08hdc02899medical_practitioner
Medical Practitioner, Dr E
New Zealand Men's Clinic Ltd
A Report by the
Health and Disability Commissioner
08HDC02899
08HDC05986
08HDC07100
08HDC09984
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
Overview
This report considers the service(s) provided to four men who attended the New Zealand Men's Clinic (the Clinic) and were seen by the Clinic's sole medical practitioner, Dr E. The Clinic specialises in the treatment of erectile dysfunction, premature ejaculation, and related complaints. The four men complained about the service provided by Dr E and the Clinic. This investigation has reviewed the standard of assessment and clinical examination performed.
The four cases have been reported together because of the similarity of the issues raised.
Parties involved
Consumer/complainant
Consumer/complainant
Consumer/complainant
Consumer/complainant
Provider/medical practitioner
New Zealand Men's Clinic
Complaint and investigation
Between 28 February and 19 June 2008, the Health and Disability Commissioner
(HDC) received four complaints about the services provided by Dr E of the New
Zealand Men's Clinic (the Clinic). The formal issues identified for investigation are
set out in
Appendix 1.
Information was obtained from Mr A, Mr B, Mr C, Mr D, Dr E, and the Clinic. Expert
advice was obtained from general practitioner Dr Stuart Tiller, and is set out in
Appendices 2 to 5.
Information gathered during investigation
New Zealand Men's Clinic The New Zealand Men's Clinic (the Clinic), which advertises widely throughout New Zealand, states in its publicity material that it has "the most experienced staff in the country for erectile dysfunction (ED), premature ejaculation (PE), low sex drive, and performance anxiety related to these". It states that it provides the "broadest range of
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
treatments", and a "thorough consultation to assess erectile dysfunction and associated problems". The Clinic's advertising states:
"Our medical team has treated thousands of patients since 1995: between the ages of 18 and 93. Over 95% of our patients achieve success after their first visit, and getting a normal sex-life back without further assistance is quite achievable — depending on your circumstances.
Our staff are knowledgeable and approachable: we treat each patient with care and confidentiality, meaning you can relax in our clinics and enjoy your private one-on-one consultation."
Clinics are held across New Zealand.
Dr E Dr E is the sole medical practitioner working at the Clinic, and is described as the medical director. He is also a director, founder and owner. His annual practising certificate advises that he is to work within a collegial relationship, and he advised HDC that he is a member of the New Zealand College of Appearance Medicine (NZCAM), although this is not mentioned in publicity material.1
Dr E advised that he receives clinical supervision from a general practitioner and that he has a "strong collegial relationship" with a general practitioner in Sydney who works in the same clinical field.
"Erectile dysfunction falls under General Practice, nevertheless I have had nine years of clinical experience, virtually exclusively in this area and in addition I have attended conferences on impotence and men's health. I have a special interest in this area of general practice and am keenly committed to offering this service to the men of New Zealand. I am proud of the service which the Clinic has developed and is able to offer to our patients."
Complaints
Chronology On 25 January 2008, Mr A (aged 60) attended the Clinic in Whangarei in response to a leaflet received in the mail.
1 Dr Peter Chapman-Smith, Secretary and Treasurer of NZCAM, stated that Dr E is a second-year trainee member of NZCAM, and is not allowed to advertise his association with NZCAM "until he has passed his level 1 Diploma in [Appearance Medicine]".
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
Prior to a consultation with Dr E at the Clinic, a client is given a questionnaire to complete that asks for details of a client's medical history and current medications. Mr A stated on the questionnaire that he had diabetes. He also noted that he suffered from high blood pressure and was on medication to treat it, but there is no evidence that his blood pressure was recorded, or that a clinical examination was performed. Mr A's medication was recorded: atenolol (to treat high blood pressure); aspirin; lisinopril (to treat high blood pressure); simvastatin (to treat high cholesterol); and amlodipine (to treat high blood pressure).
Mr A noted on the questionnaire that the "main problem" for which he was seeking treatment was "maintaining an erection".
Mr A was also given a consent form for "injectable treatments", and a document stating that he had read the information provided at the initial consultation. Neither document was signed by Mr A. (Dr E accepts that the consent forms for the test dose and the ongoing injectable treatments were not signed by Mr A.)
In his subsequent letter to the Clinic of 1 February 2008, Mr A stated that, despite claims set out in the leaflet that "a thorough consultation would take place", his consultation with Dr E took "no more than five minutes, very few questions were asked, and little interest shown by [Dr E] to [Mr A's] list of existing medication taken for blood pressure problems, heart problems, and type 2 diabetes".
Mr A stated that Dr E "very quickly" decided to inject his penis with what he was told was "human growth hormone". Mr A advised that this worked "partially", but that Dr E advised that the dosage could be increased from the 16 units given that day to 25 units or 30 units.2 Mr A stated that "[n]o other treatments were considered, and no tests carried out at any time".
"I saw [Mr A] at our Whangarei Clinic which I attend on a monthly basis. He is a man who suffers from diabetes and had reported significant erectile dysfunction problems. There can be no doubt with his medical history that the most successful treatment for him is intracavernosal injection treatment. When I met with him on 25 January 2008 I reviewed his complaint and advised him that the above treatment was, in my opinion, the only option really available to him other than doing nothing is continuing with oral medications which have been inconsistent in the past.
At no time was any pressure put on [Mr A] to proceed with the treatment or for that matter to pay for the treatment. At no time during the consultation with him did I detect that he was unhappy. Had this been the case I would have stopped the consultation and reassured him and investigated any unhappiness further.
2 No unit of measurement was provided to HDC.
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
I had explained to [Mr A] that if he was to proceed with the treatment then a test dose of the injectable treatment proposed would be required to be administered. He was provided with documentation including the consent form entitled ‘Initial consultation' which warns of risks that can occur. I note no such risks occurred in this case.
After administering the test dose (this in my experience routinely takes 15 minutes or so) [Mr A] reported a satisfactory outcome and I have noted his test results on the form entitled ‘Physical examination sheet'. That records a 60%–70% response.
I reviewed the results with him and in discussion with him recommended a slightly stronger dose than the one prescribed in the initial test dose. He was content with this."
In his response to the provisional opinion, Dr E stated that he "always" asks the patients about the management of their diabetes and hypertension. Dr E added that Mr A assured him that "both his diabetes and hypertension were well controlled through his GP". However, Dr E accepts that he did not document this.
Dr E stated that, in his view, a "thorough peripheral vascular … examination" did not need to be performed. He argued:
"It is well known vascular disease is associated with erectile dysfunction nevertheless it is well known it is also associated with diabetes and hypertension."
Dr E stated that "I have had a lot of clinical experience with similar cases and was confident that my prescribing of the intracavernosal medication would enable [Mr A] to experience satisfactory intercourse".
Mr A elected to buy (for approximately $2,000) what he was told was a one year's supply of intracavernosal medication, and he was given a six-month supply, in one bottle, with the promise of the rest to be sent to him. However, Mr A noted that the six-month supply contained 480 units. Mr A calculated:
"This equates to 10 doses per month (acceptable) but only 8 units per dose, where [Dr E] gave … 16 units in trial, then recommended 25–30 units per dose."
After returning home, on two separate days Mr A administered 20 units and 25 units with no effect.
Mr A subsequently complained to the Clinic as he felt that the treatment did not work. In response to my provisional opinion, Dr E stated: "I went to great effort to resolve [Mr A's] initial problems, and was sure it was a technique issue, but was unable to help [Mr A] without him attending his follow-up consultation."
The Clinic has agreed to refund a portion of Mr A's charges.
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
Chronology On 18 February 2008, Mr B (aged 21) attended the Clinic in Auckland. On arrival, he was asked to complete the questionnaire, which asked about his medical history and current medications. He was also given a form to sign, entitled "Initial consultation", which he signed.
Mr B noted on the questionnaire that the "main problem" for which he was seeking treatment was "coming too soon" (premature ejaculation).
"I then took [Mr B] through to my consultation room and questioned him on particular aspects of his medical history and medications that may influence the medical safety in using medications to control premature ejaculation. … I have made various notes recording the erection symptoms that he was complaining of and that he had not trialled any other treatments other than supplements. The form I went through with him … confirms he had no epilepsy or other matters of concern (that is to say I additionally went over this with him verbally). I always explain that these questions are nothing to do with explaining why he is suffering from premature ejaculation but rather to make sure that he is a reasonable candidate for the medications that were available for this condition.
After taking the history of premature ejaculation, medical history, taking into account his age, my clinical assessment was that Clomipramine would be an appropriate medication to delay his ejaculation.
My rationale for the treatment was that he had no erection problems, was of a younger age and penile injections although very effective for treating premature ejaculation, are not appropriate for younger people unless their premature ejaculation is associated with erectile dysfunction problems or they do not respond to Clomipramine.
The nasal spray delivery was prescribed as it is fast acting and is only required in low doses to be effective for controlling premature ejaculation thereby reducing systematic side effects."
In his response to the provisional opinion, Dr E stated:
"All patients suffering from erectile dysfunction / premature ejaculation are given advice around this area and the conversation is directed by them and their comfort zone.
Many young men perceive that premature ejaculation is very rare and that they have a serious problem with an unknown cause. They are comforted to know that they are normal young men and that their condition is not the result of untoward
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
behaviour on their part. This pyschosexual counselling forms a fundamental part of a successful outcome at their consultation."
"When I first arrived at the clinic I was given a letter to read about premature ejaculation and was told that someone would be with me shortly. After approximately 25 minutes [Dr E] came and introduced himself. We went to his examination room where he asked me what he could [do to] help and I advised him that I believed I was experiencing premature ejaculation and wanted to know what could be medically done.
