Ce 450 - pharmacology of systemic antibacterial agents: clinical implications

Pharmacology of Systemic Antibacterial Agents:
Leena Palomo, DDS, MSD; Géza T. Terézhalmy, DDS, MA
Continuing Education Units: 3 hours
Online Course:
Disclaimer: Participants must always be aware of the hazards of using limited knowledge in integrating new techniques or
procedures into their practice. Only sound evidence-based dentistry should be used in patient therapy.
Participants in this course will be introduced to evidence-based information related to the microbiology
of odontogenic infections, the pharmacology of systemic antibacterial agents, and the rationale for the
selection of an antibacterial agent for the treatment of odontogenic infections.
Conflict of Interest Disclosure Statement
• Dr. Palomo reports no conflicts of interest associated with this work.
• Dr. Terézhalmy has done consulting work for Procter & Gamble and is a member of the dentalcare.com
Advisory Board.
The Procter & Gamble Company is an ADA CERP Recognized Provider.
ADA CERP is a service of the American Dental Association to assist dental professionals in identifying
quality providers of continuing dental education. ADA CERP does not approve or endorse individual courses
or instructors, nor does it imply acceptance of credit hours by boards of dentistry.
Concerns or complaints about a CE provider may be directed to the
provider or to ADA CERP at: http://www.ada.org/cerp
Approved PACE Program Provider
The Procter & Gamble Company is designated as an Approved PACE Program Provider
by the Academy of General Dentistry. The formal continuing education programs of this
program provider are accepted by AGD for Fellowship, Mastership, and Membership
Maintenance Credit. Approval does not imply acceptance by a state or provincial board
of dentistry or AGD endorsement. The current term of approval extends from 8/1/2013 to
7/31/2017. Provider ID# 211886
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
Participants in this course will be introduced to evidence-based information related to the microbiology of
odontogenic infections, the pharmacology of systemic antibacterial agents, and the rationale for the selection
of an antibacterial agent for the treatment of odontogenic infections.
Upon completion of this course, the dental professional should be able to:
• Discuss the microbiology of odontogenic infections.
• Discuss the pharmacology of systemic antibacterial agents.
• Select the most appropriate antibacterial agent to treat an odontogenic infection.
• Discuss potential ADEs associated with the administration of antibacterial agents.
the normal flora establish symbiotic relationships
(mutualism, commensalisms, or parasitism) with
• Microbiology of Odontogenic Infections
their human host and each other.2,3
• Pharmacology of Systemic Antibacterial Agents
Inhibitors of Bacterial Cell Wall Synthesis
Factors that modify or shift the balanced
Inhibitors of DNA Synthesis or Integrity
environment of the normal flora (age, altered
Inhibitors of Transcription or Translation
anatomy, diet, local and systemic conditions,
• Strategies for the Treatment of Odontogenic
or pharmacotherapy) may predispose an
individual to infection.4,5 Infection, the invasion
Primary Dental Care
and multiplication of microorganisms in body
Adjunctive Antibacterial Chemotherapy
tissues, results in cellular injury due to competitive
Prophylactic Antibacterial Chemotherapy
metabolism, toxin production, or immune-mediated
• Prescription-precautions Associated with
reactions. An infection may be autogenous,
Antibacterial Agents
caused by the body's normal flora; or it may be
Antibacterial Drug-resistance
a cross-infection, related to the proliferation of
Gastrointestinal Distress
transient organisms.6
Hypersensitivity Reactions
Cardiovascular Effects
Microbiology of Odontogenic Infections
Central Nervous System Effects
Predicated on their metabolic characteristics, i.e.,
Oral Candidiasis
their metabolic demand for oxygen, bacteria are
Antibacterial Drugs and Pregnancy
classified as aerobic, facultative, or anaerobic.
Antibacterial Drugs and Nursing
Morphologically, they are characterized as cocci
Drug-drug Interactions
or bacilli (rods). Based on Gram's Method of
staining (Box 1), bacteria are further classified
• Course Test Preview
as gram-positive or gram-negative. The distinct
staining properties of bacteria are related to their
• About the Authors
architectural and biochemical differences.7
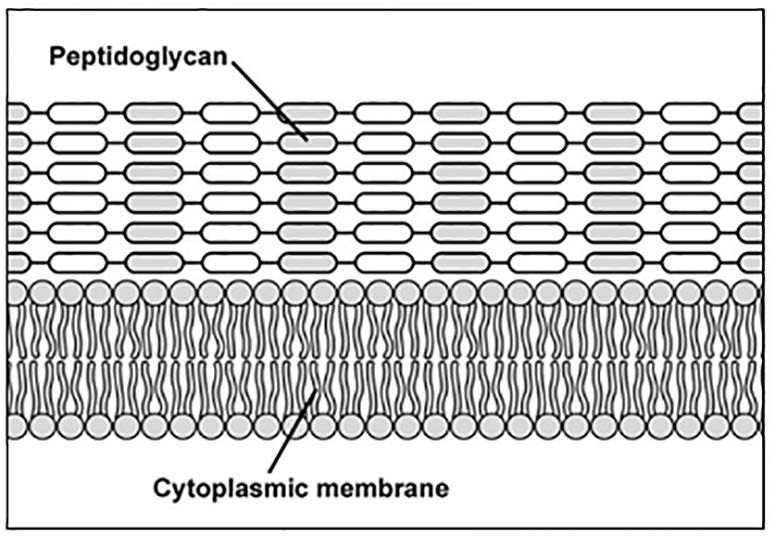
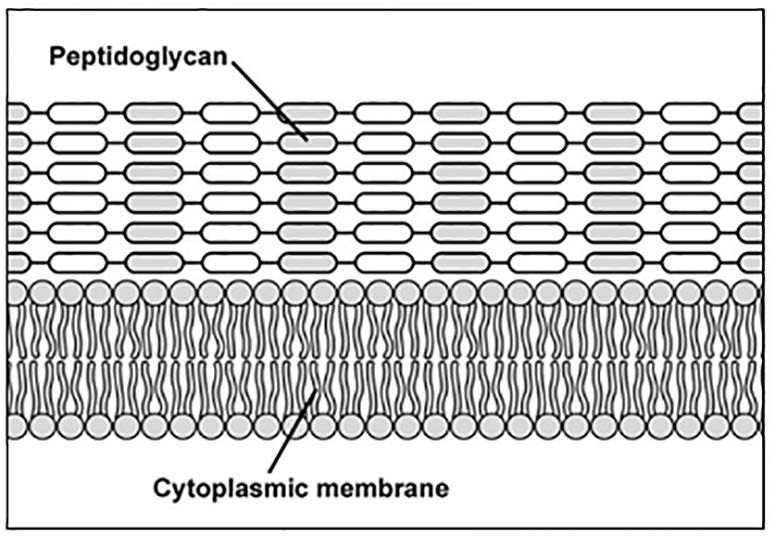
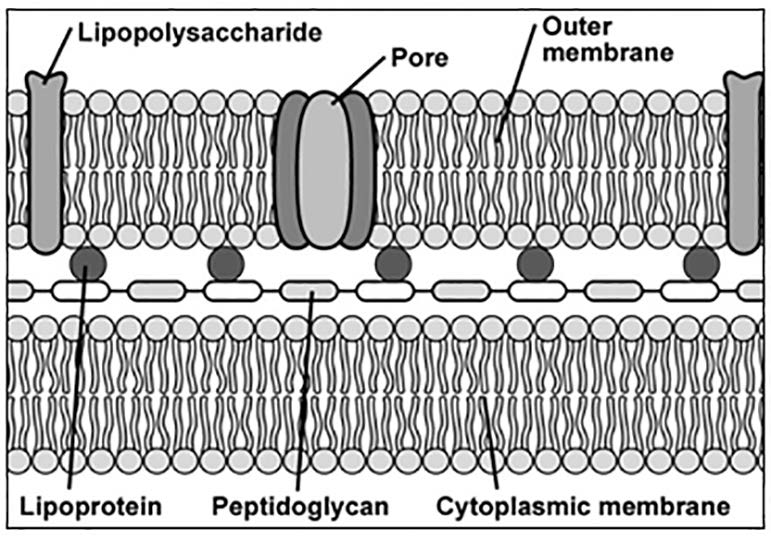
Gram-positive bacteria possess a thick
The human fetus is free of microorganisms.1
peptidoglycan cell wall interspersed with
After initial exposure at birth, most organisms are
lipoteichoic acid underlain by the cytoplasmic
soon eliminated, but others become permanently
membrane (Figure 1).8 Gram-negative bacteria
established and the dynamic process of
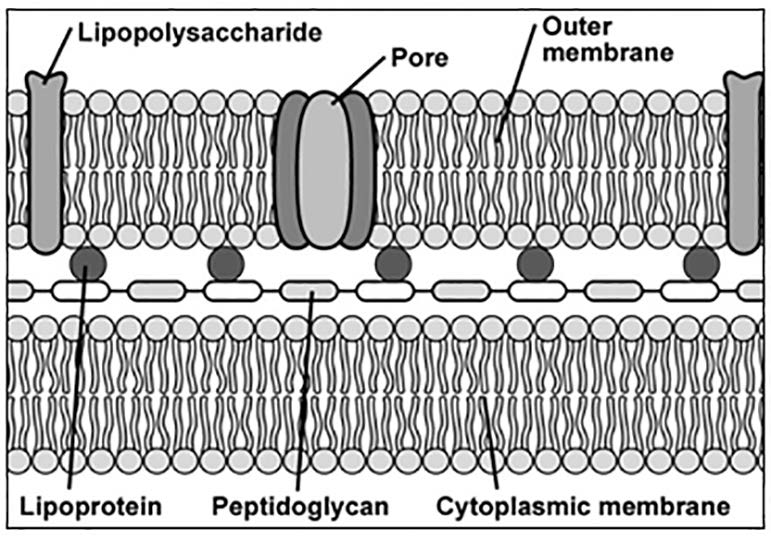
have an outer membrane with lipopolysaccharides
colonization begins. The adult body harbors a
and a lipoprotein layer underlain by a thin
dense, diverse, indigenous flora that includes
peptidoglycan layer and the cytoplasmic
bacteria, viruses, fungi and protozoa. Interaction
membrane (Figure 2).8 The ability of antibacterial
between these various microbial ecosystems
agents to diffusion into bacteria is also affected by
determines the normal flora. Microorganisms of
these structural differences.
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
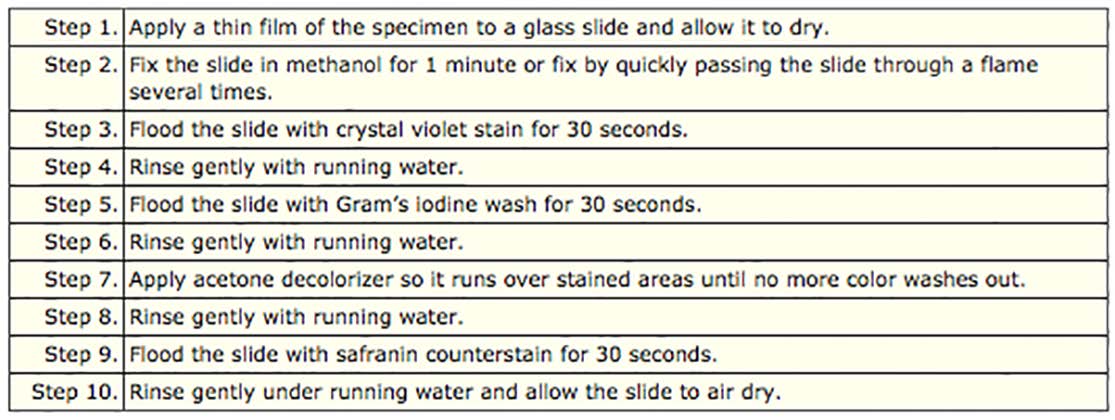
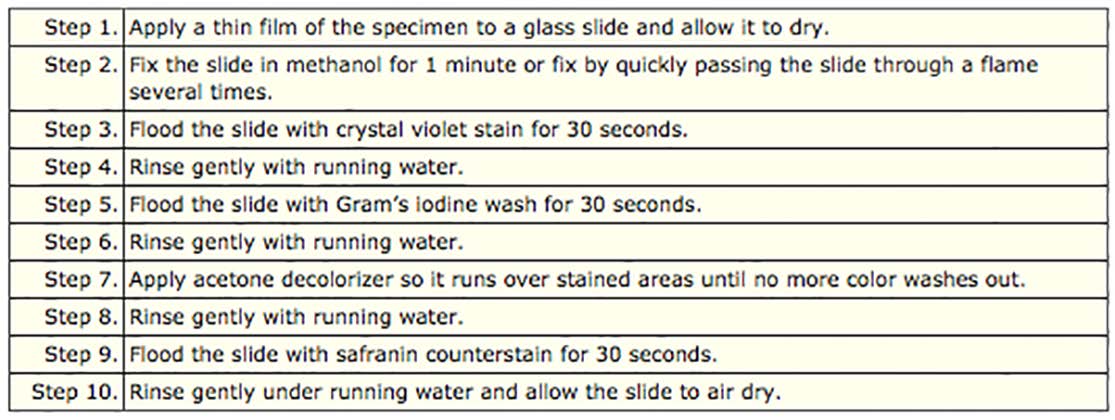
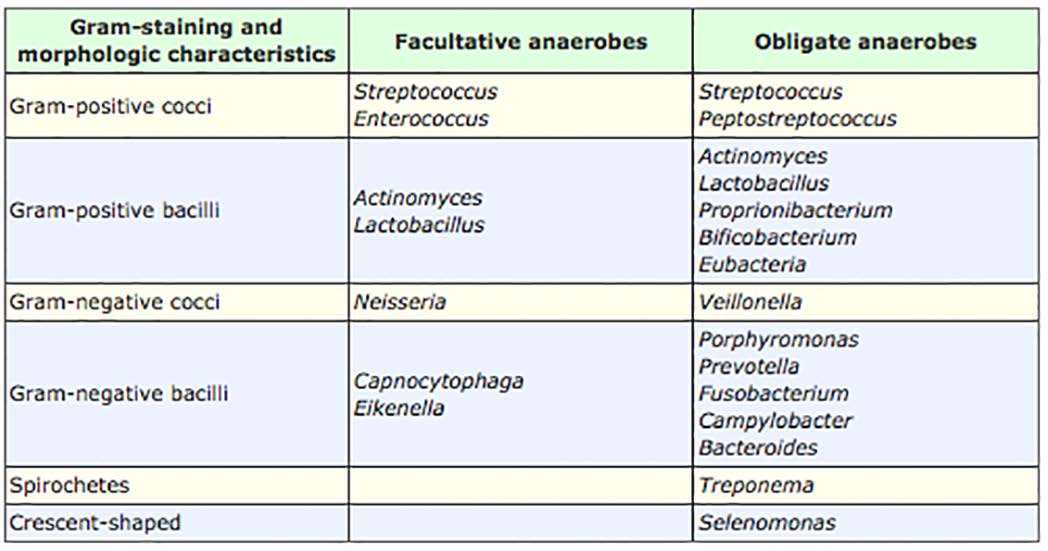
Box 1. Gram's Method of staining.7
Figure 1. Gram-positive bacteria.
