Mise en pages

The bioMérieux solution
Did you know?
VITEK2 has been challenged with ESBL in
http://www.lahey.org/studies
Site of Lahey Clinic, where tables are updated for
several studies.The broader scope has been
B-lactamases with amino-acid sequences
published by Livermore et al.
120 TEM
50 OXA
12 CMY
Multicentre Evaluation of the VITEK 2 Advanced Expert System for interpretive
reading of antimicrobial resistance tests.
6 VIM
Livermore et al. Journal of Antimicrobial Chemotherapy (2002) 49,289-30010 European centers results were compared final result to final
The study was performed by 10 European centers from nine different
The Hall Laboratory of Experimental Evolution
European countries, and involved around 1000 strains.
test agreement resistant
Klebsiella spp 99
E. cloacae, C. freundii
Identifying Resistance
E. gergoviae
total 137
bioMérieux UK jointly organised a symposium on
Klebsiella spp 5
Identifying Resistance, last February in London,
with the Public Health Laboratory Service (PHLS).
The only way to evaluate the performance of an expert system is to
One hundred and twenty people attended 8 lectures.
compare final results.
Here the comparison was made between results after interpretation by the expert system, and genotypic findings or human expert results
The first part of the meeting addressed the new
when using a phenotypic method (S.pneumoniae).
Health Organisation in this country (replacement ofthe PHLS by the Health Protection Agency (HPA)),
As a consequence, computation of results was similar to that of
bringing expertise and excellence to the National
Health Service (NHS), through a new organisation
• Agreement when both experts were giving the same result.
and a series of reference labs. The focus of the
• Disagreement when they differed.
presentations was epidemiology and microbiology
• Low discrimination when VITEK2 expert was proposing 2 or 3
answers, one of them being right.
and key speakers addressed the audience.
The second part of the meeting concerned the
control of antibiotics in hospitals, the role of themicrobiology laboratory in detecting resistance andhow this can aid infection control by more rapidreporting using VITEK®2.
In the final session, Dr David Livermore discussed
"Green cats" and the need for interpretive reading of antibiotic results. Dr Jean-Pierre Marcel frombioMérieux, concluded the meeting by discussing the company's experience in developing expert systems and the current developments in DNA Chip technology.
In the UK, authorities are working on Infection
Anne Beal,
Control and Resistance Detection based on the
Microbiology Laboratory Manager,
House of Lords white paper (Path to Least
(Fort Lauderdale, Florida)
resistance, 1998) and the Department of Health
surrounded by 4 VITEK® 2 XL
report "Getting ahead of the Curve", in order to
instruments at IntegratedRegional Laboratories (IRL).
reduce the Socio-Economic Burden of Hospital
This lab serves 13 hospitals in South Florida and
processes 2000 samples every day.
bioMérieux UK is closely supporting these official
VITEK 2 was chosen for routine use at this core lab facility
bodies, as was the case with this symposium.
because of its automation, rapid results and the AdvancedExpert System.
Did you know?