[Dr E] went straight to telling me about ‘Nasal Delivery technology' and the benefits of it being fast acting. [Dr E] told me that I should also do some exercises, which were provided to me on an information sheet. These were around sexual stimulation and being able to control the need to ejaculate and stopping it before reaching the point of no return.
[Dr E] explained to me that many men have this issue and the nasal spray is effective. I also enquired about the lozenges that were available but [was] advised that the nasal spray was the better option."
Mr B was not physically examined. Dr E prescribed 15ml clomipramine nasal spray, 50mg in 1ml. Mr B was not informed that the use of the medication prescribed was an unapproved use of an approved drug.
Mr B signed a consent form for clomipramine nasal spray, which set out information about the treatment method and possible side effects, including rare side effects. (A nose bleed was not specified as a possible side effect, although Dr E has now altered the consent form to include this.) The form contained a statement that the patient had "read and understood the above information all of which was explained fully prior to … signing".
On 24 February, Mr B used the nasal spray. Immediately after use, a nose bleed started, and he called the local emergency department and was advised how to pack his nose. Eventually, the bleeding stopped.
Mr B complained to the Clinic and received a full refund for the cost of the spray ($350), together with an apology for the discomfort he suffered.
Clomipramine Clomipramine is a drug that has been approved by Medsafe, but not in the form of a nasal spray. The guidance provided by Medsafe for prescribers states:
"For an unapproved medicine or unapproved use, the consumer should be advised of the unapproved status. The consumer should also be advised of the degree and
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
standard of the support for the use of the medicine, and of any safety concerns, or warnings or contraindications regarding its use in their particular condition."3
Dr E accepts that he did not tell Mr B that the use of clomipramine in a nasal spray was an unapproved use of an approved drug. The Clinic has since altered its practice, and clients are now advised of this.
Chronology On 15 April 2008, Mr C (aged 75) attended the Clinic in Tauranga because of difficulty getting an erection. He completed a questionnaire, and specifically mentioned a history of heart disease and high blood pressure. Mr C noted that he had had operations for an aortic valve replacement and triple coronary artery bypass grafts, and wrote down his medications: verapamil (for the treatment of angina); simvastatin (treatment of high cholesterol); allopurinol (treatment of gout); enalapril (treatment of hypertension); aspirin; and Somac (treatment of stomach ulcers).
Mr C was also given a form to sign, entitled "Initial consultation", which he signed.
Having completed the questionnaire, he was shown into a room. Dr E stated:
"I … took [Mr C] through to my consultation room and went through his medical history, as he had not filled it in while in the waiting area. I confirmed his medical concerns and current medications he was on. I noted that he had previous heart surgery and was on medications for his heart and blood pressure. I asked him if he was comfortable with the test dose procedure. He declined as he had been on penile injections previously and wasn't comfortable using them. [Mr C] did sign the Initial consultation form … although he declined the test dose procedure as above.
After [Mr C's] clinical assessment of his medical and surgical history, his history of erectile dysfunction, use of previous medications for erectile dysfunction, medications and allergies to medications, I advised [Mr C] that the penile injections would be the safest and most effective treatment, nevertheless I could prescribe an alternative treatment, being Apomorphine nasal spray.
My rationale for prescribing Apomorphine nasal spray was that he was unhappy to use the penile injections and Viagra had given him bad side effects (flushing). This meant [Mr C's] only other mainstream treatment for erectile dysfunction available to him was Apomorphine.
His blood pressure was well controlled and monitored on a regular basis."
3 See www.medsafe.govt.nz/profs/RIss/unapp.asp (June 2003).
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
(The documentation provided indicates that apomorphine lozenges were considered.)
The drug prescribed to Mr C on the document "Patient's medication" states "1xAPO sp".
A consent form signed by Mr C refers to the prescription of Apo-Phen nasal spray, which is a combination of two drugs: apomorphine and phentolamine. In his response to the provisional opinion, Dr E clarified that the nasal spray dispensed contained only apomorphine; no phentolamine was dispensed.
Mr C recalls that Dr E looked at the questionnaire and suggested the use of injections, which he declined. An apomorphine nasal spray was then suggested, which Mr C agreed to. Mr C was not physically examined and no clinical observations were performed. He was in the Clinic for only 15 minutes, and this included the time spent prior to his consultation completing the questionnaire. Mr C was not informed that the use of the medication prescribed was an unapproved use of an approved drug, and was not advised "of any possible side or adverse effects from using the nasal spray".
Dr E advised that the Clinic now informs patients of the unapproved use of an approved drug.
On his return home after the appointment, Mr C used the spray. Within 10 minutes he had "mild vomiting", and then collapsed onto the floor. He managed to "crawl" to the bed, and then "passed out cold" for almost three hours.
Mr C contacted the Clinic and, following discussion with the staff, was given a full refund of the cost of his treatment. Dr E stated that he had never experienced another patient having the same symptoms as Mr C. Dr E stated:
"I … have never heard of this being a response to this medication and I am extremely surprised … that this has happened. I cannot explain why this would be so."
Mr C described the effect of his treatment from Dr E as follows:
"The outcome of this experience is that I still have the problem but would not consider even a herbal remedy. If recognised medical professionals can act as quacks and charlatans what can be expected from persons without medical training who some see as quacks in the first instance.
The impact of all this is that medical treatment would not be again considered [by me], non medical treatment is to be avoided, so I am left with the loss of an agreeable and elementary function of my life several years earlier than I would have expected.
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
Regarding the nasal spray, the Clinic should be required to advise patients of possible effects. People with undiagnosed heart conditions could be in real danger."
Apomorphine Dr E has not stated the dosage of apomorphine in the nasal spray. Recognised side effects of apomorphine include vomiting and somnolence. Its use as a nasal spray is an unapproved use of an approved drug (see Medsafe advice, above).
Chronology On 12 May 2007, Mr D (aged 68) attended the Clinic in Dunedin. Mr D noted on the questionnaire that the "main problem" for which he was seeking treatment was "getting an erection". Mr D signed a consent form for "Injectable treatments" and "Initial consultation".
Dr E described the service provided to Mr D:
"[Mr D] was greeted at reception and given the questionnaire about his details, erectile dysfunction history, medical history, surgical history, and current medications being taken … He was also given a consent form for a penile injectable test dose of medication if required … [Mr D] was given time to complete these forms and read the material and he duly signed the [consent form].
I then took [Mr D] through to my consultation room and went through his history and confirmed his medical concerns and current medications he was on. This involved some discussion with him although I do not now recall exactly what was said. I have however made some of my own handwritten notes on the personal details and erection symptoms … reflecting points discussed with him. I noted he was getting very poor erections, only 10%. I asked him if he was comfortable with the test dose procedure. He told me he was agreeable to a test procedure and a penile injectable test dose was administered.
[Mr D] had only a moderate response. The assessment of this test dose gives a good indication of blood flow or insufficiency of it to the penis. In [Mr D's] case I assessed his condition as one of severe erectile dysfunction.4 I completed his form … In my clinical assessment of [Mr D], taking into account the result of the test dose and his erectile dysfunction history I recommended a course of intracavernosal injections, which he was advised to try to use at least once a week.
[Mr D] was shown how to use the medication with a model penis and explained the cost for the treatment of intracavernosal injections. [Mr D] appeared happy to proceed with the treatment."
4 Mr D does not recall Dr E advising him that he had "severe erectile dysfunction".
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
Dr E submitted that the consultation was not superficial, and that "care was taken to prescribe the most effective treatment and [Mr D] was clearly explained the cost of the medication". Dr E noted that erectile dysfunction is a sensitive issue and "a lot more conversation goes on during the examination than what is documented in the patient notes". Dr E added that Mr D's prescription of Hytrin "was discussed and there was no temporal relationship with the use of Hytrin and [Mr D's] erectile dysfunction".
Mr D described the consultation as "relatively quick". He was not physically examined and his pulse and blood pressure were not recorded. Mr D does not recall Dr E asking if he was comfortable with the test dose. He was not told about the cost of the treatment ($710) until he was at the receptionist's desk at the end of his visit to the Clinic. Mr D recalls:
"I feel the receptionist made me so embarrassed about the need to pay at that time that I was almost bullied into paying straight away. I wanted to discuss it with my wife who was nearby but the receptionist said I couldn't pay it off and only a credit card would be accepted. As it was such a sensitive situation anyway this only added to my embarrassment."
After Mr D complained to the Clinic, $300 was refunded to him.
Dr E's response to the provisional opinion
"The expert doctor, Dr Tiller, has not given any explanation as to his expertise. Although I am sure he is a very capable doctor and GP, I do not know how many young men he has sat down with and discussed their premature ejaculation, yet he is advising me on psychosexual counselling. This is not in any way to criticise Dr Tiller rather to identify the type of medicine I practice is very different to the general practice setting. Early on in the consultation I question patients as to whether they regularly see their GP and recommend that they have regular visits with their GP for general health. Very few young men would approach their GP about discussing premature ejaculation. Dr Tiller has made some valid points which I have taken note of and will incorporate into my future consultations. …
Being the only doctor, it is fair to say my note taking was not up to an acceptable standard as I got into a naïve trap of writing notes for myself and not for other doctors. I have implemented changes in my note taking reflective of this. I have another doctor working with me now who conducts peer reviews of notes.
I feel strongly that at no time has there been any case for allegation of serious medical neglect on my part. In the report I would agree with Dr Tiller in the use of phentolamine however, there was no phentolamine prescribed by myself in any cases nor any intention to prescribe phentolamine. I agree with Dr Tiller that it would have been medically inappropriate to have done so.