Figure 2. Gram-negative bacteria.
Images 1&2, modified from Kasmar AG, Hooper D. Pharmacology of bacterial
infections: cell wall synthesis. In Golan DE, Tashjian, Jr. AH, Armstrong EJ, Armstrong
AW. Ed. Principles of pharmacology. The pathophysiologic basis of drug therapy. 2nd
ed. 2008. Wolters Kluwer/Lippincott Williams & Wilkins. Baltimore, MD.8
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
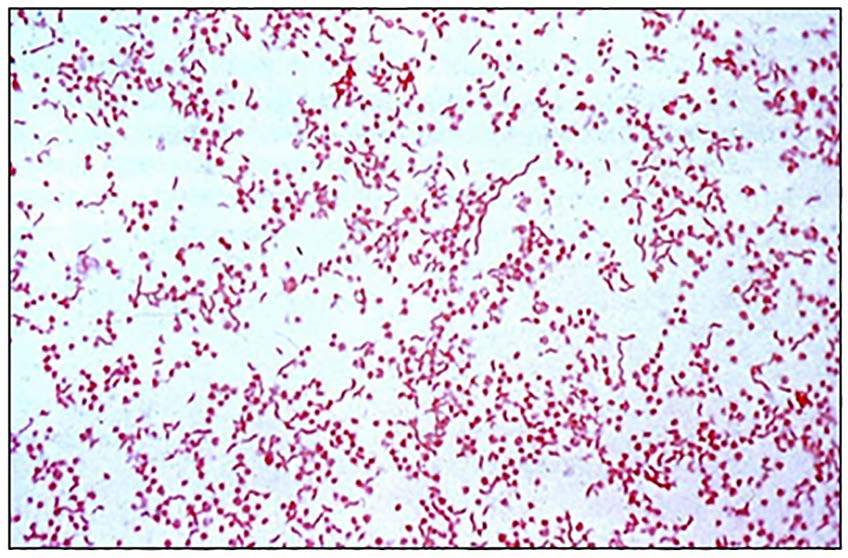

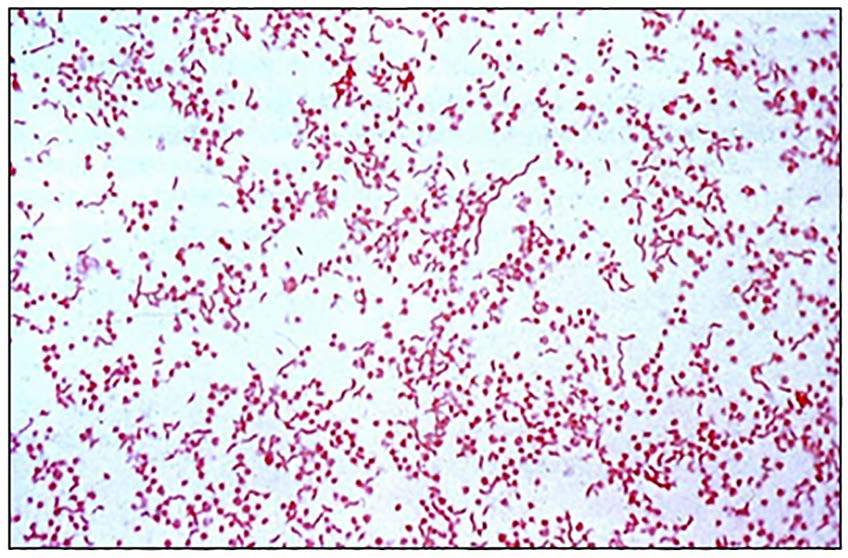
Figure 3. Gram-negative organisms.
Figure 4. Mixed gram-positive and gram negative organisms.
During staining, crystal violet interacts with iodine
acidic environment and decreased oxygenation
forming a complex. Acetone extracts lipids from
to support the growth and proliferation of its
the outer membrane, cell wall, and cytoplasmic
members. Ultimately, facultative and anaerobic
membrane of bacteria.7 The damage to gram-
gram-positive and gram-negative cocci and bacilli
negative organisms is more extensive and they
predominate in all types of odontogenic infections
lose their crystal violet-iodine complexes, i.e.,
they are decolorized; and when counterstained
with safranin, they appear red (Figure 3).7 Gram-
Pharmacology of Systemic Antibacterial
positive bacteria retain their crystal violet-iodine
complexes and appear deep purple (Figure 4).7
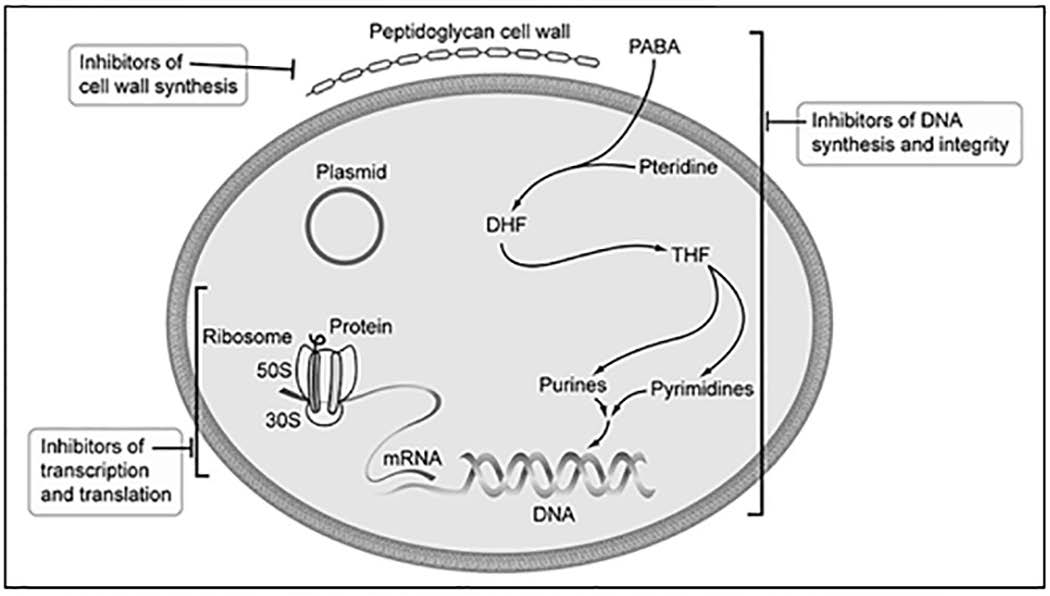
Pharmacological strategies are predicated
on targeting differences between prokaryotic
An average adult harbors at least 300 oral
bacterial and eukaryotic host cells. Selective
bacterial species and more than 700 strains of
toxicity can be achieved by (1) attacking targets
bacteria have been isolated from test cases.9-11
unique to bacteria, (2) attacking targets in bacteria
Most odontogenic infections are polymicrobial.
similar but not identical to those in host cells, and
The number of strains per infection ranges from
(3) attacking targets that are shared, but vary
1 to 10 with an average number of 4 isolates.9,12-24
in importance between bacteria and host cells
The predominant flora creates an ecosystem
(Figure 5).32 Drugs targeting unique differences
of synergism by elaborating a more favorable
are the least toxic to host cells.
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
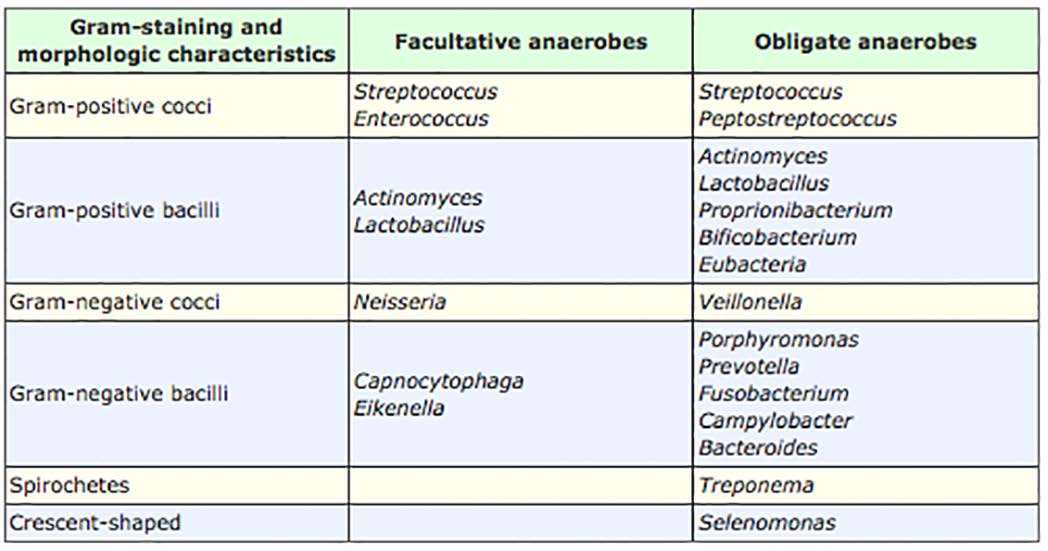
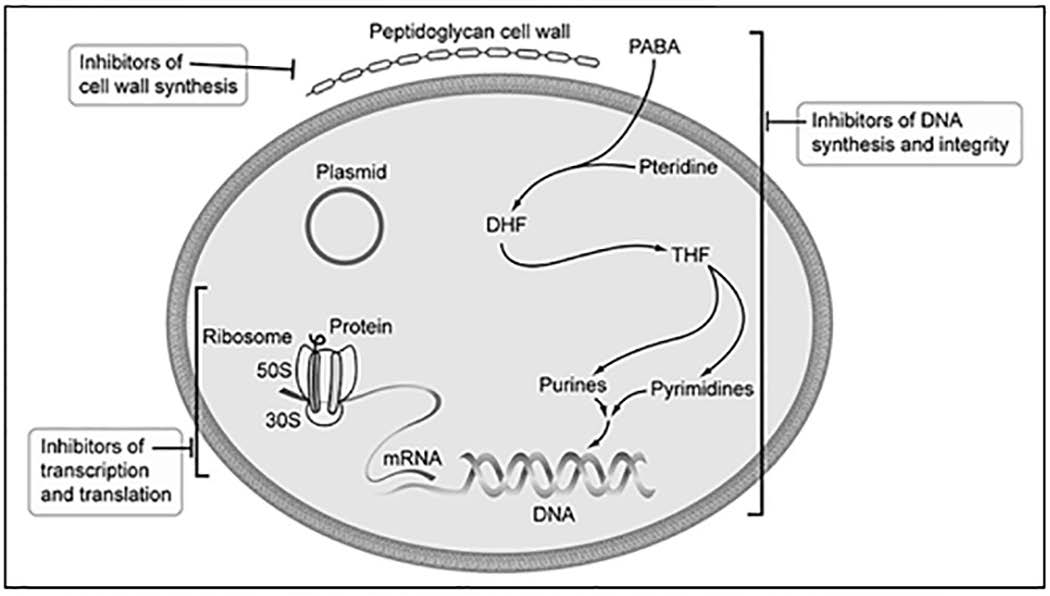
Table 1. Bacteria detected in odontogenic infections.26,27
Figure 5. Mechanisms of action of antibacterial agents.
Based on Harbison H, Rose HS, Coen DM, Golan DE. Principles of antibacterial and antineoplastic pharmacology. In
Golan DE, Tashjian, Jr. AH, Armstrong EJ, Armstrong AW. Ed. Principles of pharmacology. The pathophysiologic basis
of drug therapy. 2nd ed. 2008. Wolters Kluwer/Lippincott Williams & Wilkins. Baltimore, MD.32
Antibacterial agents are either bactericidal or
Inhibitors of Bacterial Cell Wall Synthesis
bacteriostatic. Bactericidal drugs attack targets
Most pathogenic bacteria have a cell wall that
essential for bacterial survival, e.g., inhibitors
provides tensile strength and maintains intracellular
of cell wall synthesis and most inhibitors of
osmotic pressure. Its synthesis progresses in
DNA synthesis and integrity.32 Bacteriostatic
three steps: (1) monomers are synthesized in
drugs attack targets that are necessary for
the cytoplasm from amino acid and sugar building
bacterial growth but not for survival, e.g., most
blocks; (2) Bactoperol transfers the monomers
inhibitors of transcription and translation.32 Since
across the cytoplasmic membrane where they
bacteriostatic drugs block bacterial replication,
are polymerized into linear peptidoglycan chains;
they antagonize the effects of bactericidal drugs.
finally, (3) transpeptidase cross-links peptidoglycan
chains into a three-dimensional mat (Figure 6).8
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
Figure 6. Bacterial cell wall synthesis.