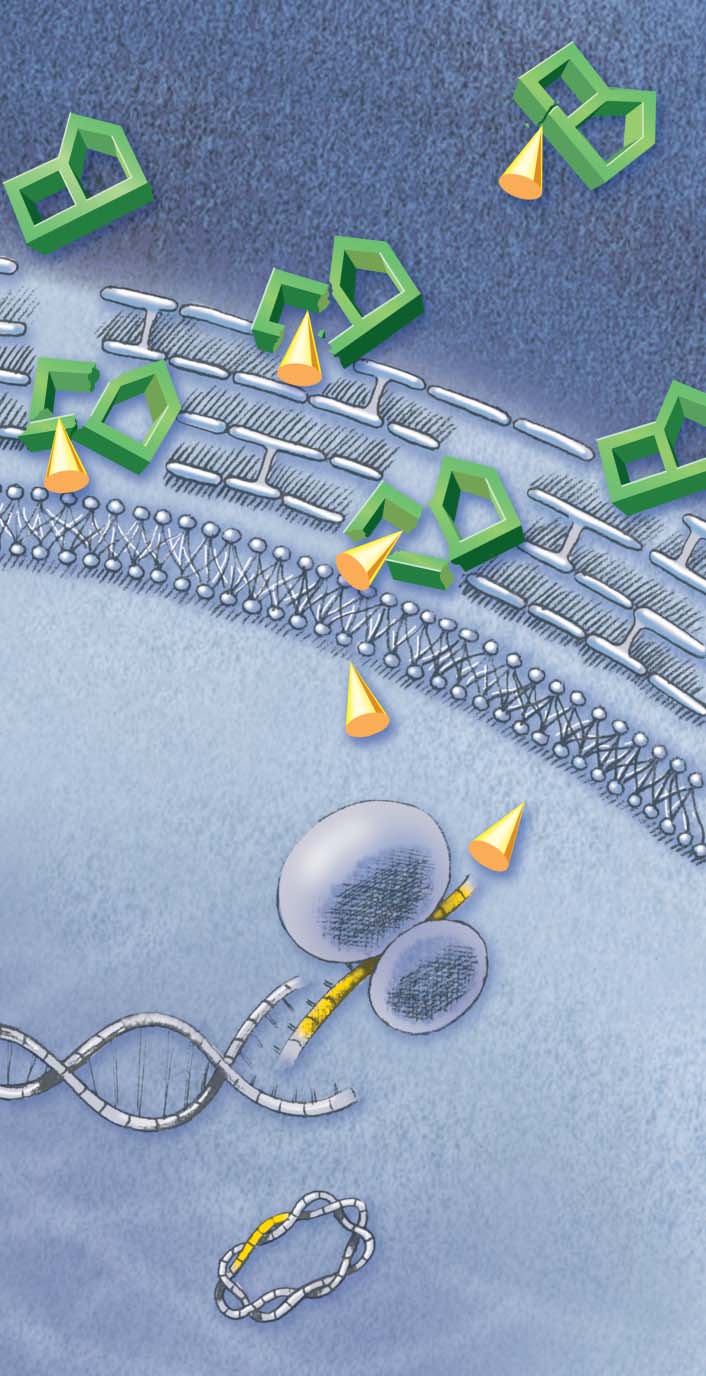
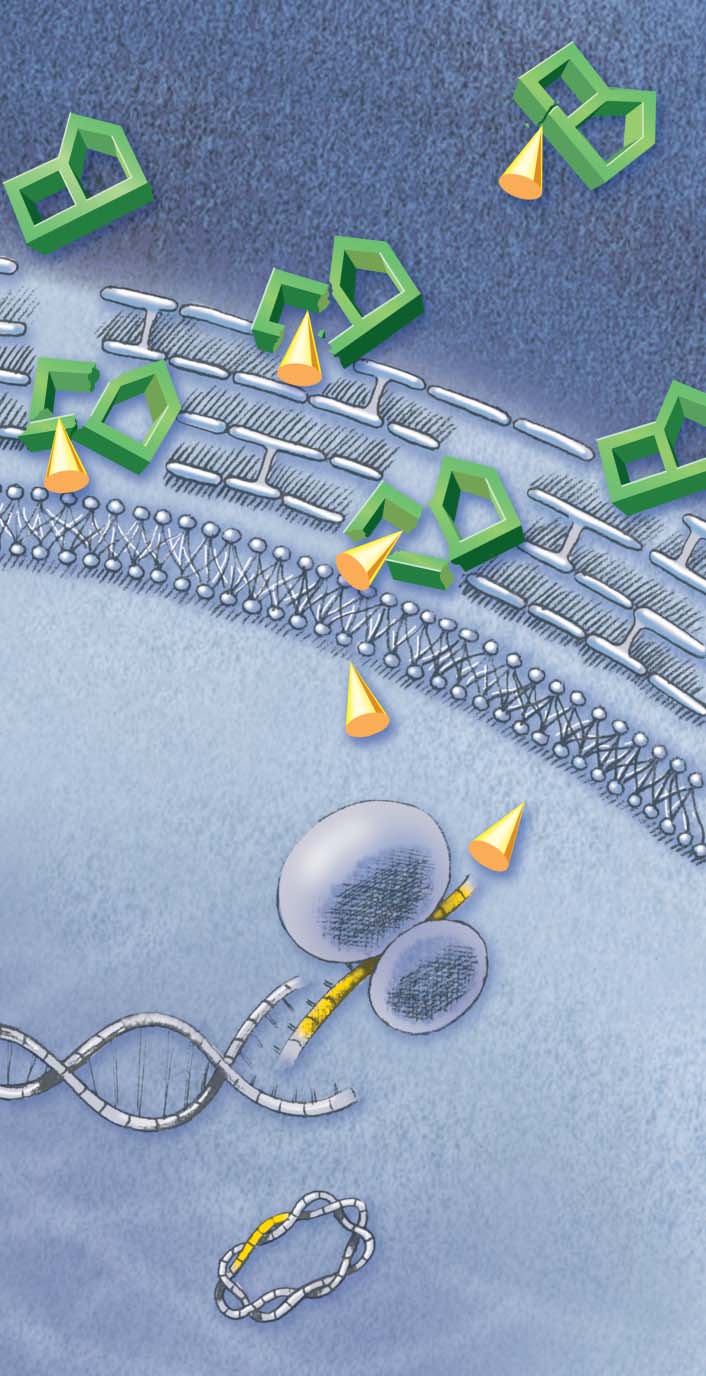
What is the impact of ESBL?
ESBL-producing bacteria escape treatment by
nccls recommendations
Cephalosporins, including widely used
ref: M100-S13 (M7) January 2003
Cephalosporins III and IV.
Table 2A Enterobacteriaceae
Comment 6
Why look for ESBL?
Strains of Klebsiella spp and E.coli that produce extended spectrum beta-lactamase (ESBLs) may be
Expression of ESBL production is variable in
clinically resistant to therapy with penicillins, cephalosporins, or aztreonam, despite apparent in vitro
intensity and with substrates. That means that
susceptibility to some of these agents.
Some of these strains will show MICs above the normal susceptible population but below the standard
the test result with a drug can be corrected
breakpoints for certain extended-spectrum cephalosporins or aztreonam. Such strains should be
when ESBL production has been demonstrated.
screened for potential ESBL production by using the ESBL screening breakpoints before reportingresults for penicillins, extended-spectrum cephalosporins, or aztreonam.
Other strains may test intermediate or resistant by standard breakpoints to one or more of these agents.
How to suspect an ESBL?
In all strains with ESBLs, the MICs for one or more of the extended-spectrum cephalosporins or
By testing several cephalosporins to contourn
aztreonam should decrease in the presence of clavulanic acid as determined in phenotypic
substrate specificity. Any non-susceptible result
confirmatory testing.
For all confirmed ESBL-producing strains, the test interpretation should be reported as resistant to all
for cefotaxime, ceftazidime, aztreonam or
penicillins, cephalosporins, and aztreonam.
cefpodoxime is a strong indication with some
The decision to perform ESBL screening tests on all urine isolated should be made on an institutional
basis, considering prevalence, therapy, and infection-control issues.
What is the reference method?
Screening and Confirmatory Tests for ESBLs in
Amplification then sequencing of resistant genes
Klebsiella pneumoniae, K.oxytoca, and Escherichia coli.
is the reference to identify mutations turning
Medium (CAMHB), antibiotic concentrations, standard broth dilution recommendations for inoculum,
incubation conditions, incubation length.
some ß-lactamases into ESBL.