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
To gain a better understanding of my practice, I feel it is very important to understand how the clinic operates in order to address comments like ‘superficial visits', ‘more than a doctor who prescribes medication'. I, like many other doctors, know that conditions such as Premature Ejaculation and Erectile Dysfunction would better treated in the GP setting as the GP knows the patient better in terms of medically, socially, psychologically. However the reality is that often this does not happen and it is the patient's choice as to how and where they seek advice and treatment for these issues. There are also a number of GPs who are not comfortable talking about these issues from the feedback I have directly received from my patients. Comments like ‘you've had a good innings' and ‘you expect too much' are not uncommon. Thereby NZ Men's Clinic provides a niche area of medicine for want of a better word. This is a special interest of general practice and there are examples of other clinics with a special interest e.g appearance medicine, acupuncture, sports medicine, occupational therapy, etc. NZ Men's Clinic fills a real void. Prior to clinics like mine I have no doubt a lot of men would have made a choice to have to avoid sex.
The GP has a lot more options than they had 10 years ago with treatments like Viagra, Cialis, Uprima (no longer available, however you can get apomorphine compounded in a lozenge or spray form) and Levitra. However these treatments do not always solve the problem and plainly do not work in some cases even though they have been prescribed by an experienced GP. We often get patients referred from GPs and even urologists where they have been unable to find treatments that work.
So, I think it is important to understand that patients are coming to us for a solution and very few ever come to us for a general check up. The prescribing of medication becomes more prevalent than in the GP setting.
The cost of the medications range from $10 per dose to $25 per dose depending on the type of medication. This is in keeping with other clinics, urologists and pharmaceutical companies range of cost of treatment. We dispense all available types of medication for Erectile Dysfunction and Premature Ejaculation. None of the medications are subsidised, they typically will seem expensive to most people.
Cost is always an issue, patients do not like paying for medication. However we run a clinic that offers a service across New Zealand. The infrastructure cost of premises and 8 staff including myself can only be paid by the people benefitting from the service. The clinic has been in operation since 1993 and has successfully treated over 25,000 patients.
In order to run such a comprehensive clinic, the administrative staff must advertise for patients. The cost of advertising is large but is a necessary cost. If we did not advertise and offer clinics men would suffer in silence.
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
I believe we offer an important service that fills a medical need in society. I have understood Dr Tiller's concerns and have made changes in areas that I agree with. I do not accept that my actions have constituted a breach of Code [right] 4(1), reasonable care of the patient. I believe [I] offer a high degree of reasonable care and accept that there will be differences of opinion at times but my underlying aim as a medical professional is to maintain a high standard of care above reasonable.
While I am personally disappointed and sorry that the 4 cases have not had a successful outcome, they are by no means reflective of my care as a Doctor or of my clinic's standard practice. The thousands of successful patients that I have treated and continue to manage their treatment is a testament of the standard of care at my clinic.
I accept your criticism of my attention to section 4(2) due to my lack of understanding of the medicines act which was more administrative than negligent as I am very comfortable to explain to patients when prescribing medications for an unapproved use."
Dr E provided a report from Dr Sean Wright, a men's health specialist from Australia,
to support his response to the provisional opinion. Dr Wright's report is attached as
Appendix 6.
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
Code of Health and Disability Services Consumers' Rights
The following Rights in the Code of Health and Disability Services Consumers' Rights (the Code) are applicable to this complaint:
Right to Services of an Appropriate Standard
(1) Every consumer has the right to have services provided with reasonable care and
(2) Every consumer has the right to have services provided that comply with legal,
professional, ethical, and other relevant standards.
Right to be Fully Informed
(1) Every consumer has the right to the information that a reasonable consumer, in
that consumer's circumstances, would expect to receive, including —
(b) An explanation of the options available, including an assessment of the
expected risks, side effects, benefits, and costs of each option; and
(e) Any other information required by legal, professional, ethical, and other
relevant standards; …
Other relevant standards
Good medical practice ― A guide for doctors (Medical Council of New Zealand, 2005)
"
Medical care
Good clinical care
In providing care you must:
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
Keep clear, accurate, and contemporaneous patient records that report the relevant clinical findings, the decisions made, the information given to patients and any drugs or other treatment prescribed.
Prescribing drugs or treatment
You may prescribe drugs or treatment … only when you:
• have adequate knowledge of the patient's health
• are satisfied that the drugs or treatment are in the patient's best interest.
Usually this will require that you have a face-to-face consultation with the patient or discuss the patient's treatment with another registered health practitioner who can verify the patient's physical data and identity. …"
Opinion — Introduction
It is unusual for four similar complaints to be made over a short period, from unconnected complainants in widespread locations around the country (Whangarei, Auckland, Tauranga and Dunedin). Although for most of the men involved their primary complaint was the poor "value for money" they received from their consultations, the main issue of concern to me is the poor standard of assessment performed by Dr E.
For the reasons set out below, I consider that Dr E failed to provide services of an appropriate standard and adequate information to his patients, in breach of the Code. I also consider that the New Zealand Men's Clinic is vicariously liable for Dr E's breaches of the Code.
Opinion: Breach — Dr E
Mr A Mr A (aged 65) sought treatment from the Clinic for erectile dysfunction. He has a significant medical history, which he described on the Clinic's questionnaire, noting that he suffered from diabetes and high blood pressure. Mr A was also taking five medications that are standard for a patient with cardiovascular disease. However, Dr E performed no physical examination, and no clinical observations were recorded prior to the prescription of a prostaglandin injection.
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
Dr E submitted that he did discuss Mr A's diabetes and hypertension management with him, but failed to document this. I also note that no consent form was signed by Mr A, despite the Clinic's own caveat on the form that the doctor must ensure that the consent form has been signed and understood.
Dr Tiller advised:
"In my view an integral component of the management of a diabetic patient requesting erectile treatment would be history of the diabetes, including current control of hyperglycaemia and hyperlipidaemia. Unless these areas of management are controlled well, any improvement in erectile function can be expected to be short lived because control of further vascular disease is required to optimise erectile function. [Dr E] made no attempt to obtain history of the current diabetic and cardiac status of [Mr A]. While the ongoing management of these conditions would remain the responsibility of the general practitioner an assessment of these matters was required in order to offer effective long term treatment. [Dr E] should also have examined the peripheral arteries in the groin and legs and examined for an abdominal bruit that might suggest arterial disease of the aorta. Such disease would affect the arterial supply to the penis. Vascular surgical advice may have been warranted."
Dr E's expert, Dr Sean Wright stated that "whilst Dr Tiller's opinion strictly speaking, is medically correct it overlooks the practicalities of this situation … It is not appropriate for a clinic such as this to manage a patient's ongoing medical problems, these patients invariably are after a ‘quick fix solution' that will enable an erection on demand."
Dr Wright did, however, agree with Dr Tiller that the history taking, physical examination and record keeping could have been more thorough. Dr Wright also noted that, while the choice of treatment may not have been affected and "Dr E may be able to arrive at the appropriate conclusion swiftly, it would be prudent to take time to outline to the patient why other measures etc are not appropriate".
I accept that patients attend men's health clinics because they are seeking specific treatments and that recurrent themes will arise. However, a health professional who allows consultations and treatment plans to become routine runs the risk that important details of a patient's medical history will be missed. In case 06HDC11343, I stated:
"The Code confirms that the Commissioner as decision-maker is expected to form an independent opinion on the reasonableness of the care provided. While I accept that there can often be a legitimate range of responsible opinion and practice, I am also conscious of my responsibility, as an independent guardian of patients' rights, to distinguish between mediocre and good practice."
I endorse Dr Tiller's view that, for a patient with Mr A's significant medical history, Dr E should have performed a more complete examination prior to offering treatment,
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
and a vascular surgery referral may have been warranted. In addition, although I accept that there was discussion about the intended treatment, the consent forms were not signed.
Dr E's treatment of Mr A shows signs of having been superficial. Mr A's description of the consultation having been brief seems convincing, and is supported by the limited documentation.
By providing a cursory assessment, Dr E failed to provide Mr A services with reasonable care and skill, and breached Right 4(1) of the Code. By failing to document his care in relation to Mr A, in particular the failure to ensure that consent forms were signed, Dr E breached Right 4(2) of the Code.
Mr B Mr B is a healthy young man (aged 21) who sought treatment for premature ejaculation. It is clear that Dr E's assessment of Mr B was superficial. Although a physical examination may not have been necessary, given Mr B's age and health background, he should have been asked questions about his sexual functioning, and should have received "psychosexual advice and education in addition to any treatments on offer" (in the words of Dr Tiller).
Dr Wright notes that "while these psychosocial aspects would certainly have added to the history, they would have had no bearing on the case management at all. They are quite simply irrelevant in a case of premature ejaculation in a young healthy male with no erectile difficulty." However, Dr Wright's opinion illustrates his lack of familiarity with the patient-centred approach that is expected under New Zealand's Code. Right 6 of the Code affirms a patient's right to the information that a reasonable patient, in that patient's circumstances, would expect to receive about his condition (including any contributing factors). As Dr E has pointed out, men attend the Clinic because they do not always feel comfortable discussing sexual dysfunction with their GP. Good information is all the more important in such "one-off" consultations, when a patient may not return for further advice.
Dr E acknowledged that "psychosexual counselling forms a fundamental part of a successful outcome" of a patient's consultation. However, Mr B describes a rushed consultation without "counselling" of any sort. In my view, Dr E's assessment was deficient.
I also note that Dr E prescribed an approved medicine for use in an unapproved manner. Although this is permissible in some circumstances, a medical practitioner should advise the patient that the proposed use is unapproved. Dr E did not do so in Mr B's case.
By providing a cursory assessment, Dr E failed to provide Mr B services with reasonable care and skill, and breached Right 4(1) of the Code. By failing to advise Mr B of the unapproved use of an approved drug, Dr E did not provide Mr B
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
information that was legally required, and therefore breached Right 6(1)(e) of the Code.
Mr C Mr C (aged 75) had a significant cardiac history, including two major operations (a coronary artery bypass and an aortic valve repair), when he attended the Clinic. Despite this history, and the fact that he was taking a number of cardiac medications, Dr E performed no clinical examination on Mr C and recorded no clinical observations.