Modified from Kasmar AG, Hooper D. Pharmacology of bacterial infections: cell wall synthesis. In Golan DE, Tashjian, Jr. AH, Armstrong EJ,
Armstrong AW. Ed. Principles of pharmacology. The pathophysiologic basis of drug therapy. 2nd ed. 2008. Wolters Kluwer/Lippincott Williams &
Wilkins. Baltimore, MD.8
A number of drugs inhibit cell wall synthesis.
potassium and broad-spectrum amoxicillin and
Most important are Vancomycin, which targets
amoxicillin with clavulanic acid have the requisite
monomer polymerization; and the β-lactams,
spectra to be considered as empirical options
e.g., penicillins and cephalosporins, which block
in treating odontogenic infections.10,42 However,
polymer cross-linking.8,33-41 β-lactam antibacterial
neither narrow-spectrum nor broad-spectrum
agents also activate autolysins. Autolysins punch
penicillins are active against β-lactamase
holes in bacterial cell wall and disrupt its integrity.8
producing bacteria; and certain β-lactamases
Transpeptidase antagonism and autolysis prevent
produced by bacteria now confer resistance to
bacterial self-maintenance, i.e., remodeling and
clavulanic acid as well.8,43-51
repair; and replication.
Penicillin V potassium and amoxicillin formulations
are not inactivated by gastric acid and also have
Vancomycin is bactericidal in susceptible
the advantage that they may be given with meals.
organisms. It is primarily effective against aerobic
They are widely distributed to most tissues and
gram-positive cocci and bacilli.8,33,36,37 It does have
body fluids, cross the placenta and they are
activity against some anaerobic gram-positive,
excreted into breast milk. The penicillins undergo
but not against gram-negative bacilli. Since
hepatic biotransformation. The metabolites and
facultative and anaerobic gram-positive and
the unchanged fraction of the drugs are excreted
gram-negative cocci and bacilli predominate in all
rapidly in individuals with normal renal function.
types of odontogenic infections, Vancomycin does
not have the requisite spectrum to be considered
an empirical option in treating odontogenic
The cephalosporins are bactericidal in susceptible
organisms.8,35,40,41,52 Most are primarily active
against aerobic gram-positive cocci and bacilli.
Second generation cephalosporins (e.g., cefaclor)
Penicillins are bactericidal in susceptible
have an overlapping spectra with those of
organisms.8,38,39 Narrow-spectrum penicillin V
penicillin V potassium and amoxicillin formulations
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
Figure 7. Folate synthesis.
Modified from Harbison H, Rose HS, Coen DM, Golan DE. Principles of antibacterial and antineoplastic pharmacology.
In Golan DE, Tashjian, Jr. AH, Armstrong EJ, Armstrong AW. Ed. Principles of pharmacology. The pathophysiologic
basis of drug therapy. 2nd ed. 2008. Wolters Kluwer/Lippincott Williams & Wilkins. Baltimore, MD.32
and are more β-lactamase resistant than the
aerobic gram-positive and gram-negative
first generation cephalosporins. However,
cocci and bacilli.53-57 The newer agents (e.g.,
cephalosporins, in general, offer no therapeutic
moxifloxacin) have some anaerobic activity.10,58,59
advantage over penicillins as empirical options in
Fluoroquinolones are indicated for the treatment
treating odontogenic infections.
of infections with designated, susceptible
bacteria and are not empirical options in treating
Inhibitors of DNA Synthesis or Integrity
Cell wall inhibitors cannot kill all bacteria because
some bacteria lack a cell wall. Other bacteria
have unique structures that inherently resist the
A metabolite of metronidazole directly binds
accumulation or action of cell wall inhibitors.
DNA, causes loss of its helical structure, and
However, bacteria, in preparation for cell division,
effects strand breakage.50,60,61 It is bactericidal in
must replicate their double stranded DNA. To
susceptible organisms. Metronidazole is active
facilitate replication, topoisomerase type II, a
against most obligate anaerobes, but lacks
bacterial DNA gyrase, must first unwind and
clinically relevant activity against obligate aerobes
separate, and then reassemble the original DNA
and facultative anaerobes.61,62 Metronidazole,
during the process.53
in combination with an agent active against
aerobic/facultative organisms (e.g., penicillin),
In the replication process, bacteria must
is an empirical option in treating odontogenic
synthesize folate. Its synthesis begins with
the formation of dihydropteroic acid from
pteridine and para-aminobenzoic acid (PAPA), a
Metronidazole is well absorbed after oral
reaction catalyzed by dihydropteroate synthase
administration and reaches peak plasma
(Figure 7).32 Dihydropteroic acid and glutamate
concentrations in 1 to 2 hours.61 It is distributed
condense to form dihydrofolate (DHF).32
to most body fluids and tissues, including bone;
Dihydrofolate reductase (DHFR) reduces DHF
crosses the placenta, and reaches concentrations
to tetrahydrofolate (THF). THF is an essential
in saliva and human milk similar to those found in
cofactor in the synthesis of DNA, RNA, and
plasma.61 Metronidazole is metabolized by hepatic
proteins (Figure 7).32
oxidation and glucuronic conjugation.61 The major
route of elimination of metronidazole and its
metabolites is via the kidneys.61
Fluoroquinolones block topoisomerase type
II activity and disrupt the integrity of bacterial
DNA.53-57 They are bactericidal in susceptible
Sulfamethoxazole (SMX) and trimethoprim
organisms and are primarily active against
(TMP), block succeeding steps in folate synthesis
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
(see Figure 7).32,63 SMX-TMP formulations are
The P-site initially is occupied by the fMet-tRNA
bacteriostatic in susceptible organisms. It has
complex. As the next charged tRNA binds to
activity against a broad spectrum of aerobic gram-
the 70S ribosomal unit, but before it is allowed
positive and gram-negative organisms, but it is not to enter the unoccupied A-site, the rRNA must
active against anaerobes.63 SMX-TMP does not
confirm that the charged tRNA carries the specific
have the requisite spectrum to be considered an
amino acid called for by the mRNA codon.54 If
empirical option in treating odontogenic infections.
access is allowed, the rRNA catalyzes the
formation of a peptide bond between the carboxy-
Inhibitors of Transcription or Translation
terminal of the fMet residing in the P-site and the
Bacteria, like mammalian cells, must synthesize
new amino acid occupying the A-site (Figure 9).53
proteins for self-maintenance and replication. DNA
serves as the "instruction manual;" it provides
Once the peptide bond is formed, the tRNA
the information necessary for protein synthesis.
originally linked to fMet is ejected from the P-site
The first step in this process is transcription,
and the second tRNA located at the A-site, which
the synthesis of a single-stranded ribonucleic
is now linked to two amino acids, translocates to
acid (RNA) from the DNA template catalyzed by
the unoccupied P-site (Figure 9).53 As the process
RNA polymerase.53 The function of the newly
repeats itself, a growing peptide chain emerges
synthesized RNA is translation.
from the exit tunnel.53 Translation continues until
a stop codon is encountered in the mRNA and the
In the process of translation, RNA serves three
newly synthesized protein is released from the
functions: (1) as messenger RNA (mRNA), it
tells ribosomes which proteins to synthesize; (2)
as transfer RNA (tRNA), it transports specific
amino acids called for by mRNA codons from the
Tetracycline and its semi-synthetic derivatives
cytoplasm to ribosomes; and (3) as ribosomal
(e.g., minocycline and doxycycline) bind to 30S
RNA (rRNA), it ensures that the amino acid carried ribosomal subunits and reversibly block the
by the charged tRNA is the one called for by the
attachment of the charged tRNA to the aminoacryl
corresponding mRNA codon.53
or A-site.53,64-66 They have bacteriostatic activity
against aerobic gram-positive and gram-negative
Protein synthesis is initiated when the mRNA joins
organisms, but in vivo many strains have been
with the 30S ribosomal subunit and tRNA-linked
shown to be resistant. Tetracyclines are not
formyl methionine (fMet).53 As the first amino
empirical options in the treatment of odontogenic
acid encoded by every bacterial mRNA, fMet
binds the initiation codon on the mRNA.53 Next,
the 30S-fMet-tRNA complex joins with the 50S
It is also of note that tetracyclines are
ribosomal subunit to form the complete initiation
teratogenic.65-67 They produce higher rates of
complex, i.e., the 70S ribosomal unit, which
neuronal-tube defect, cleft palate, and multiple
contains two binding sites, an aminoacyl or A-site
congenital abnormalities, e.g., neuronal-tube
and a peptidyl or P-site (Figure 8).53
defect with cardiovascular malformation.
Figure 8. Formation of the 70S ribosomal initiation complex.
Modified from Ryou M, Coen DM. Pharmacology of bacterial infections: DNA replication, transcription, and translation.
In Golan DE, Tashjian, Jr. AH, Armstrong EJ, Armstrong AW. Ed. Principles of pharmacology. The pathophysiologic
basis of drug therapy. 2nd ed. 2008. Wolters Kluwer/Lippincott Williams & Wilkins. Baltimore, MD.53
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
Figure 9. The process of protein synthesis.
Modified from Ryou M, Coen DM. Pharmacology of bacterial infections: DNA replication, transcription, and translation.
In Golan DE, Tashjian, Jr. AH, Armstrong EJ, Armstrong AW. Ed. Principles of pharmacology. The pathophysiologic
basis of drug therapy. 2nd ed. 2008. Wolters Kluwer/Lippincott Williams & Wilkins. Baltimore, MD.53
Furthermore, tetracyclines induce enamel
hypoplasia and discoloration of teeth. Before
Macrolides bind 50S ribosomal subunits and block
prescribing tetracycline during pregnancy and/or
translocation and peptide movement through the
tooth development the benefits and risks must be
exit tunnel.53 They are bacteriostatic in susceptible
organisms and are active against aerobic gram-
positive cocci and gram-negative bacilli, but
anaerobic gram-negative organisms are resistant.
Aminoglycosides (e.g., gentamicin) bind to 30S
Azithromycin has an extended spectrum that
ribosomal subunits and induce misreading of
includes some anaerobic gram-positive cocci
mRNA codons.53,68,69 They are bactericidal in
and gram-negative bacilli and may be considered
susceptible organisms and are active against
an empirical option in treating odontogenic
many aerobic and facultative gram-positive and
gram-negative cocci and bacilli, but most species
of streptococci and anaerobic gram-negative
Azithromycin is rapidly absorbed after oral
bacilli are resistant.53,68,69 Aminoglycosides do
administration. When administered with food,
not have the requisite spectra to be considered
however, its rate and extent of absorption is
empirical options in treating odontogenic
reduced by about 50%. The drug is widely
distributed throughout the body, accumulating in
high concentration within cells resulting in higher
tissue than plasma concentrations. Azithromycin is
Clindamycin binds to 50S ribosomal subunits and
metabolized minimally and is principally eliminated
blocks peptide bond formation between amino
as unchanged drug via the liver.
acids located in the P- and A-sites (Figure 8).53,62,70
It has excellent activity against gram-positive
Strategies for the Treatment of
aerobes and anaerobes, as well as gram-negative
anaerobes.10,42,71 Consequently, clindamycin
Uncomplicated odontogenic infections manifest
has the requisite spectrum to be considered an
primarily as caries; and pulpal, periodontal, and
empirical option in treating odontogenic infections.
pericoronal problems. Signs and symptoms include
pain, erythema, edema, and difficulty chewing.71,79
Clindamycin is rapidly and almost completely
Complicated odontogenic infections reflect the
absorbed after oral administration and reaches
extension of an uncomplicated odontogenic infection
peak plasma concentration in about 45 minutes.
into surrounding tissues and manifest as cellulitis,
It is widely distributed in body fluids and tissues
osteomyelitis, and space infections. Signs and
(including bone). Clindamycin is extensively
symptoms include lymphadenitis, trismus, difficulty
metabolized in the liver and its metabolites are
swallowing or breathing; and less frequently, fever
excreted primarily by the kidneys.
and hypotension.71,79
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
Primary Dental Care
course of penicillin administered to patients with
acute pain related to a tooth with an amalgam
restoration without clinical signs of infection,
Patients with reversible pulpitis usually report
in the absence of definitive dental care, did
sensitivity or pain in response to hot, cold,
not prevent the emergence of clinical signs of
sweets, and mechanical stimuli. Caries in
infection within 5 days.89
proximity of the pulp, defective restorations,
exposed dentinal tubules, and traumatic occlusion
Acute Apical Periodontitis
appear to be common etiologies. Provoked pain,
Irreversible pulpitis and pulpal necrosis (an
described as sharp or intense, primarily reflects
asymptomatic complication of irreversible
hyperemia or mild inflammation of the pulp and
pulpitis), if left untreated, lead to the spread of
stimulus-induced fluid movement in dentinal
irritants and bacteria into periradicular tissues
and result in acute apical periodontitis. Patients
complain of tenderness or mild to moderate pain
Reversible pulpitis is a reactive process. Caries
associated with the apical area of the offending
should be excavated and a temporary sedative
tooth. The pain may be intermittent, secondary
restoration placed. Faulty restorations should
to manipulation of the tooth, or unprovoked and
be removed and replaced. Exposed dentinal
tubules should be etched and sealed. To reduce
inflammation and shorten recovery time a
The removal of bacteria and their byproducts
disease-modifying analgesic, i.e., a nonsteroidal
by debridement and obturation of the root canal
anti-inflammatory drug (NSAIDs) should be
system effectively eliminates infection, curtails
prescribed. It is intuitive that antibacterial agents
inflammation, and promotes healing. The
would have no effect on clinical outcome.
administration of a disease modifying analgesic,
i.e., a NSAID, may shorten recovery time. It has
been shown that once the source of infection
Bacteria may gain access to the pulpal system
is eliminated, the administration of penicillin
through caries, defective restorations, and
provides no statistically significant added benefit.90
exposed dentinal tubules. Other portals may
include apical, lateral, or furcation canals
Acute Apical Abscess
associated with advancing periodontal disease.