Growth may indicate ESBL production.
Phenotypic confirmatory tests are more widely
Recommended drugs are:
used: restoration of ß-lactam activity by
cefpodoxime (4 µg/mL), ceftazidime, aztreonam, cefotaxime, ceftriaxone (1 µg/mL).
ß-lactamase inhibitors such as clavulanic acid.
These can be performed using the diffusion
method (double disk method) or dilution
Sub-classes of cephem (parenteral) class
cefazolin, cephalothin, cephapirin, cephradin
cephalosporins II
cefamandole, cefonicid, cefuroxim (sodium)
cephalosporins III
cefoperazone, cefotaxime, ceftazidime, ceftizoxime, ceftriaxone
What antibiotics to use for
cephalosporins IV
ne of its subsidiaries / Printed in F
cefmetazole, cefotetan, cefoxitin
Alternative drugs are mainly carbapenems
(imipenems, meropenem.) or combinations of
Cephalosporins I, II, III, IV are sometimes referred to as 1st, 2nd, 3rd, and 4th generation
ß-lactams with inhibitors of ß-lactamase or
Cephalosporins III and IV are also referred to as "extended-spectrum cephalosporins".
This does not imply activity against ESBL-producing gram-negative bacteria.
For all confirmed ESBL-producing strains, the test interpretation should be reported as resistant
for this antimicrobial class or subclass.
ves the right to modify specifications without noti
Extended spectrum ß-lactamase
ESBL + impermeability (cephamycins)
INTERNATIONAL NEWSLETTER
ITEK are registered and protected trademarks belonging to bioMérieux s
Director of publications : Thierry Bernard
for more information : [email protected]
bioMérieux sa69280 Marcy l'EtoileFrance
9003E / This document is not legally binding. bioMérieux reser
Tel. (33) 04 78 87 20 00
Fax (33) 04 78 87 20 90
bioMérieux, blue logo, Identifying Resistance and V


n° 4 • December 2003
Did you know?
IDENTIFYING RESISTANCE Newsletter,
bioMérieux's ambition is to contribute to
■ What is the impact
the awareness and progress in the field
of resistance to antibiotics.
■ Why look for ESBL?
I hope the information, papers written
■ How to suspect
by worldwide specialists, brings you
valuable data to help you in your
reference method?
activities and day-to-day practice.
■ What antibiotic
This new issue deals with a complex
resistance mechanism that appeared
less than twenty years ago and for
which bioMérieux rapidly adapted its
offer of tests and software.
This is a perfect illustration of our
commitment and continuous effort to
bring you a global offer in terms of
instruments, reagents, software and
in Enterobacteriaceae
expert systems.
We will do our best to deserve your
confidence and continue to propose
Karen Bush, Ph.D., is the Team Leader for the Biology Antimicrobial
innovative new products to help you in
Agents Research Team at Johnson & Johnson Pharmaceutical Research &
your endeavour.
Development (Raritan, NJ, USA), where she is responsible formicrobiology research in Drug Discovery. Her work on beta-lactamase
Dr. Benoît Adelus
inhibitors and resistance mechanisms contributed to proposing an
Chief Executive Officer
updated functional classification scheme for these enzymes.
Karen Bush
Development of the "third generation"
its single amino acid variant TEM-2, and
cephalosporins in the early 1980s was
the functionally similar SHV-1 enzyme,
based heavily on the ability of these agents
together with the oxacillin-hydrolyzing
to escape hydrolysis by all the common
OXA-1 enzyme, were the most common
ß-lactamases in both Gram-positive and
plasmid-encoded ß-lactamases in Gram-
Gram-negative bacteria (18). Broad n e g a t i v e b a c t e r i a a c c o r d i n g t o
spectrum ß-lactamases with the ability to
epidemiological surveys in the 1980s
hydrolyze the most common penicillins
(13). However, the new cephalosporins,
and cephalosporins had been identified in
cefotaxime, ceftazidime and ceftriaxone,
virtually all species of Enterobacteriaceae
and the monobactam aztreonam exhibited
before 1980 (19), and had begun to
good antibacterial activity against Gram-
appear in large numbers of Haemophilus
negative bacilli, in part because of their
influenzae and Neisseria gonorrhoeae
exceptional stability to the infamous TEM,
isolates (2). The broad spectrum TEM-1,
SHV and OXA enzymes (6).