Dr E clarified that he prescribed only apomorphine, and not phentolamine. He described the error as a typographical mistake. It resulted in subsequent reviewers (Drs Tiller and Wright) being unsure what drugs were actually prescribed. This is a good example of why clinical records need to be accurate. I also note that the dosage of the medication was not recorded.
Dr Tiller advised that, prior to the prescription of the two documented medications (apomorphine and phentolamine), a cardiology consultation was required because of the potential effect of the medications, particularly phentolamine, which is contraindicated in patients with known coronary artery disease. While Dr Wright commented that such a referral was not "mandatory" in this case, and I accept that phentolamine was not dispensed, he added that a referral would have been warranted "if there were concerns on a clinical basis". In this case, Dr E made no clinical assessment, and therefore he had no such basis on which to conclude whether a cardiac referral was warranted. Dr Wright considered "[Dr E's] history taking, note taking and examination to be inadequate" in this case.
I note that the use of apomorphine as a nasal spray is not approved by Medsafe, and Mr C was not advised of this. Dr Wright advised that apomorphine should not have been prescribed in this case, and "its use in unstable coronary disease is not recommended".
It is not known for certain what caused Mr C's collapse following his use of the nasal spray. However, the collapse occurred immediately after his use of apomorphine (which is contraindicated for patients with a cardiac history), having been taken nasally (which would result in quick action). I am surprised by Dr E's subsequent comment that he cannot explain what caused Mr C's collapse, and that Dr E has not considered the possibility that the collapse was caused by the medication he had prescribed.
By performing a cursory assessment, Dr E failed to provide Mr C services with reasonable care and skill, and breached Right 4(1) of the Code. By failing to advise Mr C of the risks associated with prescribing apomorphine, Dr E failed to provide an assessment of the expected risks, and breached Right 6(1)(b) of the Code. By failing to advise Mr C of the unapproved use of an approved medication, Dr E breached Right 6(1)(e) of the Code.
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
Mr D Mr D also sought treatment from the Clinic for erectile dysfunction. He described Dr E's assessment as very superficial, and the documentary evidence supports this view. Again, no clinical examination was performed, and no clinical observations recorded. Both should have occurred given Mr D's age (68). Dr Tiller noted that one of the medications that Mr D was taking has an adverse effect of impotence, yet there appears to have been no assessment by Dr E of this possible cause.
Dr E initially stated that he "could not now recall exactly what was said during his discussion with [Mr D]". However, Dr E later advised that "the use of [Mr D's] Hytrin was discussed and there was no temporal relationship with the use of Hytrin and his erectile dysfunction". There is no record of any such discussion, which Mr D does not recall.
Dr E's expert, Dr Wright, suggested that Mr D's consultation is "what would be expected from the average GP when a patient requests Viagra". In his view it "is simply not practical to alter medications for other conditions in an attempt to alleviate erectile difficulty".
In weighing the views of Drs Tiller and Wright, I am mindful of their different backgrounds. Dr Tiller is an experienced general practitioner with over 28 years' experience in a variety of settings. He is a Fellow of the Royal New Zealand College of General Practitioners, which supported his appointment as clinical advisor to HDC. Through his work with HDC, he is very familiar with the application of the New Zealand Code of Rights in a practical setting. Dr Wright is also experienced, having worked for seven years in the men's health area prior to taking up his current anaesthetics role. However, he is not familiar with the Code and the specific requirements that arise in New Zealand practice.
As noted above, Right 6 of the Code requires a patient-centred approach to consultations so that the patient receives appropriate information about his condition and the factors that could be contributing to it. The possibility that impotence may be caused by a patient's current medications is obviously information that should be disclosed by a health professional assessing a patient's erectile dysfunction.
There is also conflict over whether Mr D was made aware of the potential cost of treatment. I endorse the view of Dr Tiller that "where a doctor is aware that a recommended course of treatment will be expensive, that some information in that regard should be provided by the prescribing doctor". Dr E stated that Mr D was advised of the cost, yet there is no documentary evidence to support his view. In contrast, Mr D stated that he was surprised to find out the cost when he was leaving, and felt pressured to pay at the time. Given Mr D's description of a consultation that was "relatively quick", and with no contrary documentary evidence, I find his account credible.
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
While I accept that the treatment ultimately prescribed may have been appropriate, Mr D was not provided with a reasonable standard of care before that point was reached.
By performing a cursory assessment, Dr E failed to provide Mr D services with reasonable care and skill, and breached Right 4(1) of the Code. By failing to advise Mr D of the costs of treatment at an earlier stage of the consultation, Dr E breached Right 6(1)(b) of the Code.
Viewing these four complaints together, my impression is that Dr E provided a poor standard of care in each case. He treated the men as customers or clients rather than patients. As noted by Dr Tiller, "a doctor is more than a source of prescription medicines".
In each of the cases, the standard of assessment was below the standard expected of a medical practitioner, and in relation to Mr C and Mr A I consider the assessment to have been well below an acceptable standard because of their significant medical history.
Dr E and Dr Wright both made the point that patients attend men's clinics looking for a "quick fix solution", not a general check-up. However, I do not consider that this absolves health professionals from their responsibility to take an appropriate history, conduct an examination and provide information about risks, benefits, options and costs. In August 1997, because of consumer complaints, the Deputy Premier of New South Wales appointed a committee to "investigate and inquire into impotency treatment services in New South Wales".5 In relation to patient assessment, diagnosis and care, the inquiry found:6
"The majority of submissions to the Committee from consumers, professional associations and health care practitioners identified the lack of appropriate standards of care and treatment as a major issue. The Committee was informed by the main clinic operators that 95 per cent of patients are offered multi-drug injection therapy during the initial consultation.
This focus on a single method treatment without standardised medical review or follow up was found by the Committee to be accompanied by a failure to assess adequately the medical or psychological history of patients or to provide them with sufficient information on their options for treatment. Patients received inadequate information concerning the risks of any complications which may develop from the therapy."
5 1998 Report of the Ministerial Committee of inquiry into impotency treatment in New South Wales.
The relevant recommendations from the report are attached as
Appendix 7.
6 See http://www.hccc.nsw.gov.au/downloads/impo_rep.pdf
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
Similar themes are present in this case. A cursory assessment, with little discussion of relevant medical and psychosocial factors, led to the patients feeling inadequately assessed and treated.
I am also concerned by the practice of giving a patient leaflets to read and consent forms to sign
prior to their first consultation with a doctor. When men who are first-time patients are seeking treatment for a sensitive problem such as erectile dysfunction, particular care is needed to ensure that the men understand their treatment options and do not feel pressured to purchase a recommended treatment. Information about costs is especially important when an expensive course of treatment is recommended.
What happened to the men in these cases verges on exploitation. They certainly did not give informed consent to treatment — and could not do so simply by completing a questionnaire and signing a consent form before their first consultation.
Opinion: Breach — The New Zealand Men's Clinic
Under section 72(2) of the Act, an employing authority may be vicariously liable for an employee's failure to comply with the Code. Section 72(1) of the Act states that the term "employing authority" means a health care provider or a disability services provider. Section 3(k) of the Act states that a health care provider includes any person who provides health services to the public. The New Zealand Men's Clinic (the Clinic) provides health services to the public, and thus falls within the definition of health care provider and qualifies as an employing authority.
To establish vicarious liability, it must be established that Dr E was an employee, agent or member of the Clinic.
Dr E is both a director and 100% shareholder of the Clinic, and he represents himself as having a close affiliation with the Clinic. There are circumstances in which the actions of a person can lead to a relationship of agency being implied. As noted by the Court of Appeal:7
"The legal principles relating to ostensible or apparent agency are well settled. A person who by words or conduct has allowed another to appear to a third party to be his or her agent cannot afterwards repudiate that agency."
In my view, Dr E is (at the very least) an agent of the Clinic and therefore section 72 applies.
7
Arthur Watson Savage v Kathleen Taylor (unreported, CA 103/95, 19 March 1996, Richardson P).
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
The Clinic's use of questionnaires and consent forms prior to a consultation with a clinician were not designed to ensure that Dr E provided an appropriate standard of care and obtained fully informed consent. Dr E's actions were taken with the Clinic's express or implied authority. In these circumstances, the Clinic is vicariously liable for Dr E's breaches of the Code.
I recommend that Dr E:
• apologise to Mr A, Mr B, Mr C and Mr D for his and the Clinic's breaches of the
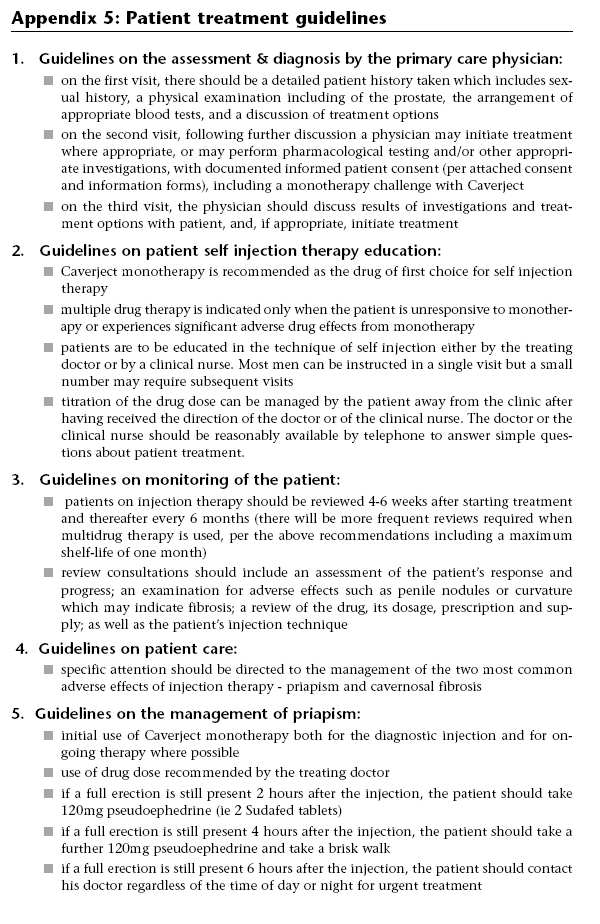
• review his practice in light of this report and the patient treatment guidelines
appended to the 1998 Report of the Ministerial Committee of inquiry into
impotency treatment in New South Wales (see
Appendix 7).