Infection associated with acute apical periodontitis
Pain may be spontaneous, but usually it is in
may extend into alveolar bone and soft tissues
response to hot, cold, sweets, and mechanical
initiating apical abscess formation. The pain is
stimuli reflects hyperemia or inflammation
usually severe, unprovoked and constant. The
secondary to infection, fluid movement in dentinal
tooth is usually mobile and the accumulation of
tubules, and increased intrapulpal pressure.
fluid in the periodontal ligament space may cause
supraeruption. Manipulation of the tooth causes
Acute dental pain associated with a tooth with
exquisite sensitivity and mastication is difficult;
deep carious lesion may reflect a reactive
swelling, malaise and fever may be present.
process to caries, but most likely to bacteria
that have infected pulpal tissues.80-85 In case
The removal of bacteria and their byproducts
of irreversible pulpitis endodontic debridement
by debridement and obturation of the root canal
and obturation of the root canal system is the
system effectively eliminates infection, curtails
most predictable method of treatment.86 To
inflammation, and promotes healing. The
reduce inflammation and shorten recovery time a
swelling, when present, may be drained through
disease-modifying analgesic, i.e., a NSAID should
the tooth, by a soft tissue incision, or there may
be prescribed.
already be drainage through a naturally occurring
sinus tract. A disease modifying analgesic, i.e., a
In untreated irreversible pulpitis, penicillin does
NSAID, may shorten recovery time.
not reduce spontaneous pain, percussion induced
pain, or the amount of analgesics taken by
In a prospective study, a five-day course of
patients.87,88 In a prospective study, a five-day
penicillin administered to patients with acute
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
pain related to a tooth with large periapical
rinse with warm saline every 2 hours for two days.
radiolucency, but without clinical signs of
Routine antibacterial therapy is not indicated.
infection, in the absence of debridement did
not prevent the development of clinical signs of
infection within 5 days.89 Another study confirmed
A periodontal abscess may be secondary to
that once the source of infection is eliminated, the
impacted foreign objects into the orifice of a
administration of penicillin provides no statistically
periodontal pocket, closure or narrowing of
significant added benefit.91
the pocket orifice, or improper use of irrigating
devices. Mild to moderate pain may be acute or
Draining Sinus Tract
chronic. The swelling rarely spreads beyond the
Inflammatory degeneration of the pulp and
mucogingival junction and may be associated with
periradicular tissues may follow a chronic
a draining sinus tract located in the gingival crevice
subclinical course. The infection progresses
or at the mucogingival junction.
slowly through cancellous bone along the
path of least resistance. It perforates the
Drainage should be established with the careful
thin cortical plate and forms a subperiosteal
use of a periodontal probe. Once the opening to
abscess. Once through the periosteum, it
the pocket is located, the root surface should be
spreads into surrounding soft tissues and leads
gently debrided. If drainage cannot be established
to the formation of either an intraoral or extraoral
through the orifice of the pocket, a vertical incision
draining sinus tract; swelling and pain are usually
should be made and the area should be irrigated
with warm saline. The patient should continue to
rinse with warm saline every 2 hours for two days.
In restorable teeth, chronic draining sinus
Routine antibacterial therapy is not indicated.
tracts will respond to nonsurgical endodontic
therapy. Successful healing depends on optimal
debridement and obturation of the canal system.
Necrotizing ulcerative gingivitis (NUG) is
Non-restorable teeth and/or those with extensive
characterized by localized necrosis and ulceration
alveolar bone loss require extraction. There
usually of the interdental papillae, which may
is no evidence that the routine administration
extend to the marginal gingiva and rarely the whole
of an antibacterial agent improves therapeutic
mouth. Microorganisms have been implicated, but
outcome.92 The residual cutaneous defect or scar
it is unclear if they are causative or opportunistic.
may require subsequent surgical revision.
Patients report a putrid odor, a foul metallic taste,
and constant radiating pain intensified by spicy or
hot foods, and gentle probing.
Gingival abscess is a localized, rapidly evolving,
painful infection of the marginal or interdental
The initial treatment of necrotizing ulcerative
gingiva usually secondary to the impaction of
gingivitis includes gentle irrigation of the affected
foreign bodies, e.g., popcorn shells, peanut
areas with warm saline; followed by careful
husks, seeds, fish bones, toothbrush bristles,
curettage of necrotic/ulcerative lesions and root
or toothpick splinters into the gingival crevice.
surfaces to reduce the bioburden. Patients are
The abscess may drain through the crevice or a
instructed to rinse with warm saline every 2 hours
draining sinus tract through the gingiva. Affected
and undergo daily repeat debridement until the
teeth may be extruded and tender to percussion.
lesions have resolved. Routine antibacterial
therapy is not indicated and response to
Foreign objects tend to adhere to the soft tissue
debridement is noted within 2-3 days. Patients
wall of the gingival crevice. Following the
may require gingivoplasty to correct residual crater-
application of a topical anesthetic agent, the
like gingival defects.
gingival tissue should be gently distended; the
foreign object removed, the soft tissue wall of
the lesion should be gently curetted to induce
Alveolar osteitis is a relatively common
drainage, and the area should be irrigated with
complication of tooth extraction, usually of
warm saline. The patient should continue to
mandibular molars. A foul taste, putrid odor, and
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
deep, radiating pain of increasing intensity is
noted three to four days following extraction.
When pulpal, periodontal or pericoronal infections
The surrounding soft tissues appear normal
overwhelm host resistance, the infection may
but the alveolar socket is empty or contains
extend into the surrounding tissues and cause
necrotic debris. Alveolar osteitis is primarily
cellulitis.93,95 The affected area becomes
an inflammatory condition, which may become
edematous and feels indurated when palpated
suggesting diffuse inflammation. Patients
present with pain, malaise, trismus, regional
A common protocol to manage alveolar osteitis
lymphadenopathy, and fever. The tissues
consists of gentle debridement of the socket,
overlying the infected area may appear bluish.
irrigation with warm saline, and placement of an
iodophor gauze impregnated with eugenol. The
Patients with cellulitis should be referred to a
patient should be reevaluated every 24 to 48
surgical specialist who may collect a sample
hours, the dressing removed, the socket irrigated
of the purulent exudate, usually by aspiration,
with warm saline and redressed. This cycle may
and initiate empirical, usually oral antibacterial
have to be continued for up to 14 days. Routine
chemotherapy. As the infection consolidates and
antibacterial therapy is not indicated.
becomes fluctuant, it will be incised at its most
dependent area, the purulent material evacuated,
and a drain inserted. Once a subacute condition
Pericoronitis is an acute infection most often
has been attained appropriate primary dental
associated with soft tissue overlying a partially
intervention should be initiated.
erupted mandibular third molar. Signs and
symptoms include pain, malaise, fever,
lymphadenopathy, trismus, and difficulty
Osteomyelitis is another potential complication
swallowing. Abscess formation may be evident
of odontogenic infection. It most often affects
buccally or lingually to the offending tooth, which
cancellous medullary bone of the mandible. As
may progress to cellulitis or osteomyelitis; or
purulence accumulates, it restricts blood flow to
spread through the fascial planes of the head and
the area, which causes osseous necrosis and the
formation of sequestrum. Signs and symptoms
include paresthesia or deep persistent pain,
To establish drainage from under the operculum,
malaise, fever, lymphadenopathy, loose teeth,
a periodontal probe should be inserted into the
and in the later stages, alveolar radiolucencies.
follicular space enlarging the opening. The area
under the operculum should be irrigated with
When osteomyelitis is suspected, the patient
warm saline and iodophor gauze impregnated
should promptly be referred to a surgical
with eugenol placed to maintain drainage. If
specialist who will collect a sample of the purulent
the opposing maxillary tooth is traumatizing the
exudate, usually by aspiration, for culture and
operculum and deemed nonfunctional, it may be
susceptibility testing and begin immediate
extracted. Otherwise, the cusps may be slightly
empirical, usually intravenous antibacterial
reduced to minimize further trauma to the soft
chemotherapy. Drainage is established at the
tissue below.
earliest possible time. Close monitoring and
modification of antibacterial chemotherapy, if
The patient should rinse with warm saline every
indicated, is imperative.
2 hours. Depending on associated signs and
symptoms, i.e., clinical evidence of induration as
the infection is spreading buccally or lingually and
The inflammatory process associated
the presence of trismus, empirical antibacterial
with cellulitis is usually restricted to the
therapy may be initiated. When a subacute
jaws. However, if timely treatment is not
condition has been attained, usually within 48
initiated, the infection may spread through
hours, and the tooth is to be maintained, the
the fascial planes of the head and neck into
operculum should be removed at this time;
the canine, buccal, masticatory, submental,
otherwise the tooth may now be extracted.
sublingual, submandibular, vestibular, parotid,
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
parapharyngeal, retropharyngeal, and deep
patients, into anatomical spaces contiguous with
spaces of the head and neck and mediastinum
fascial planes and can lead to serious, even life-
creating life-threatening situations.
threatening infections.20,101 Adjunctive antibacterial
chemotherapy, predicated on sound principles,
When space infection is suspected, the patient
is imperative in the treatment of complicated
should immediately be referred to a surgical
odontogenic infections (Table 2).71,101,102
specialist for evaluation and management.
The specialist will collect a sample of the
Based on best available evidence, penicillin V
purulent exudate, usually by aspiration, for
potassium or amoxicillin formulations, alone or in
culture and susceptibility testing and begin
combination with metronidazole; and clindamycin
immediate empirical intravenous antibacterial
are reasonable empirical options to consider
chemotherapy.96 Drainage is established at the
for the treatment of complicated odontogenic
earliest possible time and measures to protect
infections (Figure 10).10,42,71 Azithromycin may be
the airway are instituted if necessary. Close
an empirical option in some instances. Ultimately,
monitoring and modification of antibacterial
the empirical drug of choice should be an effective
chemotherapy, if indicated, is imperative.
agent with the narrowest spectrum and the least
potential for adverse drug effects.
Adjunctive Antibacterial Chemotherapy
Routine antibacterial chemotherapy for the
Primary Line of Antibacterial Chemotherapy
treatment of uncomplicated odontogenic
Unless the patient has an allergy to the
infections, in the absence of timely debridement,
penicillins, the empirical drug of first choice for
i.e., primary dental care, has not been shown
the treatment of odontogenic infections is narrow
to be effective.10,16,17,20,71,80-87,89-92,95-99 Consequently,
spectrum penicillin V potassium (Table 3).9,16,42
clinicians should avoid "rational activism" and
Most infections require 5 days of antibacterial
"reflex prescribing". The rational activist assumes
chemotherapy. An initial loading dose is followed
that it is better to over-treat than not to treat at
by maintenance doses for the remainder of the
all; the reflex prescriber caters to the patient's
time. It is prudent to schedule the patient for
expectations regardless of the diagnosis.
a follow-up in 2 to 3 days. This will provide an
opportunity to assess response to treatment.
Uncomplicated odontogenic infections that
Hypersensitivity reactions are potentially the most
have not been debrided in a timely manner
serious adverse drug effects (see the Prescription-
or have failed to respond to debridement may
precautions Associated with the Administration of
spread, especially in immunocompromised
Antibacterial Agents section).103
Figure 10. Percent antibacterial susceptibility of 98 strains of oral bacteria.
Based on data from Baumgartner JC, Xia T. Antibiotic susceptibility of bacteria associated with endodontic abscesses.
J Endod 2002;29(1):44-47.42
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
Table 2. Principles of adjunctive antibacterial chemotherapy.
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
Table 3. Empirical antibacterial agents for the treatment of complicated odontogenic infections.
If significant improvement is not noted in 48
azithromycin in the treatment of odontogenic
to 72 hours, the empirical addition (for 5 days)
infections, among macrolides it may be the best
of metronidazole to penicillin V potassium
alternative because of its extended spectrum
is reasonable. Metronidazole is β-lactamase
against facultative and some obligate anaerobes
resistant and it provides excellent coverage for
(Table 3).75,76 However, a recent FDA drug
obligate anaerobes (Table 3).61,104,105 The safety
safety communication warns about the risk of
and effectiveness of metronidazole in pediatric
QT prolongation and cardiac arrhythmias (see
patients have not been established. In patients
the Prescription-precautions Associated with the
receiving metronidazole, the concurrent use of
Administration of Antibacterial Agents section).106
alcohol may produce severe gastrointestinal
symptoms; serious convulsive seizures and
It is also of note, that the single most important
peripheral neuropathy have also been reported
driver of the emergence of macrolide resistance
(see the Prescription-precautions Associated with
in vivo is macrolide use.107 Macrolide-resistant
the Administration of Antibacterial Agents section).
organisms can block ribosomal macrolide-
receptor sites, and because of receptor-site
Secondary Line of Antibacterial Chemotherapy
overlap, these organisms will also be resistant
A macrolide is an empirical option for the
to clindamycin; and efflux pump-related
treatment of odontogenic infections in patients
macrolide-resistance also affects the intracellular
allergic to β-lactam antibiotics. While there is
concentration of β-lactam antibiotics and
a paucity of data demonstrating the efficacy of
β-lactamase inhibitor, i.e., macrolide-resistance
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
often confers multidrug-resistance. Clindamycin
Consequently, antibacterial agents given to
may also be an empirical option (see below).108
healthy people in association with third molar
extractions to prevent infection may cause more
Tertiary Line of Antibacterial Chemotherapy
harm than benefit, both to patients and the
Clindamycin is the empirical drug of choice for
community at large.118
unresolved infections following treatment with
a β-lactam antibacterial agent.71,109 It is also the
Prevention of Surgical-site Infection in
initial empirical drug of choice for the treatment
Patients Undergoing Placement of Dental
of severe complicated odontogenic infections
(Table 3).20,47,48,110,111 It is β-lactamase resistant
Bacteria introduced during the placement of
and has excellent activity against gram-positive
dental implants can lead to infection and implant
cocci and most gram-negative anaerobes.45,47,111-115
failure. A critical review of the literature identified
However, the risk of Clostridium difficile-
four randomized controlled clinical trials, with a
associated superinfections, which may range in
follow up of at least 3 months, comparing the
severity from mild diarrhea to fatal colitis, should
efficacy of various prophylactic antibacterial
prompt caution and mandates close follow-up
regiments versus no antibiotics in patients
(see the Prescription-precautions Associated
undergoing dental implant placement.119 The
with the Administration of Antibacterial Agents
implant failure rate among patients not receiving
antibiotics was 5%.119
There is some evidence to suggest that
A significant percentage of antibacterial agents
amoxicillin 2g administered 1 hour preoperatively
are putatively prescribed by dental practitioners
significantly reduces the failure rate of dental
for the prevention of infection. In general, when
implants placed under ordinary conditions.119
an effective antibacterial agent is used to prevent
The number needed to treat (NNT) to prevent
infection by specific bacteria or to eradicate them
one individual from having an implant failure is
immediately or soon after they have become
33. No significant adverse drug effects were
established, the strategy is frequently successful.
reported, although the issue of antibacterial
However, prophylactic antibacterial chemotherapy
drug resistance was not addressed. There is no
in dentistry should be limited to the prevention
evidence that postoperative antibacterial agents
of those infections that are proven or strongly
are beneficial.119
suspected to be procedure-specific.