Identifying Resistance International Newsletter • December 2003
the seeds of better health
ESBL in Enterobacteriaceae
To the dismay of their developers, these
Coincidentally, the first ESBL-producing
agents were challenged by an unexpected
K. pneumoniae isolates from the United
set of mutational events shortly after their
States were all identified during the first six
introduction into clinical medicine. The first
months of 1987 in Boston, New York City,
extended spectrum ß-lactamases (ESBLs)
Chicago and California, but with a
were reported from Germany in 1983 with
ceftazidime-resistant phenotype (8, 14,
the description of three independent
15, 20). In all cases, the producing
K. pneumoniae isolates from the same
organisms were multidrug resistant due to
hospital exhibiting transferable cefotaxime
large plasmids that usually included
resistance (10). Retrospectively, an even
aminoglycoside resistance determinants as
earlier Argentinian K. pneumoniae isolatewas later shown to produce an ESBL in
well as ß-lactamase genes.
1982, the year after the introduction of
Phenotypically, a double disk diffusion
cefotaxime in the Americas (12).
Major outbreaks of ESBL-producing
amoxicillin-clavulanic acid was used to
Enterobacteriaceae were first reportedfrom France, where 283 cefotaxime-
identify the presence of early ESBLs in
resistant K. pneumoniae isolates were
E. coli and K. pneumoniae (9). The fact
detected from 1984 through June 1987, in
that ESBLs respond to inhibition by either
addition to another 200 isolates of E. coli,
clavulanic acid or tazobactam has served
Enterobacter spp., Serratia marcescens,
as a distinguishing characteristic of these
K. oxytoca and Citrobacter freundii that
enzymes throughout their history (6) and
produced the same ESBL (16).
is the basis of the NCCLS protocol for
detection of ESBLs in E. coli and
K. pneumoniae (17).
Characteristics of ESBLs
Data compiled from http://www.lahey.org/studies/webt.stm. (February, 2003).
Enzyme family
Total number in family
73 TEM-1 variants
32 SHV-1 variants
19 TEM-2 variants*
13 SHV-2 variants*
7 OXA-10 variants
Amino acids in enzyme,
including leadersequenceNumber of amino acid
positions at which
may differ 20-25%
substitutions have beenreported from enzymesin clinical isolatesMaximum number of
mutations in a singleESBL comparedto parentMost common
OXA-10 series: I10T, G20S, T110S,
substitutions in mature
R164S or R164H(N=25)
G238S or G238A (N = 17)
Y184F, E240G, S258S,
*TEM-1 and TEM-2, differing by a Q39K substitution are not considered to be ESBLs. SHV-1 differs from SHV-2 by a G238S substitution, rendering SHV-2 an ESBL.
#Each substitution appears in 3 enzymes. Different combinations are observed.
States, almost all the early ESBLs were
identified as TEM variants, whereas in
Europe a mixture of TEM and SHV ESBLs
were characterized (12).
Comparisons of the geographically diverseESBLs indicated that two distinct ESBLpopulations were evident. In Europe, oneset of enzymes showed preferentialhydrolysis of cefotaxime compared toceftazidime and were initially named "CTX"enzymes; a second set of enzymespreferentially hydrolyzed ceftazidime andwere named "CAZ" enzymes. However,upon sequencing of the producing genes,it was noted that both sets of enzymeswere derived from the blaTEM-1 gene.