Follow-up actions
• A copy of this report will be sent to the Medical Council of New Zealand with a
recommendation that Dr E's competence be reviewed.
• A copy of this report with details identifying the parties removed, except the name
of the New Zealand Men's Clinic and the experts who advised on this case, will be sent to the New Zealand College of Appearance Medicine and the Royal New Zealand College of General Practitioners, and placed on the Health and Disability Commissioner website, www.hdc.org.nz, for educational purposes.
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
Appendix 1
Issues notified for investigation
Mr A • The appropriateness of care and the adequacy of information provided to Mr A by
Dr E and New Zealand Men's Clinic Ltd.
Mr B • The appropriateness of care provided to Mr B by Dr E, including the adequacy of
the clinical assessment and the adequacy of the information provided.
• The appropriateness of care and adequacy of information provided to Mr B by
New Zealand Men's Clinic Ltd in February 2008.
Mr C • The appropriateness of care provided to Mr C by Dr E, including the adequacy of
the clinical assessment and the adequacy of the information provided.
• The appropriateness of care and adequacy of information provided to Mr C by
New Zealand Men's Clinic Ltd in April 2008.
Mr D • The appropriateness of care provided to Mr D by Dr E, including the adequacy of
the clinical assessment and the adequacy of the information provided.
• The appropriateness of care and adequacy of information provided to Mr D by
New Zealand Men's Clinic Ltd, in particular whether he was provided with an assessment of the costs of the services.
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
Appendix 2
Expert advice from Dr Stuart Tiller: Mr A
"Thank you for the request that I provide clinical advice in relation to specific questions posed regarding the care provided by [Dr E] to [Mr A] at the New Zealand Men's Clinic.
Advice requested.
• General advice on the standard of care provided.
• Specific advice on the standard of the clinical assessment/examination
• Specific advice on the clinical treatment prescribed and/or dispensed.
• Whether any professional standards apply, and whether these standards
were complied with.
• Any other comment.
The complaint.
[Mr A] has complained that his consultation with [Dr E] was brief and the injectable medication for erectile dysfunction provided was ineffective despite great cost.
The provider response — [Dr E].
‘[Mr A] is a man who suffers from diabetes and had reported significant erectile dysfunction problems. With his medical history the most successful treatment for him is intracavernosal injection treatment.
When I met him on 25 January 2008 I advised him that this treatment was the only option really available to him, other than doing nothing or continuing with the oral medications which have been inconsistent in the past.
I explained to [Mr A] that if he was to proceed with the treatment then a test dose of the injectable treatment proposed would be required to be administered. He was provided with documentation including the consent form which warns of risks.
After administering the test dose [Mr A] reported a satisfactory outcome. I have noted his result as a 60–70% response.
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
I reviewed the results with him and in discussion with him recommended a slightly stronger dose than the one prescribed in the initial test dose. He was content with this.
Although the consent form was not signed and completed by [Mr A] at the time, I confirm it was provided to him.'
The clinical records — [Dr E].
An ‘initial consultation' consent form has been provided. This is unsigned.
An ‘Injectable treatments' consent form has been supplied. This is unsigned.
The ‘Medical history' form indicated that the concern of [Mr A] was in relation to ‘maintaining an erection'. His symptoms were of three years' duration and had not consistently responded to treatment with Viagra.
The history included note of diabetes of 6 months' duration. No note was made of any diabetic medication required or the state of control of the blood sugar levels.
Regular medications included atenolol, aspirin, lisinopril, simvastatin and amlodipine. All of these medications might be prescribed for ischaemic heart disease. No mention was made as to whether [Mr A] had this diagnosis or used nitrolingual spray for angina.
Allergies were not noted.
A test dose of prostaglandin injection into the penis was given at 1000 hours. The
form detailing this included advice to the doctor that ‘
Before proceeding with test
dose ensure that a CONSENT FORM has been understood and signed'. The form
was not signed. A test dose was given. The response was detailed as 60–70%.
Literature was given to describe the correct method of use of prostaglandin injection at home. Advice was also given regarding management of priapism, a recognised complication of intracorporeal injection.
Clinical advice
Erectile dysfunction in patients with diabetes is usually related to micro and macro vascular disease with impaired blood flow.
In my view an integral component of the management of a diabetic patient requesting erectile treatment would be history of the diabetes, including current control of hyperglycaemia and hyperlipidaemia. Unless these areas of management are controlled well, any improvement in erectile function can be expected to be short lived because control of further vascular disease is required to optimise erectile function. [Dr E] made no attempt to obtain history of the current diabetic
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
and cardiac status of [Mr A]. While the ongoing management of these conditions would remain the responsibility of the general practitioner an assessment of these matters was required in order to offer effective long term treatment. [Dr E] should also have examined the peripheral arteries in the groin and legs and examined for an abdominal bruit that might suggest arterial disease of the aorta. Such disease would affect the arterial supply to the penis. Vascular surgical advice may have been warranted.
Further, the particular list of medicines taken by [Mr A] suggested that he might also have the associated condition of ischaemic heart disease. This was important information to elicit before prescribing any treatment for erectile dysfunction. Some of these medications may also cause erectile dysfunction, as an unwanted side effect of their pharmacological actions. This possibility was not discussed.
History of the diabetes and degree of diabetic control was not explored. History of
any cardiac complications was not elicited. Ischaemic heart disease was likely,
given the medication list, and was relevant to proposed treatment for erectile
dysfunction. Consent forms were not signed. In particular, prostaglandin test
injection into the penis proceeded without signed consent.
The standard of care
fell well below an acceptable level.
Clinical examination of [Mr A] was not performed but was warranted. The
peripheral pulses and heart should have been examined, and pulse and blood
pressure recorded. The ‘Physical examination sheet' required blood pressure
recording for all patients on oral medications. [Mr A] was taking five listed
medications consistent with diabetes and cardiovascular disease but no blood
pressure or cardiovascular examination was undertaken. This was a
significant
departure from accepted standards of medical practice prior to the prescribing
of medication to such a patient.
Intracorporeal self injection can be a difficult technique to master and is subject to failure.
The standard that I have used in providing this advice is that of the New Zealand
Medical Council in their publication ‘Good medical practice'. The Council defines
good clinical care as including, amongst other factors, ‘adequately assessing the
patient's condition, taking account of the patient's history and his or her views and
examining the patient as appropriate'. They also recommend ‘referring the patient
to another practitioner when this is in the patient's best interests'. It is my view
that an inadequate history was taken and no clinical examination was documented
although this was required given the history of diabetes and prescribed
medications for possible cardiac disease. [Dr E] has stated ‘that I am proud of the
record that I have in terms of lack of any complaints and moreover, those of our
clinic. I have no doubt that my clinical competence standards, as well as those of
the clinic, are to the appropriate standards'.
It is my view that the care provided
by [Dr E] did not meet the standard set by the New Zealand Medical Council.
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
It is my impression that [Dr E] was functioning more as a prescriber of medicine rather than a doctor offering clinical assessment and examination.
[Dr E] has advised that some patients ‘will give me a clear impression that they do not want to get into discussion about risks and so forth. This involves something of a clinical judgement at the time'. It is my view that a doctor is more than just a source of prescription medicines. Where a patient is unwilling to provide reasonable information to substantiate a request for a specific treatment, a prudent doctor should refrain from prescribing such medication."
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
Appendix 3
Expert advice from Dr Stuart Tiller: Mr B
"Thank you for the request that I provide clinical advice in relation to specific questions posed regarding the care provided by [Dr E] to [Mr B] at the New Zealand Men's Clinic.
I have given earlier advice on 10th April 2008 in relation to this complaint.
Advice requested.
• General advice on the standard of care provided. • Specific advice on the standard of the clinical assessment/examination
• Specific advice on the clinical treatment prescribed and/or dispensed. • Whether any professional standards apply, and whether these standards were
• Any other comment.
Clinical advice
It is my view that the pre-consultation questionnaire completed by [Mr B]
canvassed necessary clinical history. However, as previously advised, [Mr B] did
not supply information in relation to any ‘other currently taken medications' or
‘allergies to medication'. It is my view that [Dr E] should have completed these
entries when reviewing the history with [Mr B] during the consultation. It is also
my view in relation to a young man complaining of ‘coming too soon' and
difficulty with ‘maintaining an erection' that further elaboration of these
complaints was required. Were these primary problems dating from the
commencement of sexual activity? Or were the problems secondary, after previous
satisfactory sexual experience? Was [Mr B] within a stable relationship where
discussion of sexual matters could take place? Was [Mr B] aware of ‘performance
anxiety'? There should have been some discussion regarding the need for adequate
sexual preparation prior to intercourse. In the absence of such detailed questioning
to establish the underlying cause of the perceived sexual inadequacy, any
treatment provided would be symptomatic only, and would not necessarily deal
with the underlying cause/causes of the sexual difficulties. Although I previously
advised that I thought the departure from standards of care were mild, upon
reflection
I would now consider that the care and advice offered by [Dr E], in
the context of a
specialist men's clinic dealing with issues of sexual
performance and satisfaction,
to have been a moderate departure from
accepted standards. It was important for a young man of the age of [Mr B], to
receive psychosexual advice and education in addition to any treatments on offer.