Prevention of Infective Endocarditis in
Prevention of Surgical-site Infection in
Patients Undergoing Dental Procedures
Patients Undergoing Tooth Extractions
The American Heart Association (AHA) publishes
Tooth extraction is the indicated therapy for
a clinical practice guideline, with periodic updates,
teeth deemed non-restorable. However, there
for the prevention of infective endocarditis in
is no evidence to support the prophylactic use
patients undergoing dental procedures.120 The
of antibacterial agents in association with the
2007 guideline stratifies cardiac conditions as
extraction of non-restorable teeth.118 Another
to the risk of developing endocarditis and the
common reason for tooth extraction is poorly
severity of associated morbidity. Only patients
aligned or impacted third molars. The infection
with the highest-risk of adverse outcome from
rate after third molar extraction is about 10%.118
endocarditis (Table 4) should be considered for
In debilitated or immunocompromised patients,
antibacterial prophylaxis prior to invasive dental
the infection rate may be as high as 25%.118
procedures (Table 5).120
Antibacterial drugs administered just before and/
In situations where no chemoprophylaxis
or just after third molar extractions do reduce the
was given, but in which unexpected bleeding
risk of infection, pain, and dry socket, but there
occurred, the institution of antibacterial therapy
is no evidence that antibacterial agents reduce
within 2 hours is recommended. Patients at
fever, swelling, or trismus. The practice also
risk already taking an antibacterial agent should
contributes to adverse drug effects, including
be prescribed one of the drugs from a different
the likelihood of bacterial drug resistance.
class recommended for chemoprophylaxis.
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
Table 4. Conditions associated with the highest risk of adverse outcome from endocarditis for
which antibacterial prophylaxis is reasonable.120
Table 5. Antibacterial prophylaxis before procedures that involve manipulation of gingival tissue,
periapical region of teeth, or perforation of the oral mucosa.120
Clinicians should allow at least 9-14 days
2003 guideline was prescriptive, patients with
between appointments to reduce the risk for the
one or more high-risk conditions were considered
development of resistant organisms.
candidates for antimicrobial prophylaxis in
association with invasive dental procedures.122
Prevention of Orthopaedic Implant Infection in
Patients Undergoing Dental Procedures
The 2012 AAOS-ADA Clinical Practice Guideline,
The American Academy of Orthopedic Surgeons
which was developed using a systematic
(AAOS) in cooperation with the American
evidence-based process, replaces all previous
Dental Association (ADA) publishes a clinical
advisory or information statements.121 It provides
practice guideline, with periodic updates, for the
no specific direction in managing individual
prevention of orthopaedic implant infection in
patients (Table 6).121 Until scientific prospective
patients undergoing dental procedures.121 The
data becomes available, the development of
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
Table 6. Recommendations of the 2012 AAOS-ADA clinical practice guideline.121
therapeutic and preventive strategies for each
the efficacy of post-operative prophylactic
patient should be based on dialogue between oral
antibacterial chemotherapy in association with
healthcare provider, physician, and patient.121
open reduction and internal fixation of mandibular
fractures and found no statistically significant
Prevention of Infection in Patients with
benefit.129 However, investigators concluded that
Various Medical Conditions Undergoing Dental
tobacco and alcohol appear to be significant risk
factors for post-operative infections.
A number of systemic conditions, e.g., neutropenia,
asplenia, diabetes mellitus, end-stage renal
Prevention of Surgical-site Infection in Patients
disease, immunosuppression, systemic lupus
Undergoing Head and Neck Oncology Surgery
erythematosus, and others are commonly cited as
The incidence of wound infection in patients
conditions that predispose a patient to bacteremia-
undergoing head and neck oncology surgery
induced infections. Evidence that a particular
has been reported to be as high as 87%, often
bacteremia-producing dental procedure caused a
with devastating consequences.130 Based on the
specific case of infection is circumstantial at best
best current evidence, it is recommended that
and no definitive, scientific evidence supports the
prophylactic antibacterial agents, covering aerobic
use of prophylactic antibiotics.123-125
gram-positive cocci and gram-negative bacilli, and
anaerobic bacteria be administered in association
Most importantly, clinicians should amplify their
with clean and clean-contaminated head and neck
efforts to ensure that all patients understand
oncology surgery.130 There is no evidence that
the critical importance of maintaining optimal
prophylactic antibacterial agents offer any benefit
oral health, which could serve to reduce the
in clean surgery for benign disease.
severity of both self-induced and treatment-
induced bacteremia. In the absence of evidence
Prescription-precautions Associated with
or consensus on the issue, oral healthcare
providers should weigh the benefits of antibacterial There are no "absolutely" safe biologically active
prophylaxis against the risks of ADEs, including the therapeutic agents, i.e., drugs seldom exert
development of drug resistance.
their beneficial effects without also causing
adverse drug events (ADEs). The penicillins,
Prevention of Surgical-site Infection in Patients metronidazole, azithromycin, and clindamycin,
Undergoing Open Reduction and Fixation of
like other drugs, even after the administration of a
single dose, can produce ADEs.
The benefit of pre- and intra-operative antibacterial
chemotherapy when treating open mandibular
fractures has long been established.126-128 More
The widespread and ever increasing use of
recently, a prospective randomized trial evaluated
antibacterial agents contributes to the development
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
of antibacterial drug-resistance.102,107,131-143 Unless
medications for the treatment of abnormal heart
healthcare providers change their practices,
rhythm or arrhythmias. Increased risk of death
many currently available antibacterial agents may
from cardiovascular causes has been reported
become ineffective. When antibacterial agents
in persons treated with a 5-day course of
are used appropriately to treat complicated
odontogenic infections or to prevent infections
in high-risk patients, clinicians must accept
Central Nervous System Effects
the ecological consequences of antibacterial
Metronidazole should be administered with
chemotherapy. However, when other therapeutic
caution to patients with central nervous system
means are available, antibacterial agents should
disorders. Severe convulsive seizures and
not be routinely prescribed to treat or to prevent
peripheral neuropathy, characterized by
numbness or paresthesia of the extremities, have
been reported.61 Infrequently, neuropathy has
been noted with penicillin formulations, but when
Common ADEs associated with antibacterial
present, it is usually associated with high doses
agents, but especially with macrolides, are
of parenteral penicillin.38,39
nausea, vomiting, epigastric distress, and
diarrhea.38,39,61,70,73 These symptoms may be
amplified in patients on metronidazole with
Superinfections with Candida sp. can occur
concurrent use of alcohol.70 When a patient has
in association with all, but especially broad-
been taking an antibacterial agent for 1 to 2 days,
spectrum antibacterial agents.38,39,61,70,73 Acute
diarrhea is probably due to the mild irritating
pseudomembranous oral candidiasis appears
action of the drug; however, bloody diarrhea
as white, raised, or cottage cheese-like that
with abdominal cramping is highly suggestive of
can be scraped off, leaving a red, sometimes
pseudomembranous colitis, a superinfection with
hemorrhagic base. Patients may also present
Clostridium difficile.117 Colitis has been reported
with hairy tongue and complain of burning,
with the use of nearly all antibacterial agents, but
itching, or a metallic taste. Candidiasis
especially with clindamycin.38,39,61,70,73
occurring in a patient with a dry mouth may
present as areas of patchy erythema with little
or no evidence of cottage cheese-like curds.
Hypersensitivity reactions, characterized by
Candida sp. may spread to the esophagus or
maculopapular to exfoliative dermatitis, urticaria,
lungs via swallowing or droplet aspiration; or
angioedema, and rarely, anaphylaxis may occur
systemically via the blood stream, especially in
with all antibacterial agents, but especially with
the β-lactams.103,38,39,61,70,73 Allergic reaction to the
penicillins is more likely to occur in individuals
Antibacterial Drugs and Pregnancy
with sensitivity to multiple allergens and in those
There is no firm evidence that the penicillins,
with asthma; and patients with a history of allergy
metronidazole, azithromycin, and clindamycin
to the penicillins have experienced allergic
are teratogenic in humans; however, drugs in
reactions when treated with cephalosporins.
general should be prescribed with caution during
Rare instances of erythema multiforme and
pregnancy. To assist practitioners in prescribing
Stevens-Johnson syndrome have been reported
drugs for the pregnant patient, the Food and Drug
with clindamycin and azithromycin.70,73
Administration (FDA) has established a code for
categorizing drugs according to their potential to
cause fetal injury.145
Azithromycin and other macrolides can cause
abnormal electrical activity in the heart that
The penicillins, metronidazole, azithromycin, and
may lead to a potentially fatal irregular heart
clindamycin all have an FDA Pregnancy Category
rhythm.73,106 Patients at particular risk for
B rating, i.e., animal studies have revealed no
developing this condition include those with
evidence of harm to the fetus; however, there
known risk factors such as existing QT interval
are no adequate and well-controlled studies in
prolongation, bradycardia, and those taking
pregnant women.38,39,61,70,73,145 Since animal studies
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
are not always predictive of a drug's teratogenic
However, the theoretical possibility that
effect in humans, antibacterial agents should
antibacterial agents may reduce the efficacy of
only be prescribed during pregnancy if clearly
oral contraceptives must be addressed directly.
An exhaustive review of the literature found no
credible pharmacokinetic data, with the possible
Antibacterial Drugs and Nursing
exception of rifampin, to substantiate such
Mechanisms of drug excretion in human milk
interactions.150 The U.S. District Court for the
include both passive diffusion and carrier-
Northern District of California also concluded
mediated transport. The amount of drug
that "scientific evidence regarding the alleged
excreted in milk depends on the drug's molecular
interaction between antibacterial agents and oral
weight, lipid solubility, pKa, and plasma
contraceptives" does not satisfy the "Daubert
protein binding.146,147 Once in milk, the pKa of
standard of causality."151
the drug is an important determinant of the
drug's concentration in milk. Consequently, at
However, the American Medical Association
equilibrium some drugs may accumulate in milk in
states that such interactions cannot be completely
higher concentration relative to plasma.
discounted and recommends that women be
informed of the possibility of such interactions.152
The penicillins are excreted in milk and may lead
Similarly, the American Dental Association Council
to sensitization of infants.38,39 Metronidazole,
on Scientific Affairs recommends (1) that patients
which has been shown to be carcinogenic in rats
be advised of the potential risk, (2) that patients
and mice, is excreted in milk in concentrations
comply with their oral contraceptive regimen, and
similar to those found in plasma.61 Clindamycin is
(3) that patients consider alternative contraception
also excreted in milk.70 The fate of azithromycin
during periods of antibacterial chemotherapy.153,154
is unknown.73 Considering the potential risks to
the nursing infant and benefits to the mother, a
decision should be made whether to discontinue
The routine use of antibacterial agents in the
nursing or not to prescribe an antibacterial
treatment of uncomplicated odontogenic infections
has not been shown to be effective. Most such
infections respond to timely debridement. When
treating complicated odontogenic infections, the
Two or more drugs administered in therapeutic
adjunctive use of antibacterial agents is justified.
dosages at the same time or in close sequence,
The empirical drug of choice should be the most
may act (1) independently, (2) interact to
effective and least toxic agent with the narrowest
increase or diminish the effect of one or more
spectrum. Prophylactic antibacterial chemotherapy
drugs, or (3) interact to cause an unintended
in dentistry should be limited to the prevention
reaction. Potentially serious interactions can
of those infections that have been proven or are
occur between antibacterial agents and other
strongly suspected to be procedure-specific. It is
medications. An awareness of the patient's
axiomatic that before prescribing an antibacterial
medical history, including medications taken, is
agent, the clinician must consider the diagnosis,
helpful in minimizing or avoiding potential drug-
the need for drug therapy, and the benefits versus
drug interactions. Two excellent reviews of the
risks of treatment.
subject are presented elsewhere.148,149
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
Course Test Preview
To receive Continuing Education credit for this course, you must complete the online test. Please go to:
1. Invasion and multiplication of bacteria in body tissues result in local cellular injury due to
a. competitive metabolism
b. toxin production
c. immune-mediated reactions
d. All of the above.
2. Which of the following statements is correct with respect to Gram-positive and Gram-
a. Acetone extracts lipids from the outer membrane, cell wall, and cytoplasmic membrane of bacteria.
b. The damage to gram-negative organisms is more extensive and they lose their crystal violet-iodine
complexes, i.e., they are decolorized; and when counterstained with safranin, they appear red.
c. Gram-positive bacteria retain their crystal violet-iodine complexes and appear deep purple.
d. All of the above.
3. All of the following statements is correct with respect to odontogenic infections EXCEPT
which one?
a. Most odontogenic infections are polymicrobial.
b. The predominant flora create an ecosystem of synergism by elaborating a more favorable alkaline
environment and increased oxygenation to support the growth and proliferation of its members.
c. In odontogenic infections, the number of isolated strains ranges from 1 to 10 organisms.
d. The average number of organisms responsible for an odontogenic infection is 4.
4. Pharmacological strategies are predicated on targeting differences between prokaryotic
bacterial and eukaryotic host cells. Selective toxicity can be achieved by _.
a. attacking targets unique to bacteria
b. attacking targets in bacteria similar but not identical to those in host cells
c. attacking targets that are shared, but vary in importance between bacteria and host cells
d. All of the above.
5. Which of the following statements is correct with respect to bacterial cell walls?
a. Monomers are synthesized in the cytoplasm from amino acid and sugar building blocks.
b. Bactoperol transfers the monomers across the cytoplasmic membrane where they are polymerized
into linear peptidoglycan chains.
c. Transpeptidase cross-links peptidoglycan chains into a three-dimensional mat.
d. All of the above.