Thus, an early consensus was reached in
the ß-lactamase community that the
ESBLs would be numbered according to
their parent, and not according to their
functional status (5). ESBL nomenclature
is currently being monitored on a website
managed by G. A. Jacoby and K. Bush
(http://www.lahey.org/studies/webt.stm),
where amino acid sequences and
literature references are provided for
all TEM and SHV variants, and for
OXA-derived ESBLs (see Table). In
addition, references are given for all OXA,
CMY-type, IMI-type and CTX-M sequences.
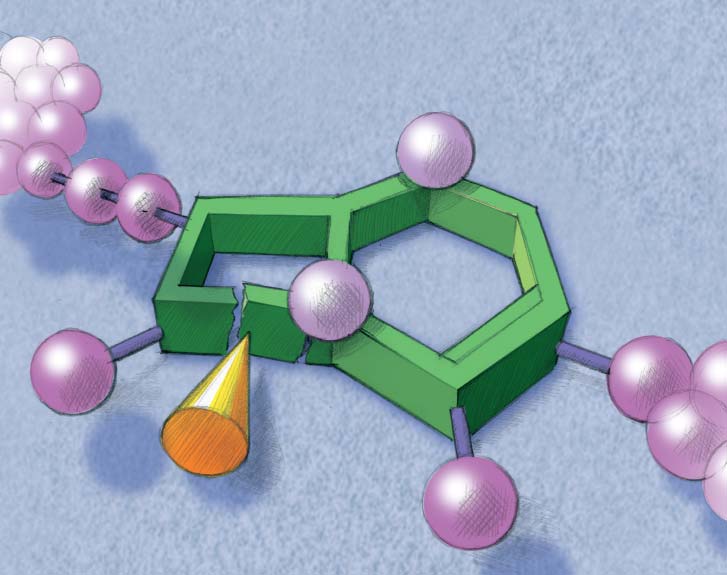
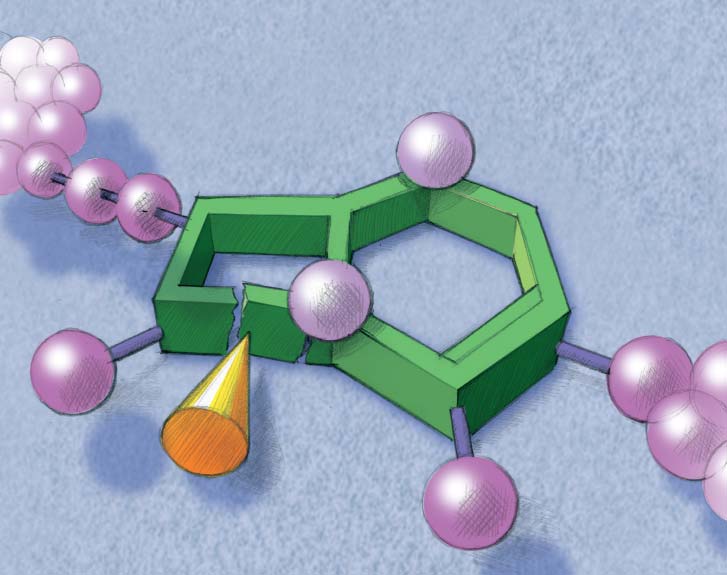
Resistance by ESBL:
enzymatic inactivation
Of assistance to the practicing laboratory
enzymologist is a table of all isoelectricpoints reported for all ESBLs.
Although the majority of ESBLs areassociated with either a TEM or SHVheritage, other enzyme families haveachieved recognition as they become
As improved molecular techniques
predominant in their own geographical
became more widely available in the
niches. Extended spectrum OXA-derived
1990s, sequencing of the responsible
enzymes were originally reported in
genes became routine and is considered
Pseudomonas aeruginosa isolates from
to be the "gold standard" for ESBL
Turkey (7) and have now been identified
identification (2). The original ESBLs from
from other European sites (2).
