2004;75:982–988.
implants after diphosphonate therapy for osteoporosis: A
33. Bianchi AR, San Filippo F. Single tooth replacement by imme-
case report. Int J Oral Maxillofac Implants 1995;10:74–78.
diate implant and connective tissue graft. A 1-9 year clinical
53. Ruggiero SL, Mebrotra B, Rosenberg TJ, Engroff SI. Osteonecro-
evaluation. Clin Oral Implants Res 2004;15:269–277.
sis of the jaws associated with the use of bisphosphonates: A
34. Albrektsson T, Zarb GA, Worhtington P, Eriksson AR. The long-
review of 63 cases. J Oral Maxillofac Surg 2004;62:527–534.
term efficacy of currently used dental implants: A review and
54. Tokugawa Y, Shirota T, Ohno K, Yamaguchi A. Effects of bispho-
proposed criteria for success. Int J Oral Maxillofac Implants
sphonate on bone reaction after placement of titanium
implants in tibia of ovariectomized rats. Int J Oral MaxillofacImplants 2003;18:66–74.
The International Journal of Oral & Maxillofacial Implants
COPYRIGHT 2005 BY QUINTESSENCE PUBLISHING CO, INC.
PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY.
NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM
WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER.
Froum.qxd 1/23/06 10:57 AM Page 80
55. Shibutani T, Inuduka A, Horiki I, Luan Q, Iwayama Y. Bisphos-
60. Nevins M, Langer B. The successful use of osseointegrated
phonate inhibits alveolar bone resorption in experimentally
implants for the treatment of the recalcitrant periodontal
induced perio-implantitis in dogs. Clin Oral Implants Res
patient. J Periodontol 1995;66:150–157.
61. Mengel R, Stelzel M, Hasse C, Flores-de-Jacoby L. Osseointe-
56. Dahlin C, Lekholm U, Linde A. Membrane induced bone aug-
grated implants in patients treated for generalized severe
mentation at titanium implants. A report on ten implants fol-
adult periodontitis. An interim report. J Periodontol
lowed from 1 to 3 years after loading. Int J Periodontics
Restorative Dent 1991;11:272–281.
62. Ellegaard B, Baelum V, Karring T. Implant therapy in periodon-
57. Morris HF, Ochi S, Plezia R, et al. AICRG, Part III: The influence of
tally compromised patients. Clin Oral Implants Res
antibiotic use on the survival of a new implant design. J Oral
63. Rosenberg ES, Cho SC, Elian N, Jalbout ZN, Froum S, Evian CI. A
58. Dent CD, Olson JW, Farish SE, et al. The influence of preopera-
comparison of characteristics of implant failure and survival in
tive antibiotics on success of endosseous implants up to and
periodontally compromised and periodontally healthy
including stage II surgery: A study of 2,641 implants. J Oral
patients: A clinical report. Int J Oral Maxillofac Implants
Maxillofac Surg 1997;55(12 suppl 5):19–24.
59. Sennerby L, Dr O, ROOS J. Surgical determinants of clinical
success of osseointegrated oral implants: A review of the liter-ature. Int J Prosthodont 1998;11:408–420.
Volume 21, Number 1, 2006
COPYRIGHT 2005 BY QUINTESSENCE PUBLISHING CO, INC.
PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY.
NO PART OF THIS ARTICLE MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM
WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER.
Source: http://www.ladent.ru/Content/02review.pdf
NATURE Vol 465 20 May 2010 parasites (Toxoplasma, Leishmania and active compounds — and an earlier, partial y These reports1,2 offer tremendous opportunities trypano somes) and on replicating human cel described set8 identified in a high-throughput to develop the next generation of antimalarial lines, and found that most of the compounds screen against P. falciparum — should be a first drugs. They also sound a call for the academic
August /September 2006 – Issue No. 22 The New Zealand Fire Service Magazine Reaction August/September 2006 Issue No. 22 Fire & Rescue is the flagship publication of the New Zealand Fire Service. It is produced by Media, Promotions and Communications, National Headquarters, Level 9, 80 The Terrace, Wellington. Editor: Iain Butler