6. All of the following statements are correct with respect to inhibitors of cell wall synthesis
EXCEPT which one?
a. Vancomycin targets monomer polymerization, it is bactericidal, but does not have the requisite
spectrum to be considered an empirical option in treating odontogenic infections.
b. Penicillin V potassium and amoxicillin formulations, which block polymer cross-linking, are
bactericidal, and have the requisite spectra to be considered as empirical options in treating
c. Second generation cephalosporins have an overlapping spectra with those of penicillin V potassium
and amoxicillin formulations.
d. 2nd generation cephalosporins are more β-lactamase resistant and offer a significant therapeutic
advantage over the penicillins as empirical options.
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
7. Which of the following statements relative to inhibitors of DNA synthesis and integrity is
a. Fluoroquinolones block topoisomerase type II activity, disrupt the integrity of bacterial DNA, and are
b. Sulfamethoxazole (SMX) and trimethoprim (TMP), block succeeding steps in folate synthesis and the
combination is bactericidal.
c. A metabolite of metronidazole directly binds DNA, causes loss of its helical structure, effect strand
breakage, and is bactericidal.
d. Metronidazole, in combination with penicillin V potassium or amoxicillin, is an empirical option in
treating odontogenic infections.
8. Which of the following statements is correct with respect to inhibitors of transcription and
a. Tetracyclines are teratogenic and produce higher rates of neuronal-tube defect, cleft palate, and
multiple congenital abnormalities.
b. Clindamycin has excellent activity against gram-positive aerobes and anaerobes, as well as gram-
negative anaerobes.
c. Azithromycin has an extended spectrum that includes some anaerobic gram-positive cocci and gram-
negative bacilli.
d. All of the above.
9. Uncomplicated odontogenic infections manifest primarily as caries; and pulpal, periodontal,
and pericoronal problems with signs and symptoms that include pain, erythema, edema,
and difficulty chewing.
10. Complicated odontogenic infections reflect the extension of an uncomplicated odontogenic
infection into surrounding tissue with Signs and symptoms that include lymphadenitis,
trismus, difficulty swallowing or breathing; and less frequently, fever and hypotension.
11. Which of the following statements about the routine use of antibacterial agents in the
treatment of uncomplicated infections is correct?
a. Reversible pulpitis is a reactive process and there is no evidence that antibacterial agents would
have any effect on clinical outcome.
b. In untreated irreversible pulpitis, penicillin does not reduce spontaneous pain, percussion induced
pain, or the intake of analgesics.
c. In the treatment of acute apical periodontitis, once the source of infection is eliminated, the
administration of penicillin provides no added benefit.
d. All of the above.
12. In a prospective study, a five-day course of penicillin administered to patients with acute
pain related to a tooth with an amalgam restoration without clinical signs of infection, in
the absence of definitive dental care, did not prevent the emergence of clinical signs of
infection within 5 days.
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
13. In a prospective study, a five-day course of penicillin administered to patients with acute
pain related to a tooth with large periapical radiolucency, but without clinical signs of
infection, in the absence of debridement did not prevent the development of clinical signs
of infection within 5 days.
14. In the treatment of draining sinus tract, there is convincing evidence that the routine
administration of an antibacterial agent improves therapeutic outcome.
15. There is convincing evidence that the routine administration of an antibacterial agent
improves therapeutic outcome in association with which of the following conditions?
a. Gingival and periodontal abscesses
b. Necrotizing ulcerative gingivitis
c. Alveolar osteitis
d. None of the above.
16. Depending on pericoronitis-associated signs and symptoms, i.e., clinical evidence of
induration as the infection is spreading buccally or lingually and the presence of trismus,
the adjunctive antibacterial therapy may be appropriate.
17. Which of the following conditions should be considered a complicated odontogenic
infection and an indication for adjunctive antibacterial chemotherapy?
c. Space infections
d. All of the above.
18. Based on best available evidence, penicillin V potassium or amoxicillin formulations, alone
or in combination with metronidazole; and clindamycin are reasonable empirical options to
consider for the treatment of complicated odontogenic infections.
19. The empirical antibacterial agent drug of choice should be an effective agent with the
narrowest spectrum and the least potential for adverse drug effects.
20. Which of the following statements is correct with respect to primary line antibacterial
a. Unless the patient has an allergy to the penicillins, the empirical drug of first choice for the treatment
of odontogenic infections is narrow spectrum penicillin V potassium.
b. Most infections require 5 days of antibacterial chemotherapy - an initial loading dose followed by
maintenance doses for the remainder of the time.
c. If significant improvement is not noted in 48 to 72 hours, the addition (for 5 days) of metronidazole to
penicillin V potassium is reasonable.
d. All of the above.
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
21. Which of the following statements is correct with respect to secondary line antibacterial
a. A macrolide is an empirical option for the treatment of odontogenic infections in patients allergic to
b. While there is a paucity of data demonstrating the efficacy of azithromycin in the treatment of
c. Clindamycin may be a better empirical option in patients allergic to β-lactam antibacterial agents.
d. All of the above.
22. Which of the following statements is correct with respect to tertiary line antibacterial
a. Clindamycin is the empirical drug of choice for unresolved infections following treatment with a
β-lactam antibacterial agent.
b. Clindamycin is the initial empirical drug of choice for the treatment of severe complicated
c. Clindamycin is β-lactamase resistant and has excellent activity against gram-positive cocci and most
d. All of the above.
23. All of the following statements are correct with respect to the prevention of surgical-site
infection in patients undergoing tooth extractions EXCEPT which one?
a. There is no evidence to support the prophylactic use of antibacterial agents in association with the
extraction of non-restorable teeth.
b. The infection rate after third molar extraction is about 10%.
c. In debilitated or immunocompromised patients, the infection rate after third molar extraction may be
as high as 25%.
d. Antibacterial drugs administered just before and/or just after third molar extractions do reduce the
risk of infection, pain, and dry socket.
e. There is solid evidence that an antibacterial agent given to healthy people in association with third
molar extractions is more beneficial than harmful.
24. All of the following statements are correct with respect to the prevention of surgical-site
infection in patients undergoing placement of dental implants EXCEPT which one?
a. Bacteria introduced during the placement of dental implants can lead to infection and implant failure.
b. The implant failure rate among patients not receiving antibiotics is about 5%.
c. There is no evidence to suggest that amoxicillin 2g. administered 1 hour preoperatively significantly
reduces the failure rate of dental implants placed under ordinary conditions.
d. There is no evidence that postoperative antibacterial agents are beneficial to reduce infection and
implant failure.
25. All of the following statements are correct with respect to the prevention of infective
endocarditis in patients undergoing dental procedures EXCEPT which one?
a. The 2007 guideline stratifies cardiac conditions as to the risk of developing endocarditis and the
severity of associated morbidity.
b. Only patients with the highest-risk of adverse outcome from endocarditis require antibacterial
prophylaxis prior to dental procedures.
c. Antibacterial prophylaxis is indicated before procedures that involve manipulation of gingival tissue,
periapical region of teeth, or perforation of the oral mucosa.
d. In situations where no chemoprophylaxis was given, but in which unexpected bleeding occurred, the
institution of antibacterial therapy within 24 hours is recommended.
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
26. Which of the following statements is correct with respect to the prevention of orthopaedic
implant infection in patients undergoing dental procedures?
a. The practitioner might consider discontinuing the practice of routinely prescribing prophylactic
antibiotics for patients with hip and knee prosthetic joint implants undergoing dental procedures.
b. There is no evidence to recommend for or against the use of topical oral antimicrobials in patients
with prosthetic joint implants or other orthopaedic implants undergoing dental procedures.
c. In the absence of reliable evidence linking poor oral health to prosthetic joint infection, it is the
consensus that patients with prosthetic joint implants or other orthopaedic implants maintain
appropriate oral hygiene.
d. All of the above.
27. Which of the following statements is correct with respect to the prevention of infection in
patients with various medical conditions undergoing dental procedures?
a. Evidence that a particular bacteremia-producing dental procedure caused a specific case of infection
is circumstantial at best.
b. No definitive, scientific evidence supports the use of prophylactic antibiotics in patients with various
medical conditions undergoing dental procedures.
c. Clinicians should amplify their efforts to ensure that all patients understand the critical importance
of maintaining optimal oral health, which could serve to reduce the severity of both self-induced and
d. All of the above.
28. Which of the following statements is correct with respect to the prevention of surgical-site
infection in patients undergoing open reduction and fixation of mandibular fractures?
a. The benefit of pre- and intra-operative antibacterial chemotherapy when treating open mandibular
fractures has long been established.
b. A prospective randomized trial evaluated the efficacy of post-operative prophylactic antibacterial
chemotherapy in association with open reduction and internal fixation of mandibular fractures and
found no statistically significant benefit.
c. A prospective randomized trial evaluated the efficacy of post-operative prophylactic antibacterial
chemotherapy in association with open reduction and internal fixation of mandibular fractures
concluded that tobacco and alcohol appear to be significant risk factors for post-operative infections.
d. All of the above.
29. Which of the following statements is correct with respect to the prevention of surgical-site
infection in patients undergoing head and neck oncology surgery?
a. The incidence of wound infection in patients undergoing head and neck oncology surgery has been
reported to be as high as 87%, often with devastating effect.
b. Based on the best current evidence, it is recommended that prophylactic antibacterial agents,
covering aerobic gram-positive cocci and gram-negative bacilli, and anaerobic bacteria be
administered in association with clean and clean-contaminated head and neck oncology surgery.
c. There is no evidence that prophylactic antibacterial agents offer any benefit in clean surgery for
benign disease.
d. All of the above.
30. Which of the following statements is correct with respect to antibacterial drug-resistance?
a. The widespread and ever increasing use of antibacterial agents contributes to the development of
b. Unless healthcare providers change their practices, many currently available antibacterial agents
may become ineffective.
c. When other therapeutic means are available, antibacterial agents should not be routinely prescribed
to treat or to prevent infections.
d. All of the above.
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
31. All of the following statements are correct with respect to gastrointestinal disturbances in
association with antibacterial agents EXCEPT which one?
a. Common ADEs associated with antibacterial agents, but especially with macrolides, are nausea,
vomiting, epigastric distress, and diarrhea.
b. Gastrointestinal symptoms may be amplified in patients on clindamycin with concurrent use of alcohol.
c. When a patient has been taking an antibacterial agent for 1 to 2 days, diarrhea is probably due to the
mild irritating action of the drug.
d. Bloody diarrhea with abdominal cramping is highly suggestive of pseudomembranous colitis, a
superinfection with Clostridium difficile.
32. Which of the following statements is correct with respect to hypersensitivity or other
immune-related reactions to antibacterial agents?
a. Maculopapular to exfoliative dermatitis, urticaria, angioedema, and rarely, anaphylaxis may occur with
all antibacterial agents.
b. Allergic reaction to the penicillins is more likely to occur in individuals with sensitivity to multiple
allergens and in those with asthma.
c. Rare instances of erythema multiforme and Stevens-Johnson syndrome have been reported with
clindamycin and azithromycin.
d. All of the above.
33. Which of the following statements is correct with respect to potential cardiac complications
associated with macrolides antibacterial agents?
a. Azithromycin and other macrolides can cause abnormal electrical activity in the heart that may lead to
a potentially fatal irregular heart rhythm.
b. Patients at particular risk for developing cardiac complications include those with existing QT internal
prolongation and bradycardia; and those taking medications for the treatment of abnormal heart
rhythm or arrhythmias.
c. Increased risk of death from cardiovascular causes has been reported in persons treated with a 5-day
course of azithromycin.
d. All of the above.
34. Penicillins should be administered with caution to patients with central nervous system
disorders because severe convulsive seizures and peripheral neuropathy, characterized by
numbness or paresthesia of the extremities are common.
35. Superinfections with Candida sp. can occur in association with all, but especially broad-
spectrum antibacterial agents.
36. Which of the following statements is correct with respect to antibacterial agents and
a. There is no firm evidence that the penicillins, metronidazole, azithromycin, and clindamycin are
teratogenic in humans.
b. The penicillins, metronidazole, azithromycin, and clindamycin all have an FDA Pregnancy Category
B rating, i.e., animal studies have revealed no evidence of harm to the fetus; however, there are no
adequate and well-controlled studies in pregnant women.
c. Since animal studies are not always predictive of a drug's teratogenic effect in humans, antibacterial
agents should only be prescribed during pregnancy if clearly indicated.
d. All of the above.
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
37. Which of the following statements is correct with respect to antibacterial agents and nursing?
a. The penicillins are excreted in milk and may lead to sensitization of infants.
b. Metronidazole, which has been shown to be carcinogenic in rats and mice, is excreted in milk in
concentrations similar to those found in plasma.
c. Considering the potential risks to the nursing infant, a decision should be made whether to discontinue
nursing or not to prescribe an antibacterial agent to the mother.
d. All of the above.
38. Which of the following statements are correct in relation to interactions between antibacterial
agents and oral contraceptives EXCEPT which one?
a. There are no pharmacokinetic data at this time to support the contention that antibacterial agents
reduce the efficacy of oral contraceptives, except for rifampin, an antituberculin drug.
b. The United States District Court for the Northern District of California concluded that "scientific
evidence regarding alleged interaction between antibacterial agents and oral contraceptives did not
satisfy the "Daubert" standard of causality.
c. According to the American Medical Association, such interactions cannot be completely discounted.
d. All of the above.
39. The ADA recommends that patients prescribed an antibacterial agent while also taking an oral
a. be advised of the potential risk
b. comply with their oral contraceptive regimen
c. consider alternative contraception during periods of antibacterial chemotherapy
d. All of the above.
40. All of the following statements are correct with respect to the administration of antibacterial
agents in oral healthcare settings EXCEPT which one?
a. The routine use of antibacterial agents in the treatment of uncomplicated odontogenic infections has
not been shown to be effective.
b. When treating complicated odontogenic infections, the adjunctive use of antibacterial agents is
c. Prophylactic antibacterial chemotherapy in dentistry should be limited to the prevention of those
infections that have been proven or are strongly suspected to be procedure-specific.
d. The empirical drug of choice should be the most effective and least toxic agent with the broadest
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
1. Hallman M. The surfactant system protects both fetus and newborn. Neonatology. 2013;103(4):
2. Lederberg J. Infectious history. Science. 2000 Apr 14;288(5464):287-293.
3. Darveau RP, McFall-Ngai M, Ruby E, Miller S, Mangan DF. Host tissues may actively respond to
beneficial microbes. ASM News 2003;69(4):186-191.