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
It is my view that a physical examination was not necessary in this particular case, although [Mr B] should have been asked if he held any concerns regarding his sexual organs and his ability to achieve satisfactory erections. If concern in this regard had been raised by [Mr B], then an examination should have been performed to ensure normal male sexual maturation.
[Dr E] has advised that the medication used, ‘is widely regarded as being safe as well as effective as an option to treat erectile dysfunction' by doctors working in this area of medicine. I am not in a position to comment upon this assertion. The use of clomipramine in a nasal delivery form is an unapproved use of a registered medicine. Clomipramine is traditionally used in tablet form for the treatment of depression and obsessive compulsive disorder. Some male patients taking oral clomipramine, for its registered indications, have reported retarded ejaculation, and this side effect is presumably the basis upon which the nasal delivery spray is used. I am unable to comment whether single intermittent use of clomipramine nasal spray is effective for retarding ejaculation where this is the desired outcome. [Dr E] has acknowledged that at the time of his treatment of [Mr B], he was not in the habit of advising his patients that the nasal delivery of clomipramine was an unapproved use of this medication. Since this complaint [Dr E] has updated the treatment consent form, which [Mr B] signed, to include the advice that nasal clomipramine is an unapproved presentation of clomipramine under the Medicines Act 1981. He has also ‘added nose bleeds as a rare side effect'.
The standard that I have used in providing this advice is that of the New Zealand Medical Council in their publication ‘Good medical practice'. The Council defines good clinical care as including, amongst other factors, ‘adequately assessing the patient's condition, taking account of the patient's history and his or her views and examining the patient as appropriate'. It is my view that [Dr E] did not adequately document that he had elaborated the clinical history of [Mr B] in order to address the psychosocial aspects of his sexual concerns. In this regard, medical students are taught that a good clinical history will provide in the region of 60% or more of the necessary information to make the correct diagnosis. The Code of Consumers Rights of the Health and Disability Commissioner would apply in relation to inadequate informed consent to an unapproved use of clomipramine in a spray formulation.
It is my view that the immediate onset of nasal bleeding upon the first use of clomipramine spray was likely a very rare and unexpected event. I note that the response from the New Zealand Men's Clinic to the complaint of [Mr B] was respectful and led to a refund of his expenses within one week. [Dr E] has advised that some patients ‘will give me a clear impression that they do not want to get into discussion about risks and so forth. This involves something of a clinical judgement at the time'. It is my view that a doctor is more than just a source of prescription medicines. Where a patient is unwilling to provide reasonable information to substantiate a request for a specific treatment, a prudent doctor should refrain from prescribing such medication."
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
Appendix 4
Expert advice from Dr Stuart Tiller: Mr C
"Thank you for the request that I provide clinical advice in relation to specific questions posed regarding the care provided by [Dr E] to [Mr C] at the New Zealand Men's Clinic.
Advice requested.
• General advice on the standard of care provided. • Specific advice on the standard of the clinical assessment/examination
• Specific advice on the clinical treatment prescribed and/or dispensed. • Whether any professional standards apply, and whether these standards were
• Any other comment.
The complaint
[Mr C] consulted with [Dr E] in Tauranga on 15 April 2008.
‘discussion of the problem and the options available and after rejecting an injection regime I was offered a nasal spray. I enquired about side effects and was told to expect some nausea but that was all. I had informed [Dr E] of my medical history including a triple bypass and aortic valve replacement.
I came home with some literature and a bottle of Apomorphine nasal spray.
I inhaled the spray, one squirt in each nostril at about 2.40pm. By 2.50pm. I had some mild vomiting and then collapsed on the floor. I passed out cold and came to almost three hours after the collapse.'
The next day [Mr C] spoke with [a clinic assistant], at the clinic. [The clinic assistant] advised him that ‘some people do have lowered blood pressure from using the spray but most continue using it and adjust to its use'.
[Mr C] advised that he did not wish to ‘chance it again'. He requested a refund of the cost. This was initially declined but after some strong representations ‘relented and made a refund of the cost of the medication'.
[Mr C] considers it ‘medical negligence if they know that the spray may lead to lowered blood pressure and do not inform people of that fact'.
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
The provider response — [Dr E]
[[Dr E] stated:]
‘[Mr C] says that he was only told about nausea as a side effect. This is not so. It is true that I explained to [Mr C] the most common of the unusual side effects is nausea and it occurs in perhaps 5% or so of patients. I expect this is why [Mr C] has remembered nausea being mentioned because I did specifically emphasise it as the most common of these unusual risks. I also routinely discuss with all of my patients receiving nasal spray, this would have included [Mr C] at the time, that in rare cases some cerebral interference can occur like drowsiness. I discuss this in layman's terms. The written material I gave [Mr C] and which he signed for refers to drowsiness.
[Mr C] in his letter of complaint, reports an immediate effect of mild vomiting with a subsequent collapse to the floor and being in a coma for some three hours. I, as above, have never heard of this being a response to this medication and I am extremely surprised for the reasons set out below, that this has happened. I cannot explain why this would be so. I can find no references in the medical literature that I have looked at that this is a known risk or one that has been experienced before.
I am very sorry that [Mr C] has had this reaction.
I do not believe it has been negligent on my part to prescribe the spray.
We have always treated his complaint as serious and have genuinely endeavoured to resolve matters with him. We did not hesitate to refund his fee.'
The clinical records — [Dr E].
[Mr C] signed an ‘initial consultation' form and an information sheet regarding ‘Apo-phen nasal spray'. These provided consent for the consultation and basic information regarding the apomorphine-phentolamine spray which was prescribed.
[Mr C] was aged 75 years and had a medical history which included coronary artery bypass surgery and aortic valve replacement.
The standard history form to be completed by [Mr C] prior to the consultation and to be discussed by [Dr E] during the consultation was incomplete.
Many questions related to past medical history, in particular alcohol use, smoking, prostate health, nitrolingual spray use and allergies were unanswered by [Mr C] and not completed by [Dr E] during the consultation. Cardiac medications were listed including Verapamil, Lipex, Enalapril, aspirin and Progout and Somac. There was no recording of the status of the ischaemic heart disease, whether [Mr C] currently suffered any angina or breathlessness, and no recording of pulse rate and rhythm, blood pressure or chest and heart auscultation.
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
[Mr C] had a history of previous abreaction to medication for sexual functioning, including Viagra and an injection which had proven ineffective.
The clinical records indicate that [Dr E] intended to prescribe testosterone cream and Apomorphine lozenges. [The] latter were to be taken as half tablet daily for 2 weeks then one prior to intercourse. Thirty lozenges were to be dispensed. But the consent form and medication invoice indicate that Apomorphine/phentolamine spray was dispensed.
Apomorphine
Medsafe data indicates that the optimal dosage of Apomorphine injection ‘has to be determined on an individual basis. Hospital admission under appropriate specialist supervision is advised when establishing a patient's therapeutic regime'.
[Dr E] has not advised what dosage of Apomorphine was used in the nasal spray. I can advise that nasal absorption would be rapid.
Recognised side effects include vomiting and somnolence.
[Dr E] has not provided evidence of pharmacological studies to indicate the safety, rate of absorption, and recommended dose range of Apomorphine by a nasal route.
New Ethicals compendium lists Phentolamine as a powerful vasoactive medication for use in hypertensive crises to rapidly lower blood pressure.
It is contraindicated where there is a history of coronary artery disease.
Phentolamine may augment the hypotensive effect of other anti-hypertensive agents. [Mr C] was taking Enalapril and Verapamil, both of which have hypotensive effects.
[Dr E] has not advised what dosage of Pentolamine was used in the nasal spray. I can advise that nasal absorption would be rapid.
[Dr E] has not provided evidence of pharmacological studies to indicate the safety, rate of absorption, and recommended dose range of Pentolamine by a nasal route.
Clinical advice
The pre-consultation questionnaire was incompletely answered by [Mr C]. [Dr E] did not ‘fill in the gaps' in the history in order to obtain a necessary and comprehensive clinical history prior to prescribing medication with significant effects upon the cardiovascular system. [Dr E] did not detail whether [Mr C] had stable heart disease or was using a nitrate spray for symptomatic angina. No clinical examination was made upon [Mr C] to establish his baseline blood
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
pressure on his usual medications prior to adding Phentolamine which is a
powerful hypotensive agent. It is my view that discussion with the cardiologist
was required before prescribing any agent to improve erectile function. The failure
of [Dr E] to provide studies to indicate the safety of Apomorphine-Phentolamine
nasal spray, could be interpreted to indicate irresponsible prescribing of two agents
with known powerful systemic effects.
It is my view that the standard of care
provided to [Mr C] was a severe departure from expected standards because
of the failure by [Dr E] to obtain an adequate medical history, the failure to
undertake any clinical examination or clarify the cardiological status of [Mr C],
and the prescribing of powerful medications, one of which was contraindicated in
known coronary artery disease. I note that the records of [Dr E] indicated that he
intended to prescribe Apomorphine lozenges, but Apomorphine-Phentolamine
spray was dispensed.
No clinical assessment was documented. No telephone consultation with the
cardiologist was undertaken. Both were mandatory actions in the given clinical
context of [Mr C's] known ischaemic heart disease.
These were serious
omissions in care.
It is my view that Phentolamine, in particular, was contraindicated. It is unclear whether the intended medication was dispensed by the clinic.
The standard that I have used in providing this advice is that of the New Zealand Medical Council in their publication ‘Good medical practice'. The Council define good clinical care as including, amongst other factors, ‘adequately assessing the patient's condition, taking account of the patient's history and his or her views and examining the patient as appropriate'. They also recommend ‘referring the patient to another practitioner when this is in the patient's best interests'. It is my view that an inadequate history was taken and no clinical examination was documented. Cardiological advice was also necessary.