Europe and the United States were allderived from the common TEM-1 andSHV-1 enzymes, usually differing by one to
One of the most rapidly growing new
three amino acid substitutions compared
families of ESBLs is the CTX-M family,
to the parent enzyme. In almost all cases,
CTX-M-1 was first identified in cefotaxime-
these changes were due to point mutations
resistant K. pneumoniae isolates from
in the nucleotide sequences. In the United
Western Europe; CTX-M-2 was then found
Bauernfeind, A., I. Stemplinger, R. Jungwirth, S. Ernst, and J. M.
Casellas. 1996. Sequences of ß-lactamase genes encoding CTX-M-1(MEN-1) and CTX-M-2 and relationship of their amino acidsequences with those of other ß-lactamases. Antimicrob. AgentsChemother. 40:509-513.
Bradford, P. A. 2001. Extended-spectrum ß-lactamases in the 21stcentury: characterization, epidemiology, and detection of thisimportant resistance threat. Clin. Microbiol. Rev. 14:933-951.
in several South American isolates and
In addition, it is important to note that
differed by 16% in its amino acid sequence
Brenwald, N. P., G. Jevons, J. M. Andrews, J. H. Xiong, P. M.
Hawkey, and R. Wise. 2002. An outbreak of a CTX-M-type
from CTX-M-1 (1). These enzymes
Enterobacteriaceae, with their production
ß-lactamase-producing Klebsiella pneumoniae: the importance of
strongly prefer cefotaxime as a substrate
often masked by the concurrent
using cefpodoxime to detect extended-spectrum ß-lactamases.J.
Antimicrob. Chemother. 51:195-196.
and hydrolyze ceftazidime poorly.
production of AmpC cephalosporinases
Bush, K. 2001. ß-lactamases in gram-negative bacteria: diversity
(4). With the promiscuous transfer of
and impact on the selection of antimicrobial therapy. Clin. Infect.
At this time there are over 25 unique
ESBL determinants among Gram-negative
Dis. 32:1085-1089.
members of this family. It is regarded as
rods, we can only expect these enzymes
Bush, K., and G. Jacoby. 1997. Nomenclature of TEM
to continue to proliferate in the present
ß-lactamases. J. Antimicrob. Chemother. 39:1-3.
the most prominent ESBL in SouthAmerica, and has now been identified with
Bush, K., G. A. Jacoby, and A. A. Medeiros. 1995. A functionalclassification scheme for ß-lactamases and its correlation with
outbreaks in China and the United
molecular structure. Antimicrob. Agents Chemother. 39:1211-
Kingdom (3). The producing organisms
do not appear to be resistant to
Hall, L. M. C., D. M. Livermore, D. Gur, M. Akova, and H. E.
Akalin. 1993. OXA-11, an extended spectrum variant of OXA-10
ceftazidime in standard susceptibility
(PSE-2) ß-lactamase from Pseudomonas aeruginosa. Antimicrob.
testing, so detection systems utilizing only
Agents Chemother. 37:1637-1644.
ceftazidime will not identify a CTX-M ESBL
Jacoby, G. A., A. A. Medeiros, T. F. O'Brien, M. E. Pinto, and H.
(3). As additional families of enzymes
Jiang. 1988. Broad-spectrum, transmissible ß-lactamases [letter].
N. Engl. J. Med. 319:723-723.
continue to be identified, it may be
Jarlier, V., M. Nicolas, G. Fournier, and A. Philippon. 1988.
expected that even more narrow spectrum
Extended broad-spectrum ß-lactamases conferring transferable
ESBLs will become prevalent.
resistance to newer ß-lactam agents in Enterobacteriaceae:Hospital prevalence and susceptibility patterns. Rev. Infect. Dis.
10:867-878.