4. Brito LC, Sobrinho AP, Teles RP, Socransky SS, Haffajee AD, Vieira LQ, Teles FR. Microbiologic
profile of endodontic infections from HIV+ and HIV- patients using multiple-displacement amplification
and checkerboard DNA-DNA hybridization. Oral Dis. 2012 Sep;18(6):558-567.
5. Uzel NG, Teles FR Song XQ, Torresyap G, Socransky SS, Haffajee AD. Microbial shifts during dental
biofilm re-development in the absence of oral hygiene in periodontal health and disease. J Clin
Periodontol. 2011 Jul; 38(7):612-620.
6. Haug RH. Microorganisms of the nose and paranasal sinuses. Oral Maxillofac Surg Clin North Am.
7. McClelland R. Gram's stain: The key to microbiology. Medical Laboratory Observer. 2001;33(4):20-28.
8. Kasmar AG, Hooper D. Pharmacology of bacterial infections: cell wall synthesis. In Golan DE,
Tashjian, Jr. AH, Armstrong EJ, Armstrong AW. Ed. Principles of pharmacology. The pathophysiologic
basis of drug therapy. 2nd ed. 2008. Wolters Kluwer/Lippincott Williams & Wilkins. Baltimore, MD.
9. Kuriyama T. Karasawa T. Nakagawa K. Saiki Y. Yamamoto E. Nakamura S. Bacteriologic features and
antimicrobial susceptibility in isolates from orofacial odontogenic infections. Oral Surg Oral Med Oral
10. Warnke PH1, Becker ST, Springer IN, Haerle F, Ullmann U, et al., Penicillin compared with other
advanced broad spectrum antibiotics regarding antibacterial activity against oral pathogens isolated
from odontogenic abscesses. J Craniomaxillofac Surg. 2008 Dec;36(8):462-467.
11. Pennisi E. A mouthful of microbes. Science. 2005 Mar 25;307(5717):1899-1901.
12. Greenberg RN, James RB, Marier RL, et al. Microbiologic and antibiotic aspects of infections in the
oral and maxillofacial region. J Oral Surg 1979;37:873-884.
13. Kannangara DW, Thadepalli H, McQuirter JL. Bacteriology and treatment of dental infections. Oral
Surg Oral Med Oral Pathol 1980;50:103-109.
14. Von Konow L, Nord CE, Nordenram A. Anaerobic bacteria in dentoalveolar infections. Int J Oral Surg
15. Gill Y, Scully C. Orofacial odontogenic infections: review of microbiology and current treatment. Oral
Surg Oral Med Oral Pathol 1990;70:155-158.
16. Sandor GK, Low DE, Judd PL, Davidson RJ. Antimicrobial treatment options in the management of
odontogenic infections. J Can Dent Assoc 1998;64;508-514.
17. Baker KA, Fotos PG. The management of odontogenic infections: a rational for appropriate
chemotherapy. Dent Clin North Am 1994;38:689-706.
18. Moenning JE, Nelson CL, Koehler RB. The microbiology and chemotherapy of odontogenic infections.
J Oral Maxillofac Surg 1989;47:976-985.
19. Newman MG. Anaerobic oral and dental infection Rev Infect Dis. 1984 Mar-Apr;6 Suppl 1:S107-114.
20. Heimdahl A, von Konow L, Satoh T, Nord CE. Clinical appearance of orofacial infections of
odontogenic origin in relation to microbiological findings. J Clin Microbiol. 1985 Aug;22(2):299-302.
21. Könönen E1, Nyfors S, Mättö J, Asikainen S, Jousimies-Somer H. Beta-lactamase production by
oral pigmented Prevotella species isolated from young children. Clin Infect Dis. 1997 Sep;25 Suppl
22. van Winkelhoff AJ, Winkel EG, Barendregt D, Dellemijn-Kippuw N, Stijne A, van der Velden U. J Clin
23. Sands T, Pynn BR, Katsikeris N. Odontogenic infections: Microbiology, antibiotics, and management.
Oral Health 1995;85:11-28.
24. Williams R. Periodontal disease. N Eng J Med 1990;322:373-382.
25. Barclay JK. Antibiotics revisited. N Z Dent J. 1990;86:44-47.
26. Loesche WJ. The antibacterial treatment of periodontal disease: changing the treatment paradigm.
Crit Rev Oral Biol Med 1999;10(3):245-275.
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
27. Baumgartner JC. Microbiologic aspects of endodontic infections. J Calif Dent Assoc 2004;32(6):
28. Tomazinho LF, Avila-Campos MJ. Detection of Porphyromonas gingivalis, Porphyromonas
endodentalis, Prevotella intermedia, and Prevotella nigrescens in chronic endodontic infection. Oral
Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103(2):285-288.
29. Patel M, Chettiar TP, Wadee AA. Isolation of Staphylococcus aureus and black-pigmented
Bacteroides indicate a high risk for the development of Ludwig's angina. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod 2009;108(5):667-672.
30. Siqueira HF, Racos IN, Alves FRF, Silva MG. Bacteria in the apical canal of teeth with primary apical
periodontitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107(5):721-726.
31. Avila M, Ojcius DM, Yilmaz O. The Oral Microbiota: Living with a Permanent Guest. DNA Cell Bio.
32. Harbison H, Rose HS, Coen DM, Golan DE. Principles of antibacterial and antineoplastic
pharmacology. In Golan DE, Tashjian, Jr. AH, Armstrong EJ, Armstrong AW. Ed. Principles of
pharmacology. The pathophysiologic basis of drug therapy. 2nd ed. 2008. Wolters Kluwer/Lippincott
Williams & Wilkins. Baltimore, MD.
33. Wilhelm MP, Estes L. Vancomycin. Mayo Clin Proc. 1999 Sep;74(9):928-935.
34. Wright AJ. The penicillins. Mayo Clin Proc. 1999 Mar;74(3):290-307.
35. Marshall WF, Blair JE. The cephalosporins. Mayo Clin Proc. 1999;74:187-195.
36. Vancomycin hydrochloride (vancomycin hydrochloride, USP) injection. Baxter Healthcare
Corporation. Revised: 02/2012. Accessed January 30, 2014.
37. Vancocin (vancomycin hydrochloride, USP) capsule. ViroPharma. Revised: 12/2011. Accessed
February 27, 2014.
38. Penicillin V Potassium (penicillin V potassium, USP) tablet. Sandoz Inc. Revised: 10/2011. Accessed
January 30, 2014.
39. Amoxicillin (amoxicillin, USP) capsule. Ranbaxy Pharmaceuticals Inc. Revised: 05/2008. Accessed
January 27, 2014.
40. Cephalexin (cephalexin, USP) capsule. Ranbaxy Pharmaceuticals Inc. Revised: 03/2007. Accessed
January 28, 2014.
41. Cefaclor (cefaclor, USP) capsule. Alvogen, Inc. Revised: 03/2011. Accessed January 28, 2014.
42. Baumgartner JC, Xia T. Antibiotic susceptibility of bacteria associated with endodontic abscesses.
J Endod 2002;29(1):44-47.
43. Murray PR, Rosenblatt JE. Penicillin resistance and penicillinase production in clinical isolates of
Bacteroides melaninogenicus. Antimicrobial Agents Chemother 1977;11:605-608.
44. Edson RS, Rosenblatt JE, Lee DT. Recent experience with antimicrobial susceptibility of anaerobic
bacteria: increasing resistance to penicillin. Mayo Clin Proc 1982;57:737-741.
45. Kinder SA, Holt SC, Korman KS. Penicillin resistance in subgingival microbiota associated with adult
periodontitis. J Clin Microbiol 1986;23:1127-1133.
46. Heimdahl A, Von Konow L, Nord CE. Isolation of beta-lactamase producing Bacteroides strains
associated with clinical failures with penicillin treatment of human orofacial infections. Arch Oral Biol
47. Walker C, Gordon J. The effect of clindamycin on the microbiota associated with refractory
periodontitis. J Periodontal 1990;61:692-698.
48. Witcher BL, Beirne OR, Smith RA. Beta-lactamase producing Bacteroides melaninogenicus and
osteomyelitis of the mandible. J Oral Med 1983;38:17-20.
49. Hackman AS, Wilkins TD. Influence of penicillinase production by strains of Bacteroides
melaninogenicus and Bacteroides oralis on penicillin therapy of experimental mixed anaerobic
infection in mice. Arch Oral Biol 1976; 21:385-389.
50. Handal T, Olsen I. Antimicrobial resistance with focus on oral beta-lactamases. Eur J Oral Sci
51. Thaler DS. The evolution of genetic intelligence. Science 1994;264:224-225.
52. Abbanat D, Morrow B, Bush K. New agents in development for the treatment of bacterial infections.
Curr Opin Pharmacol 2008 Oct;8(5):582-592.
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
53. Ryou M, Coen DM. Pharmacology of bacterial infections: DNA replication, transcription, and
translation. In Golan DE, Tashjian, Jr. AH, Armstrong EJ, Armstrong AW. Ed. Principles of
pharmacology. The pathophysiologic basis of drug therapy. 2nd ed. 2008. Wolters Kluwer/Lippincott
Williams & Wilkins. Baltimore, MD.
54. Walker RC. The Fluoroquinolones. Mayo Clinic Proceedings 1999;74:1030-1037.
55. Cipro (ciprofloxacin hydrochloride, USP) tablet. Revised: 08/2013. Accessed February 27, 2014.
56. Levaquin (levofloxacin, USP) tablet. Lake Erie Medical DBA Quality Care Products LLC. Revised:
10/2012. Accessed February 27, 2014.
57. Avelox (moxifloxacin hydrochloride, USP) tablet. Red Pharm Drug Inc. Revised: 08/2011. Accessed
February 27, 2014.
58. Al-Nawas B1, Walter C, Morbach T, Seitner N, et al., Clinical and microbiological efficacy of
moxifloxacin versus amoxicillin/clavulanic acid in severe odontogenic abscesses: a pilot study. Eur
J Clin Microbiol Infect Dis. 2009 Jan;28(1):75-82.
59. Cachovan G1, Böger RH, Giersdorf I, Hallier O, et al., Comparative efficacy and safety of
moxifloxacin and clindamycin in the treatment of odontogenic abscesses and inflammatory
infiltrates: a phase II, double-blind, randomized trial. Antimicrob Agents Chemother. 2011
60. Ivers LC, Ryan ET. Pharmacology of parasitic infections. In Golan DE, Tashjian, Jr. AH, Armstrong
EJ, Armstrong AW. Ed. Principles of pharmacology. The pathophysiologic basis of drug therapy. 2nd
ed. 2008. Wolters Kluwer/Lippincott Williams & Wilkins. Baltimore, MD.
61. Metronidazole (metronidazole, USP) tablets. Watson Labs. Revised: 11/2006. Accessed January
62. Kasten MJ. Clindamycin, metronidazole, and chloramphenicol. Mayo Clin Proc. 1999
63. Sulfamethoxazole and trimethoprim (sulfamethoxazole and trimethoprim, USP) tablets. Vista
Pharmaceuticals, Inc. Revised:12/2012. Accessed February 27,2014.
64. Smilack JD. The tetracyclines. Mayo Clin Proc. 1999 Jul;74(7):727-729.
65. Minocin (minocycline hydrochloride, USP) capsule. Triax Pharmaceuticals, LLC. Revised: 12/2013.
Accessed February 27, 2014.
66. Doxycycline hyclate (doxycycline hyclate, USP) capsule. Kikma Pharmaceuticals. Revised:
09/2009. Accessed February 27, 2014.
67. Czeizel AE, Rockenbauer M. A population-based case-control teratologic study of oral
oxytetracycline treatment during pregnancy. European Journal of Obstetrics & Gynecology and
Reproductive Biology. 2000;88:27-33.
68. Edson RS, Terrell CL. The aminoglycosides. Mayo Clin Proc. 1999 May;74(5):519-528.
69. Gentamycin sulfate (gentamycin sulfate, USP) injection. Hospira, Inc. Revised: 06/2011. Accessed
February 27, 2014.
70. Clindamycin hydrochloride (clindamycin hydrochloride, USP) capsule. Cardinal Health. Revised:
08/2013. Accessed January 27, 2014.
71. Ellison SJ. The role of phenoxymethylpenicillin, amoxicillin, metronidazole and clindamycin in the
management of acute dentoalveolar abscesses – a review. Br Dent J 2009;206(7):357-362.
72. Alvarez-Elcoro S, Enzler MJ. The macrolides: erythromycin, clarithromycin, and azithromycin. Mayo
Clin Proc. 1999 Jun;74(6):613-634.
73. Azithromycin (azithromycin, USP) tablet. Greenstone LLC. Revised: 08/2010.
Accessed January 17, 2014.
74. Walker CB. The acquisition of antibiotic resistance in the periodontal microflora. Periodontology
2000 1996;10:79-88.
75. Moore PA. Dental therapeutic indications for the newer long-acting macrolide antibiotics. J Am Dent
76. McCracken GH Jr. Microbiologic activity of the newer macrolide antibiotics. Pediatr Infect Dis J.
77. Addy LD, Martin MV. Azithromycin and dentistry – a useful agent? Br Dent J 2004;197(3):
141-143, 138.
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
78. Al-Belasy FA, Hairam AR. The efficacy of azithromycin in the treatment of acute infraorbital space
infection. J Oral Maxillofac Surg 2003;61(3):310-316.
79. Dirks SJ, Terezhalmy GT. The patient with an odontogenic infection. Quintessence Int 2004
80. Massler M, Pawlak J. The affected and infected pulp. Oral Surg Oral Med Oral Pathol 1977;43:
81. Torneck CD. A report of studies into changes in the fine structure of the dental pupl in human caries
pulpitis. J Endod 1981;7:8-16.
82. Huang GT, Potente AP, Kim JW, Chugal N, Zhang X. Increased interleukin-8 expression in
inflammed human dental pulps. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;88:214-
83. Hahn CL, Falkler WA Jr. Antibodies in normal and diseased pulps reactive with microorganisms
isolated from deep caries. J Endod 1992;18:28-31.