[Dr E] has advised that some patients ‘will give me a clear impression that they do not want to get into discussion about risks and so forth. This involves something of a clinical judgement at the time'. It is my view that a doctor is more than just a source of prescription medicines. Where a patient is unwilling to provide reasonable information to substantiate a request for a specific treatment, a prudent doctor should refrain from prescribing such medication."
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
Appendix 5
Expert advice from Dr Stuart Tiller: Mr D
"Thank you for the request that I provide clinical advice in relation to specific questions posed regarding the care provided to [Mr D] by [Dr E] of the New Zealand Men's Clinic.
Advice requested.
• General advice on the standard of care provided.
• Specific advice on the standard of the clinical assessment/examination
• Specific advice on the clinical treatment prescribed and/or dispensed.
• Whether any professional standards apply, and whether these standards
were complied with.
• Any other comment.
The complaint.
The complaint has been prepared with the assistance of a Health and Disability advocate.
[Mr D] has complained regarding the cost of his treatment, the manner in which he was required to pay a large sum of money and the ineffectiveness of the treatment provided.
[Mr D] consulted with a doctor for about 30 minutes. At no time was cost of the proposed treatment mentioned.
At the reception desk he felt pressured to pay $710 immediately without time for reflection or discussion with his wife who was outside the clinic. Given the sensitive nature of his consultation he felt unable to dispute the demand for such a sum of money. He felt ‘bullied into paying'.
He believes that he was not given adequate prior information or time to consent to the proposed treatment and accept the expense involved.
The clinical records.
The ‘Initial consultation' consent form has been signed by [Mr D].
The ‘Injectable treatments' consent form has been signed by [Mr D].
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
The pre-consultation forms were completed by [Mr D] and indicated that his presentation was for difficulty ‘getting an erection'. The symptoms had been present for 1–3 years. Regular medication included Hytrin and synflex.
[Mr D] was aged 68 years.
The ‘Physical examination sheet' was left blank. This form indicated that for all
patients on oral medications the blood pressure ‘
must be done'. There was no
recording of blood pressure or pulse. There was no examination of the peripheral
pulses or any other area of the cardiovascular system.
A test dose of prostaglandin injection was given with a recorded 30% response.
Prostaglandin injections for home use were prescribed and dispensed.
The ‘injectable treatments' consent form signed by [Mr D] contained information regarding potential side effects of this treatment.
Clinical advice
It is my view that for a man of the age of [Mr D]
examination of the
cardiovascular system was required before recommending treatment for erectile
dysfunction with anticipated resumption of sexual activity to follow. The forms of
the clinic required the doctor to record the blood pressure. This was not done. No
examination of the peripheral pulses was undertaken to assess the state of the
arterial circulation. No enquiry was made regarding cholesterol levels. It is my
view that the
omission of any physical examination was a mild to moderate
departure from accepted standards for a medical practitioner. I acknowledge
that [Mr D] was an apparently fit and healthy man for his age of 68 years. There
was also no discussion of the possibility that Hytrin treatment might be
contributing to the erectile dysfunction. Impotence is listed in MIMS/New Ethicals
as a recognised adverse side effect of Hytrin medication. Doctors should always
consider long term medication as a possible cause of side effects and adverse
symptoms, such as erectile dysfunction.
See above comment.
The treatment offered and prescribed was reasonable.
The standard that I have used in providing this advice is that of the New Zealand Medical Council in their publication ‘Good medical practice'. The Council define good clinical care as including, amongst other factors, ‘adequately assessing the patient's condition, taking account of the patient's history and his or her views and examining the patient as appropriate'. The Council also recommends ‘referring the patient to another practitioner when this is in the patient's best interests'. It is my view that an adequate history was taken but no clinical examination was documented although this was required given the age of [Mr D].
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
[Dr E] has advised that some patients ‘will give me a clear impression that they do not want to get into discussion about risks and so forth. This involves something of a clinical judgement at the time'. It is my view that where a doctor is aware that a recommended course of treatment will be expensive, that some information in that regard should be provided by the prescribing doctor. [Mr D] has indicated that the doctor did not warn him of the expense to be incurred. [Dr E], however, has indicated that he ‘explained the cost for the treatment of intracavernosal injections, and that ‘[Mr D] appeared happy to proceed with the treatment'."
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
Appendix 6
Expert report from Dr Sean Wright
"My name is Dr Sean Wright. I am a medical practitioner registered in New South Wales. I currently work in a Sydney teaching hospital practicing anaesthetics. Prior to this position I worked for 7 years in the Men's Health area in which [Dr E] currently works. I have been asked to provide an opinion on the complaints brought against [Dr E] by Messrs [C, B, A and D] and to comment on the critique supplied by Dr Stuart Tiller. I shall deal with each complaint in turn, as set out below.
[Mr B] is a 22 year old male who presented to the clinic with a complaint of premature ejaculation. His clinical history was unremarkable and no clinical examination was performed. According to [Mr B] ‘a couple of options' were discussed with Clomipramine being recommended. Notes supplied by the clinic indicate [Mr B] signed a consent form outlining common side effects of clomipramine, he was also supplied with exercises designed to desensitize the penis. These exercises are included in the clinical record and referred to by [Mr B].
Clomipramine is commonly used to delay ejaculation. It is not a permanent cure. Premature ejaculation is overcome through desensitization; generally exercises of the stop/start type variety, or by continuing post ejaculatory stimulation with the aid of intracavernosal injections. [Dr E] quite rightly has chosen to avoid the possible long term use of injections in favour of simpler treatment. The treatment offered covered both a long term approach to correct the problem through exercises and a short term solution to alleviate the relationship difficulties in the interim. I find no issue with the proposed treatment. As premature ejaculation is purely subjective, from a physiological viewpoint it is not abnormal and in a reproductive sense even desirable. Therefore there are no relevant clinical findings and as such physical examination is unwarranted I find no issue with the lack of physical examination in this case.
Dr Tiller in his report has drawn attention to numerous facts re the patient's relationship history, performance anxiety, chronological onset of the condition etc. Whilst these psychosocial aspects would certainly have added to the history, they would have had no bearing on the case management at all. They are quite simply irrelevant in a case of premature ejaculation in a young healthy male with no erectile difficulty.
[Mr B's] complaint itself can be reduced to three factors. He was not informed that this was an unapproved use of the medication. He was not informed it was for depression/OCD in its approved use. He was not informed that epistaxis was a possible side effect.
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
I am not in a position to state whether it is a specific legal requirement to notify a patient of unapproved use of a medicine under New Zealand law. If this is the case, then [Dr E] is at fault. I understand this aspect has since been remedied and is now included in the consent form supplied to the patient.
We do not routinely inform patients of the alternative usages of medicines. Antidepressants, whilst developed for depression are commonly used for other psychiatric issues such as anxiety, as sedatives for insomnia and for chronic pain amongst others uses. How many patients receiving Viagra from their GP, (surely the accepted standard of care), are informed that this drug was developed for pulmonary hypertension? The use of a side effect of Clomipramine to treat PE is obviously a comparable situation.
Clomipramine (as Anafranil) in Australia carries a warning that 2% of patients will suffer epistaxis. The average starting dose is 25mg, maximum dosage is 200mg. There is no information given on the duration of treatment prior to onset of epistaxis, but I suspect it would necessitate ongoing usage. In my opinion epistaxis from a single low dose of Clomipramine, such as administered by a nasal spray, is likely to be extremely rare. I note further that epistaxis is not listed in the New Zealand version of MIMs drug compendium as a side effect of Clomipramine. [Dr E] could not reasonably be expected to know therefore of this possibility. I note that having been informed of such a possibility, clinic documents have been altered to address this issue.
This case, in my opinion, shows no significant departure from the relevant standards of care appropriate to the presenting complaint. The issues raised by [Mr B] re unapproved use and alternative uses of clomipramine are not of clinical significance. The failure to mention a side effect that MIMs also fails to mention, whilst regrettable, would be reproduced by any practitioner in New Zealand who utilizes MIMs and therefore cannot be termed substandard care.
[Mr A] is a 61 year old man suffering from erectile dysfunction. Co-morbidities include diabetes, hypertension and hyperlipidaemia. His regular medications are listed as Atenolol, Aspirin, Lisinopril, Simvastatin, Amlodipine. He denied ischaemic heart disease.
There are several issues in this case. I see these to be the examination and history taken, consideration of background co-morbidities in the context of the patient's complaint, suitability of the recommended treatment and the effectiveness of the recommended treatment.
[Mr A] has several conditions all of which can and probably are contributing to his erectile dysfunction. He certainly has microvascular damage due to hypertension, diabetes and hypercholesterolaemia. Erectile difficulties are also a side effect of anti hypertensive medications, particularly beta blockers.
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
Whilst Dr Tiller's opinion strictly speaking, is medically correct it overlooks the practicalities of this situation. Firstly the notes clearly indicate that heart disease was excluded in the patient history despite Dr Tiller's assertion to the contrary. There is no mention of the patient's current diabetic/lipid control, this does not mean it was not discussed merely that it was not recorded. Dr Tiller has correctly asserted that these are issues for the patient's regular GP and would be important in any long term prevention of erectile deterioration. This is undoubtedly true, however, in my experience a patient of this nature will not achieve any significant long term improvement regardless of treatment or glycaemic control. I agree with [Dr E's] assessment that intracavernosal injections are the only reliable treatment in the situation. I am not surprised that this patient had poor results with Viagra treatment previously. It is not appropriate for a clinic such as this to manage a patient's ongoing medical problems, these patients invariably are after a ‘quick fix solution' that will enable an erection on demand. The injections supplied are the only feasible alternative. [Mr A's] antihypertensives are certainly contributing to the problem. He is on triple therapy, strongly suggesting that he has refractory hypertension. It would be very unwise to alter his antihypertensives in an effort to alleviate his erectile problems. The possible sequelae could be devastating (eg stroke) compared to the benign nature of erectile difficulty. Injection therapy is the safest and most reliable option in this instance.