10. Knothe, H., P. Shah, V. Krcmery, M. Antal, and S. Mitsuhashi.
1983. Transferable resistance to cefotaxime, cefoxitin,cefamandole and cefuroxime in clinical isolates of Klebsiella
K. pneumoniae is often attributed solely
pneumoniae and Serratia marcescens. Infection 11:315-317.
to ESBL production; however, other
Livermore, D. 1995. ß-lactamases in laboratory and clinical
factors must also be considered.
resistance. Clin. Microbiol. Rev. 8:557-584.
12. Medeiros, A. A. 1997. Evolution and dissemination of
ß-lactamases accelerated by generations of ß -lactam antibiotics.
The combined contributions of porin
Clinic. Infect. Dis. 24(Suppl. 1):S19-45.
mutations, quantity of enzyme activity, and
13. Medeiros, A. A. 1989. Plasmid-determined ß-lactamases.
number of ß-lactamases per strain (4, 11)
Handbook of Experimental Pharmacology (91):101-127.
will result in elevated MICs for these
14. Naumovski, L., J. P. Quinn, D. Miyashiro, M. Patel, K. Bush, S. B.
Singer, D. Graves, T. Palzkill, and A. M. Arvin. 1992. Outbreak ofceftazidime resistance due to a novel extended-spectrumß-lactamase in isolates from cancer patients. Antimicrob.
Agents Chemother. 36(9):1991-1996.
15. Quinn, J. P., D. Miyashiro, D. Sahm, R. Flamm, and K. Bush.
1989. Novel plasmid-mediated ß-lactamase (TEM-10) conferring
selective resistance to ceftazidime and aztreonam in clinical
Enzymatic
isolates of Klebsiella pneumoniae. Antimicrob. Agents
16. Sirot, J., C. Chanal, A. Petit, D. Sirot, R. Labia, and G. Gerbaud.
1988. Klebsiella pneumoniae and other Enterobacteriaceae producing novel plasmid-mediated ß -lactamases markedly activeagainst third-generation cephalosporins: Epidemiologicalstudies. Rev. Infect. Dis. 10:850-859.
17. National Committee for Clinical Laboratory Standards. 2003.
Performance standards for antimicrobial susceptibility testing.
NCCLS approved standard M100-S13 (M7). National Committeefor Clinical Laboratory Standards, Wayne, PA.
18. Sykes, R. B., and K. Bush. 1983. Interaction of new cephalosporins
with ß-lactamases and ß-lactamase-producing Gram-negativebacilli. Rev. Infect. Dis. 5 Suppl. 2:S356-S366.
19. Sykes, R. B., and M. Matthew. 1976. The ß-lactamases of gram-
negative bacteria and their role in resistance to ß -lactam antibiotics.
J. Antimicrob. Chemother. 2:115-157.
20. Urban, C.,K. S. Meyer, N. Mariano, J. J. Rahal, R. Flamm, B. A.
Rasmussen and K. Bush. 1994. Identification of TEM-26ß-lactamase responsible for a major outbreak of ceftazidimeresistant Klebsiella pneumoniae. Antimicrob.
Agents Chemother. 38:392-395.
Source: http://www.biomerieux.com.tr/upload/IRN4_esbl4.pdf
37412_SpanishCover:37412_SpanishCover 9/17/09 10:37 AM Page 1 Publicado por la American Society for Reproductive Medicine, bajo la dirección del Comité de Educación del Paciente y el Comité de Publicaciones. Ninguna parte en este documento puede ser reproducida en ninguna forma sin permiso por escrito. Este folleto no pretende de ninguna manera sustituir, dictar ni definir
Monitoring the situation of children and women Multiple Indicator Cluster Survey SUMMARY REPORT Federal Republic of Nigeria National Bureau of Statistics MICS Nigeria, 2011 Summary Report In Memory This report is dedicated to the 24 people killed, and those who were injured, by the bomb attack on UN House in Abuja on the 26th August 2011. Amongst the people who lost their lives was Johnson Awotunde who devoted his time, energy and personal resources to the success of the survey until his untimely departure.