84. Rauschenberger CR, Bailey JC, Cootauco CJ. Detection of human IL-2 in normal and inflamed
dental pulp. J Endod 1997; 23:366-370.
85. Matsushima K, Ohbayashi E, Takeuchi H, Hosoya S, Abiko Y, Yamakazi M. Stimulation of
interleukin-6 production in human pulp cells by peptidoglycans from Lactobacillus casei. J Endod
86. Oguntebi BR, DeSchepper EJ, Taylor TS, White CL, Pink FE. Postoperative pain incidence related
to the type of emergency treatment of symptomatic pulpitis. Oral Surg Oral Med Oral Pathol
87. Nagle D, Reader A, Beck M, Weaver J. Effect of systemic penicillin on pain in untreated irreversible
pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;90:636-640.
88. Keenan JV1, Farman AG, Fedorowicz Z, Newton JT. Antibiotic use for irreversible pulpitis.
Cochrane Database Syst Rev. 2005 Apr 18;(2):CD004969.
89. Brennan MT, Runyon MS, Batts JJ, Fox PC, et al. Odontogenic signs and symptoms as predictors
of odontogenic infections. J Am Dent Assoc 2006;137:62-66.
90. Ranta H, Haapasalo M, Ranta K, Konyiainan S, Kerisuo E, Valtonen V, Suuronen R, Hovi T.
Bacteriology of odontogenic apical periodontitis and effect of penicillin treatment. Scand J Infect Dis
91. Fouad AF, Rivera EM, Walton RE. Penicillin as a supplement in resolving the localized acute apical
abscess. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996;81:590-595.
92. Cioffi GA, Terezhalmy GT, Parlette HL. Cutaneous draining sinus tract: an odontogenic etiology.
J Am Acad Dermatol. 1986 Jan;14(1):94-100.
93. Stone A, Straitigos GT. Mandibular Odontogenic Infection with Serious Complications. Oral Surg
Oral Med Oral Pathol. 1979 May;47(5):395-400.
94. Meislin HW. Pathogen identification of abscesses and cellulitis. Ann Emerg Med 1986
95. Bratton TA, Jackson DC, Nkungula-Howlett T, Williams CW, Bennett CR. Management of complex
multi-space odontogenic infections. J Tenn Dent Assoc 2002;82(3):39-47.
96. American Dental Association, Council on Scientific Affairs. Antibiotic use in dentistry. J Am Dent
Assoc 1997;128:648.
97. Haas DA, Epstein JB, Eggert FM. Antimicrobial resistance: dentistry's role. J Can Dent Assoc. 1998
98. Akimoto Y, Nishimura H, Komiya M, Shibata T, Kaneko K, Fujii A, et al. Ampicillin concentrations
in human serum and dental pulp following a single oral administration. J Nihon Univ School Dent
99. Runyon MS, Brennan MT, Batts JJ, et al. Efficacy of penicillin for the dental pain without overt
infection. Acad Emerg Med 2004;11:1268-1271.
100. Heimdahl A, Nord CE. Treatment of orofacial infections of odontogenic origin. Scand J Infect Dis
101. Meurman JH. Dental infections and general health. Quintessence Int 1997;28:807-811.
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
102. Harrison JW, Svec TA. The beginning of the end of the antibacterial era? Part II. Proposed
solutions to antibiotic use. Quintessence Int 1998;29:223-229.
103. Gruchalla RS, Pimohamed M. Antibiotic allergy. N Engl J Med 2006;354(6):601-609.
104. Nord CE. Mechanisms of beta-lactam resistance in anaerobic bacteria. Rev Infect Dis
105. Lewis MAO, Parkhurst CL, Douglas CWI, Martin MV, Absi EG, Bishop PA, et al. Prevalence
of penicillin resistant bacteria in acute suppurative oral infection. J Antimicrob Chemother
106. FDA Drug Safety Communications. Azithromycin (Zithromax or Zmax) and the risk of potentially
fatal heart rhythms. March 12, 2013. Accessed January 29, 2014.
107. Malhotra-Kumar S, Lammens C, Coenen S, Van Herck K, Goossens H. Effect of azithromycin
and clarithromycin therapy on pharyngeal carriage of macrolide-resistant streptococci in
healthy volunteers: a randomised, double-blind, placebo-controlled study. Lancet. 2007 Feb
108. Sanford JP, Low DE, Judd PL, Davidson RJ. Antibacterial treatment options in the management of
odontogenic infections. J Can Dent Assoc 1998;64:508-514.
109. Chardin H, Yasukawa K, Nouacer N, Plainvert c, et al. Reduced susceptibility to amoxicillin of oral
streptococci following amoxicillin exposure. The Cochrane Center Register of Controlled Trials
(CENTRAL) 2012 Issue 3. The Cochran Collaboration. Published by John Wiley & Sons, Ltd.
110. Kuriyama T. Nakagawa K. Karasawa T. Saiki Y. Yamamoto E. Nakamura S. Past administration
of beta-lactam antibiotics and increase in the emergence of beta-lactamase-producing bacteria in
patients with orofacial odontogenic infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod
111. Gordon J, Walker C, Hovliaras C. Efficacy of clindamycin hydrochloride in refractory periodontitis:
24-month results. J Periodontol 1990;61:686-691.
112. Gilmore WC, Jacobus NV, Gorbach SL, et al. A prospective double blind evaluation of penicillin
versus clindamycin in the treatment of odontogenic infections. J Oral Maxillofac Surg 1988;46:
113. Von Konow L, Kondell PA, Nord CE, Heimdahl A. Clindamycin versus phenoxymethylpenicillin in
the treatment of acute orofacial infections. Eur J Clin Microbiol Infect Dis 1992;11:1129-1135.
114. Mangundjaja S. Hardjewinata K. Clindamycin versus ampicillin in the treatment of odontogenic
infections. Clin Ther 1990;12:242-249.
115. Hupp JR. Antibacterial, antiviral, and antifungal agents. Oral Maxillofac Surg Clin North Am.
116. Sandor GK, Low DE, Judd PL, Davidson RJ. Antimicrobial treatment options in the management of
odontogenic infections. J Can Dent Assoc. 1998 Jul-Aug;64(7):508-14.
117. Kelly CP, LaMont T. Clostridium difficile – More difficult than ever. N Engl J Med 2008;359(18):
118. Lodi G1, Figini L, Sardella A, Carrassi A, Del Fabbro M, Furness S. Antibiotics to prevent
complications following tooth extractions. Cochrane Database Syst Rev. 2012 Nov
119. Esposito M, Worthington HV, Loli V, Couthard P, Grusovin MG. Interventions for replacing missing
teeth: antibiotics at dental implant placement to prevent complications. Cochrane Database Syst
Rev. 2010 Jul 7;(7):CD004152.
120. Wilson W, Taubert KA, Gewitz M, Lockhart PB, et al. Prevention of infective endocarditis:
Guidelines from the American heart Association. J Am Dent Assoc 2008;139(suppl):3S-24S.
Accessed January 29, 2014.
121. AAOS/ADA. Prevention of orthopaedic implant infection in patients undergoing dental procedures.
Evidence-based guideline and evidence report. December 7, 2012. Accessed February 23, 2013.
122. The ADA/AAOS Expert Panel. Advisory statement. Antibiotic prophylaxis for dental patients with
total joint replacement. J Am Dent Assoc 2003;134(7):895-898.
123. Huber MA, Terezhalmy GT. The patient with a transient bacteremia. Gen Dent. 2005 Mar-
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
124. Lockhart PB, Loven B, Brennan MT, Fox PC. The evidence base for the efficacy of antibiotic
prophylaxis in dental practice. J Am Dent Assoc 2007;138(4):458-474.
125. Termine N, Panzarelle V, Ciavarella D, Lo Muzio L, et al. Antibacterial prophylaxis in dentistry and
oral surgery: use and misuse. Intl Dent Jl 2009;59:263-270.
126. Zallen RD, Curry J. A study of antibiotic usage in compound mandibular fractures. J Oral Surg
127. Greenberg RN, James RB, Marier RL, et al. Microbiologic and antibiotic aspects of infections in the
oral and maxillofacial region. J Oral Surg 1979;37:873-884.
128. James RB, Fredrickson C, Kent J. Prospective study of mandibular fractures. J Oral Surg
129. Miles BA, Potter JK, Ellis E. The efficacy of postoperative antibiotic regimens in the open treatment
of mandibular fractures: a prospective randomized trial. J Oral Maxillofac Surg 2006;64:576-582.
130. Simo R, French G. The use of prophylactic antibiotics in head and neck oncology surgery. Curr
Opin Otolaryngol Head Neck Surg 2006;14(2):55-61.
131. Harrison JW, Svec TA. The beginning of the end of the antibacterial era? Part I. The problem:
Abuse of the "miracle drugs". Quintessence Int 1998;29:151-162.
132. Davies J. Inactivation of antibiotics and the dissemination of resistance genes. Science
133. Neu HC The crisis in antibiotic resistance. Science. 1992 Aug 21;257(5073):1064-1073.
134. Hawkey PM The origins and molecular basis of antibiotic resistance. BMJ. 1998 Sep
135. Koshland DE. The microbial wars. Science 1992;257:1021.
136. Brisson-Noël A, Arthur M, Courvalin P. Evidence for natural gene transfer from gram-positive cocci
to Escherichia coli. J Bacteriol. 1988 Apr;170(4):1739-1745.
137. Trieu-Cuot P, Carlier C, Courvalin P. Conjugative plasmid transfer from Enterococcus faecalis to
Escherichia coli. J Bacteriol 1988;170:4388-4391.
138. Higgins NP. Death and transfiguration among bacteria. 1992;17:207-211.
139. Travis J. Possible evolutionary role exposed for "jumping genes". Science 1992;257:884-885.
140. Travis J. Reviving the antibacterial miracle. Science 1994;264:360-362.
141. Cohen ML. Epidemiology of drug resistance: Implications for a post-antimicrobial ear. Science
142. Tomasz A. Multiple-antibiotic-resistant pathogenic bacteria. N Engl J Med 1994;330:1247-1251.
143. Hughes VM, Datta N. Conjugative plasmids in bacteria of the "pre-antibiotic" era. Nature
144. Ray WA, Murray KT, Hall K, et al. Azithromycin and the risk of cardiovascular death. N Engl J Med
145. FDA Pregnancy Categories. Accessed January 12, 2014.
146. Ito S. Drug therapy for breast-feeding women. N Engl J Med. 2000 Jul 13;343(2):118-126.
147. Kacew S. Adverse effects of drugs and chemicals in breast milk on the nursing infant. J Clin
148. Hersch EV. Adverse drug interactions in dental practice: Interactions involving antibiotics. J Am Dent
149. Meechan JG. Polypharmacy and dentistry: 2. Interactions with analgesics and antimicrobials. Dent
Update. 2002 Oct;29(8):382-388.
150. Archer JS. Archer DF. Oral contraceptive efficacy and antibiotic interaction: A myth debunked. J Am
Acad Dermato 2002;46:917-923.
151. LaCasa C. California court denies wrongful birth claim. J Law Med Ethics 1996;24:273-274.
152. Council on Scientific Affairs, American Medical Association, et al. Drug interactions between oral
contraceptives and antibiotics. Obstet Gynecol. 2001 Nov;98(5 Pt 1):853-860.
153. American Dental Association Health Foundation Research Institute, Department of Toxicology.
Antibiotic interference with oral contraceptives. J Am Dent Assoc 1991;122:79.
154. American Dental Association Council on Scientific Affairs. Antibiotic interference with oral
contraceptives. J Am Dent Assoc 2002;133:880.
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
About the Authors
Leena Palomo, DDS, MSD
Dr. Palomo is Associate Professor of Periodontics and director DMD periodontics.
She is a diplomate of the American Board of Periodontology. She published several
articles in medical and dental journals. Additionally, she has been invited for
presentations at national and international professional meetings. Her commitment
to our dental students has been recognized. She earned her undergraduate as well
as DDS and MSD degrees from Case Western Reserve University in 1996 and 2004
Géza T. Terézhalmy, DDS, MA
Professor and Dean Emeritus
School of Dental Medicine
Case Western Reserve University
Dr. Terézhalmy is Professor and Dean Emeritus, School of Dental Medicine, Case
Western Reserve University. In addition, he is a Consultant, Naval Postgraduate
Dental School, National Naval Medical Center; and Civilian National Consultant for
Dental Pharmacotherapeutics, Department of the Air Force.
Dr. Terézhalmy earned a B.S. degree from John Carroll University; a D.D.S. degree from Case
Western Reserve University; an M.A. in Higher Education and Human Development from The George
Washington University; and a Certificate in Oral Medicine from the National Naval Dental Center. Dr.
Terézhalmy is certified by the American Board of Oral Medicine and the American Board of Oral and
Maxillofacial Radiology (Life).
Dr. Terézhalmy has many professional affiliations and over the past 40 years, has held more than
30 positions in professional societies. He has served as editor or contributing editor for several
publications, co-authored or contributed chapters for several books and has had over 200 papers
and abstracts published. Dr. Terézhalmy has accepted invitations to lecture before many local, state,
national, and international professional societies.
Crest® + Oral-B® at dentalcare.com Continuing Education Course, May 1, 2014
Source: https://dental.case.edu/media/school-of-dental-medicine/documents/resources/graduate-student-resources/dent-550/Systemic_Antibacterial_Agents_Clinical_Implications.pdf
Concussion Guide The Human Motion Institute at Randolph Hospital Concussion Guide for Parents GFELLER-WALLER CONCUSSION AWARENESS ACT The Gfeller-Waller Concussion Awareness Act was created to help educate, and prepare for concussions in high school and middle school athletics. The law is named for two North Carolina football players who died as a result of concussion related injury and whose deaths could have been prevented with proper preparation.
Models 1860, 1862, 1862E, 1864 PowerLuber Grease Gun (Lithium Ion) Series "A" EC Declaration of Confomrity Basic PowerLuber Model 1860 Lincoln declares that these products described under "Technical Data" are in compliance with 2006/42/EC and EN 60745-1 DEC - 2011 Form 404264 Section - D7 Page - 83