I agree with Dr Tiller's assertion that a physical examination should have been conducted, including peripheral pulses. The commissioner states that ‘I endorse Dr Tiller's view … that a vascular referral was warranted' this is a gross distortion of what Dr Tiller actually wrote ‘a vascular referral MAY have been warranted'. Erectile difficulty occurs in up to 50% of men over the age of 40. To suggest that all of these require a vascular referral is clearly incorrect. In the absence of any clinical indication, e.g bruit, palpable aneurysm or unequal pulses, such a referral IS NOT warranted. Unfortunately this examination was not performed. Nevertheless it is worth noting that in an elderly gentleman with significant co-morbidities, vascular surgery and the attendant risks would almost certainly be imprudent if the only symptom were erectile dysfunction. Medical therapy should always precede surgical treatment where possible. Whilst cardiac auscultation and blood pressure recording should be part of any thorough examination, and I would recommend they be done routinely, they would not alter the treatment in this case.
As regards the apparent ineffectiveness this is quite clearly a technique problem on the patient's part. It is inconceivable that the patient would receive a lesser effect with a higher dose at home than that achieved with a lower dose in the clinic. [Mr A] seems unable to appreciate this or unwilling to remedy his technical difficulties.
In summary, there are several instances here where history taking, physical examination and record keeping could have been more thorough. However, these factors would not materially alter the choice of treatment, which was the
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
appropriate one in this case. Nor would they affect the patient's long term welfare which is the responsibility of his primary GP.
I would recommend in future that whilst [Dr E] may be able to arrive at the appropriate conclusion swiftly, it would be prudent to take time to outline to the patient why other measures etc are not appropriate.
[Mr D] is a 69 year old gentleman who presented with erectile difficulties. Background history was unremarkable except for some prostatic hypertrophy treated with Hytrin.
[Mr D] has not in fact complained about his medical treatment. His complaint is purely fiscal and should probably therefore be directed at the clinic's manager not [Dr E]. I will however refer to Dr Tiller's opinion as provided. Examination of the cardiovascular system being a requirement before resumption of sexual activity arises from the belief that exercise in the previously sedentary may precipitate a coronary event. My understanding is that [Mr D] is a fit [businessman]. Presumably this involves some exercise and his tolerance of such would be sufficient for intercourse. Regardless, if one is to properly assess a patient's capacity for vigorous exercise, this would require a stress ECHO/ECG. Clinical examination in the GP rooms is of no help in this regard. I have already discussed the suitability of blood pressure recording and cardiac auscultation, and pulse checks in all patients routinely. I have also indicated that where injection therapy is the treatment of choice, these examinations serve only as a general check up, i.e. they do not alter treatment or outcomes. One should compare the thoroughness of [Dr E's] consultation with what would be expected from the average GP when a patient requests Viagra. I would suggest [Dr E] meets that minimum standard.
Hytrin could certainly be a contributing factor to [Mr D's] condition. However, urinary retention is a poor substitute for erectile dysfunction. I.e. one must take into account that the patient only wishes to have sex occasionally, whilst his prostatic hypertrophy, hypertension etc are ongoing. It is simply not practical in most cases to alter medications for other conditions in an attempt to alleviate erectile difficulty. Sometimes the patient's current regime has been arrived at after a very long process by the GP, addressing many issues and to unilaterally alter this regime is imprudent.
The treatment prescribed to [Mr D] was appropriate. It is unfortunate that [Mr D] did not have a good result He did however persevere for some months before complaining. I am unable to find significant medical care issues in this case.
[Mr C] is a 76 year old gentleman who presents with erectile dysfunction having previously used both Viagra and intracavernosal injections, neither of which he
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Health and Disability Commissioner
found effective. His background co-morbidities include hypertension, and ischaemic heart disease. He has had 3 vessel CABG and an aortic valve replacement (tissue not prosthetic). His medications include Verapamil, Lipex, Progout, Enalapril, Aspirin and Somac.
[Mr C] was recommended injection therapy which he refused. He was then prescribed a nasal spray. This then becomes quite confusing. The consent form is for
apomorphine/phentolamine sublingual tablets, which I understand were unavailable. [Dr E] avers that he prescribed only apomorphine and not phentolamine.
On taking the medication [Mr C] suffered what appears to be a severe hypotensive episode.
I would consider in this case that [Dr E's] history taking, note taking and examination to be inadequate. Previously I have mentioned that with injection therapy which is confined to the cavernosa that blood pressure recordings etc do not alter treatment or outcomes. This is true. It is not true when prescribing a systemically vasoactive oral or nasal medication. These medications have the potential to lower blood pressure, it is therefore prudent to know what the baseline pressure is. The patient's aortic valve (tissue) may be stenotic, which would reduce the patient's ability to increase cardiac output to compensate for hypotension. Failure to maintain adequate cardiac output in a patient with ischaemic heart disease could have serious consequences.
In my opinion there is insufficient history recorded as to the current cardiac status regarding angina, exercise tolerance etc. This does not mean it was not elicited, merely that it was not recorded. I am unable to comment which is the case. Similarly cardiac auscultation should have been used to assess degree of aortic stenosis and cardiac referral would be warranted if there were concerns on a clinical basis. I do not accept that a cardiologist referral/discussion is a mandatory standard of care as stated by Dr Tiller. Blood pressure should have been assessed.
Verapamil and Enalapril are both likely to potentiate the first dose effect of an alpha blocker such as phentolamine. This would produce a hypotensive episode such as that seen in [Mr C's] case. I would consider it imprudent to prescribe phentolamine in the presence of these other medications. There is some discrepancy as to what was prescribed and dispensed.
Apomorphine can also cause hypotension and its use in unstable coronary disease is not recommended. There are insufficient notes recording the status of [Mr C's] coronary disease to comment on the appropriateness of apomorphine here. It is recommended that oral Apomorphine use be initiated in a monitored hospital situation. I have no information on the pharmacodynamics of this nasal spray and cannot reliably comment therefore on how it is best initiated. Nausea is a common
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Opinion 08HDC02899, 08HDC05986, 08HDC07100, 08HDC09984
side effect of apomorphine. That [Mr C] suffered nausea immediately following administration and prior to his collapse, would indicate that the apomorphine absorption and dosage from a single spray is systemically significant. Nausea could also be a simple vasovagal result from hypotension secondary to phentolamine. Due to the uncertainty of the medication it is hard to say which drug was responsible only that either should be administered with great care in this patient. I would suggest that phentolamine is contraindicated here. I would be reluctant to prescribe apomorphine spray or lozenges until some pharmacodynamic studies are available.
In my opinion these medications were inappropriate for this patient. Injection therapy (dismissed by the patient) would have been more appropriate in this situation."
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
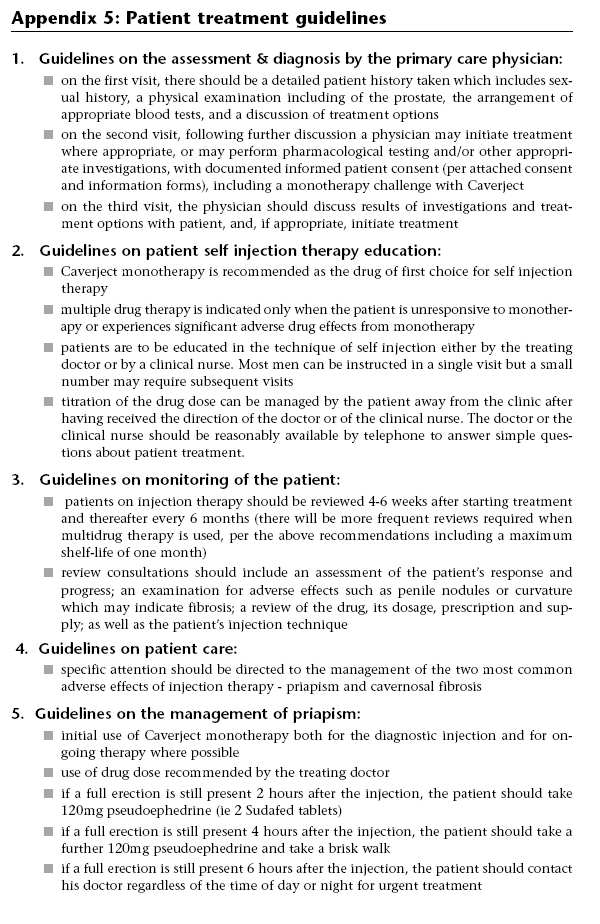
Health and Disability Commissioner
Appendix 7
New South Wales Impotence Inquiry Recommendations
18 December 2008
Names have been removed (except the NZ Men's Clinic) to protect privacy. Identifying letters are assigned in alphabetical order and bear no relationship to the person's actual name.
Source: http://www.hdc.org.nz/media/14218/08hdc02899,-07100,-05986,-09984.pdf
What is Aura-Soma? Other Colour Treatments Aura-Soma is a remarkable Colour Therapy System, based Full Spectrum Colour Healing on over a hundred vibrant dual-coloured bottles of ‘oil Uses the healing arts of intuitive and colour healing combined over water.' These natural oils are known as "Equilibriums" with the therapeutic use of the Aura-Soma chakra colours.
IATA Dangerous Goods Regulations 50th Edition (English) Effective 1 January 2009 ADDENDUM Posted 23 December 2008 Users of the IATA Dangerous Goods Regulations are asked to note the following amendments and corrections to the 50th Edition, effective from 1 January 2009. Where appropriate, changes or amendments to existing text have been highlighted (in yellow - PDF or grey - hardcopy) to help identify the change or amendment.